Abstract
AIMS—The reliability of scanning laser ophthalmoscope (SLO) microperimetry in differentiating full thickness macular holes from macular pseudoholes and impending macular holes was evaluated. METHODS—106 eyes with the clinical diagnosis of full thickness macular holes, macular pseudoholes, and impending (stage 1) macular holes were examined for the presence of deep or relative scotoma using SLO microperimetry. The relation between these scotomas and the clinical diagnosis was studied. RESULTS—Deep and relative scotomas were detected in all 57 eyes with clinically defined full thickness macular holes. In contrast, among 49 eyes diagnosed with macular pseudoholes or impending macular holes, no deep and only one relative scotoma was observed. The sensitivity of the presence of a deep scotoma as an indicator of the clinical diagnosis of a full thickness macular hole was 100% (57 of 57), and the specificity was 100% (49 of 49). The sensitivity of the presence of a relative scotoma was 100% (57 of 57) and the specificity was 98.0% (48 of 49). CONCLUSION—With SLO microperimetry, full thickness macular holes can be precisely and objectively distinguished from other conditions that mimic macular holes.
Full Text
The Full Text of this article is available as a PDF (140.5 KB).
Figure 1 .
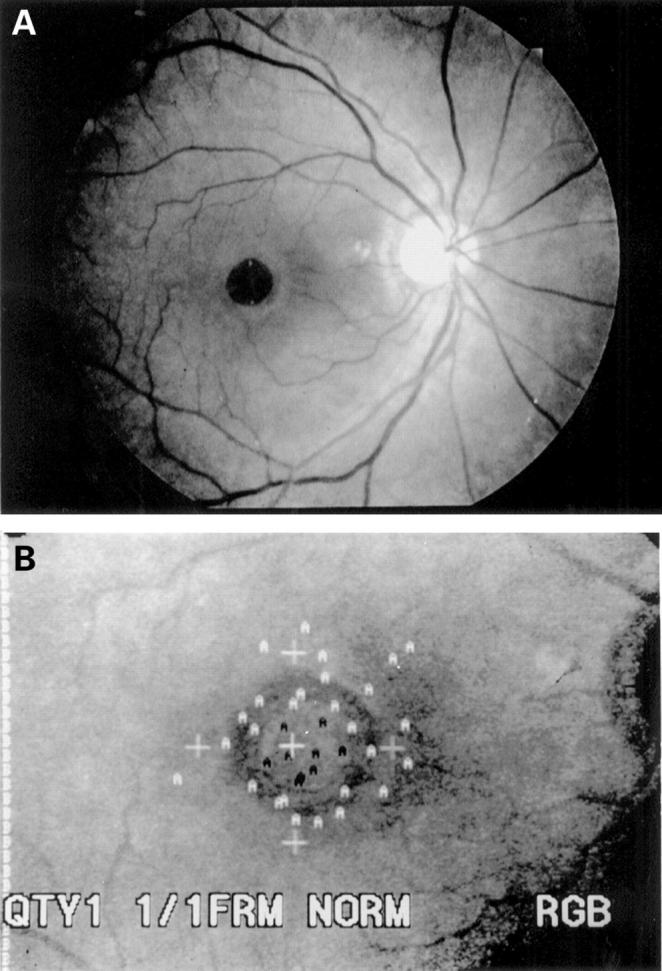
(A) Fundus photograph of a patient with a full thickness macular hole. (B) Scanning laser ophthalmoscope microperimetry with a 0 dB stimulus from the same patient. The white `A's indicate points seen by the patient, and black `A's correspond to points not seen (deep scotoma). Deep scotoma points were detected within the hole.
Figure 2 .
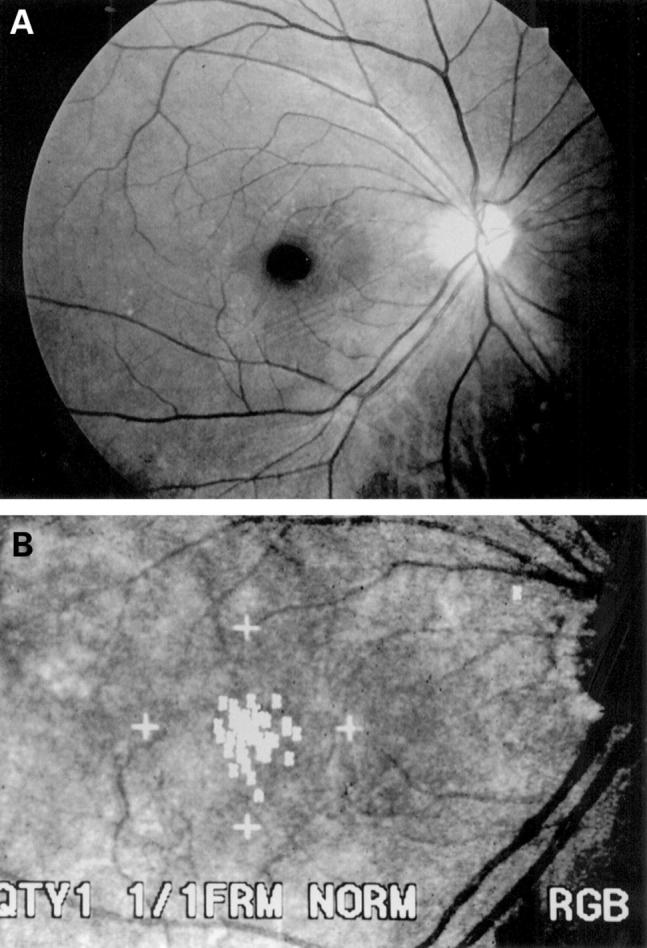
(A) Fundus photograph of a patient with a macular pseudohole. (B) Scanning laser ophthalmoscope microperimetry with a 10 dB stimulus from the same patient. A relative scotoma was not detected.
Figure 3 .
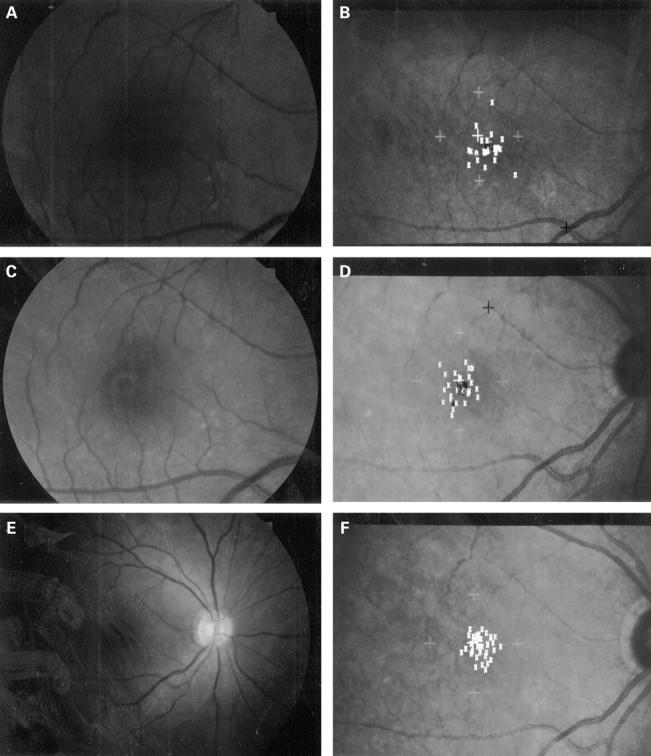
Fundus photograph and scanning laser ophthalmoscope (SLO) microperimetry of case 1. A 50-year-old woman presented with a 5 day history of visual loss in her right eye. The initial diagnosis was an impending macular hole. (A) Fundus photograph at presentation. Her best corrected visual acuity was 20/30. (B) Scanning laser ophthalmoscope microperimetry with a 10 dB stimulus at presentation. The white `K's indicate points seen by the patient, and black `K's correspond to points not seen. There is a relative scotoma at the nasal border of the macular hole. (C) Fundus photograph taken 2 months later. Her best corrected visual acuity had dropped to 20/50. The hole had enlarged and the cuff of subretinal fluid surrounding the hole had increased in size. (D) SLO microperimetry performed at that time shows extension of the scotoma to the nasal side of the hole. (E) Fundus photograph of the patient taken 1 month after vitrectomy and gas injection. The hole was closed anatomically. (F) SLO microperimetry recorded 1 month postoperatively. The scotoma had disappeared.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Acosta F., Lashkari K., Reynaud X., Jalkh A. E., Van de Velde F., Chedid N. Characterization of functional changes in macular holes and cysts. Ophthalmology. 1991 Dec;98(12):1820–1823. doi: 10.1016/s0161-6420(91)32044-x. [DOI] [PubMed] [Google Scholar]
- Allen A. W., Jr, Gass J. D. Contraction of a perifoveal epiretinal membrane simulating a macular hole. Am J Ophthalmol. 1976 Nov;82(5):684–691. doi: 10.1016/0002-9394(76)90002-7. [DOI] [PubMed] [Google Scholar]
- Bischoff P., Lang J., Huber A. Macular sparing as a perimetric artifact. Am J Ophthalmol. 1995 Jan;119(1):72–80. doi: 10.1016/s0002-9394(14)73816-4. [DOI] [PubMed] [Google Scholar]
- Chambers R. B., Davidorf F. H., Gresak P., Stief W. C., 4th Modified vitrectomy for impending macular holes. Ophthalmic Surg. 1991 Dec;22(12):730–734. [PubMed] [Google Scholar]
- Fish R. H., Anand R., Izbrand D. J. Macular pseudoholes. Clinical features and accuracy of diagnosis. Ophthalmology. 1992 Nov;99(11):1665–1670. [PubMed] [Google Scholar]
- Gass J. D. Idiopathic senile macular hole. Its early stages and pathogenesis. Arch Ophthalmol. 1988 May;106(5):629–639. doi: 10.1001/archopht.1988.01060130683026. [DOI] [PubMed] [Google Scholar]
- Gass J. D., Joondeph B. C. Observations concerning patients with suspected impending macular holes. Am J Ophthalmol. 1990 Jun 15;109(6):638–646. doi: 10.1016/s0002-9394(14)72431-6. [DOI] [PubMed] [Google Scholar]
- Gass J. D. Reappraisal of biomicroscopic classification of stages of development of a macular hole. Am J Ophthalmol. 1995 Jun;119(6):752–759. doi: 10.1016/s0002-9394(14)72781-3. [DOI] [PubMed] [Google Scholar]
- Guyer D. R., Green W. R., de Bustros S., Fine S. L. Histopathologic features of idiopathic macular holes and cysts. Ophthalmology. 1990 Aug;97(8):1045–1051. doi: 10.1016/s0161-6420(90)32465-x. [DOI] [PubMed] [Google Scholar]
- Hikichi T., Yoshida A., Akiba J., Konno S., Trempe C. L. Prognosis of stage 2 macular holes. Am J Ophthalmol. 1995 May;119(5):571–575. doi: 10.1016/s0002-9394(14)70214-4. [DOI] [PubMed] [Google Scholar]
- Johnson R. N., Gass J. D. Idiopathic macular holes. Observations, stages of formation, and implications for surgical intervention. Ophthalmology. 1988 Jul;95(7):917–924. doi: 10.1016/s0161-6420(88)33075-7. [DOI] [PubMed] [Google Scholar]
- Kelly N. E., Wendel R. T. Vitreous surgery for idiopathic macular holes. Results of a pilot study. Arch Ophthalmol. 1991 May;109(5):654–659. doi: 10.1001/archopht.1991.01080050068031. [DOI] [PubMed] [Google Scholar]
- Madreperla S. A., McCuen B. W., 2nd, Hickingbotham D., Green W. R. Clinicopathologic correlation of surgically removed macular hole opercula. Am J Ophthalmol. 1995 Aug;120(2):197–207. doi: 10.1016/s0002-9394(14)72608-x. [DOI] [PubMed] [Google Scholar]
- Mandelcorn M. S., Lipton N. Epi-macular holes: a cause of decreased vision in the elderly. Can J Ophthalmol. 1977 Jul;12(3):182–187. [PubMed] [Google Scholar]
- Martinez J., Smiddy W. E., Kim J., Gass J. D. Differentiating macular holes from macular pseudoholes. Am J Ophthalmol. 1994 Jun 15;117(6):762–767. doi: 10.1016/s0002-9394(14)70319-8. [DOI] [PubMed] [Google Scholar]
- Morgan C. M., Schatz H. Idiopathic macular holes. Am J Ophthalmol. 1985 Apr 15;99(4):437–444. doi: 10.1016/0002-9394(85)90011-x. [DOI] [PubMed] [Google Scholar]
- Morgan C. M., Schatz H. Involutional macular thinning. A pre-macular hole condition. Ophthalmology. 1986 Feb;93(2):153–161. doi: 10.1016/s0161-6420(86)33767-9. [DOI] [PubMed] [Google Scholar]
- Schneider U., Kuck H., Inhoffen W., Kreissig I. Funduskontrollierte Mikroperimetrie mit dem Scanning-Laser-Ophthalmoskop bei Makulaerkrankungen. Klin Monbl Augenheilkd. 1993 Sep;203(3):212–218. doi: 10.1055/s-2008-1045670. [DOI] [PubMed] [Google Scholar]
- Sjaarda R. N., Frank D. A., Glaser B. M., Thompson J. T., Murphy R. P. Assessment of vision in idiopathic macular holes with macular microperimetry using the scanning laser ophthalmoscope. Ophthalmology. 1993 Oct;100(10):1513–1518. doi: 10.1016/s0161-6420(93)31448-x. [DOI] [PubMed] [Google Scholar]
- Smiddy W. E., Gass J. D. Masquerades of macular holes. Ophthalmic Surg. 1995 Jan-Feb;26(1):16–24. [PubMed] [Google Scholar]
- Smiddy W. E., Michels R. G., Glaser B. M., de Bustros S. Vitrectomy for impending idiopathic macular holes. Am J Ophthalmol. 1988 Apr 15;105(4):371–376. doi: 10.1016/0002-9394(88)90300-5. [DOI] [PubMed] [Google Scholar]
- Smiddy W. E., Michels R. G., Green W. R. Morphology, pathology, and surgery of idiopathic vitreoretinal macular disorders. A review. Retina. 1990;10(4):288–296. doi: 10.1097/00006982-199010000-00012. [DOI] [PubMed] [Google Scholar]
- Van de Velde F. J., Timberlake G. T., Jalkh A. E., Schepens C. L. La micropérimétrie statique avec l'ophtalmoscope à balayage laser. Ophtalmologie. 1990 May-Jun;4(3):291–294. [PubMed] [Google Scholar]
- Wendel R. T., Patel A. C., Kelly N. E., Salzano T. C., Wells J. W., Novack G. D. Vitreous surgery for macular holes. Ophthalmology. 1993 Nov;100(11):1671–1676. doi: 10.1016/s0161-6420(93)31419-3. [DOI] [PubMed] [Google Scholar]
- Wiznia R. A. Reversibility of the early stages of idiopathic macular holes. Am J Ophthalmol. 1989 Mar 15;107(3):241–245. doi: 10.1016/0002-9394(89)90306-1. [DOI] [PubMed] [Google Scholar]
- de Bustros S. Vitrectomy for prevention of macular holes. Results of a randomized multicenter clinical trial. Vitrectomy for Prevention of Macular Hole Study Group. Ophthalmology. 1994 Jun;101(6):1055–1060. doi: 10.1016/s0161-6420(94)31218-8. [DOI] [PubMed] [Google Scholar]


