Abstract
AIMS/BACKGROUND—Deep lamellar keratoplasty (DLK) was performed to restore visual acuity in 120 eyes with corneal stromal opacification. DLK is believed to be an effective treatment in eyes in which endothelial cell function had been preserved, and in which there was no epithelial or stromal oedema. The purpose of this study was to evaluate the effectiveness of this treatment. METHODS—The stroma was excised to the extent that only Descemet's membrane remained, at least in the optical zone. Donor corneas of full, or almost full, thickness with Descemet's membrane removed, or which had been lathed to a thickness of 0.4 mm from the endothelial side, were attached by suturing. RESULTS—In 113 eyes which were observed for 6 months or more postoperatively in which average prospective visual acuity was 0.09, average postoperative visual acuity improved to 0.6. Specular microscopy 1 month postoperatively revealed average endothelial cell counts of 2225 (SD 659)/mm2, while 24 months postoperatively this value was 1937 (642)/mm2 (cell loss 13%). Puncturing of Descemet's membrane during surgery occurred in 47 of 120 eyes (39.2%), but after 12 months, there was no difference in visual acuity or number of endothelial cells between these eyes and those in which no puncturing had occurred. CONCLUSIONS—There was no postoperative endothelial rejection reaction with DLK, and restoration of postoperative visual acuity was quite adequate. Compared with penetrating keratoplasty, DLK allows endothelial cell counts to be maintained for a longer period. In addition, results can be expected to be more consistent over the long term with DLK.
Full Text
The Full Text of this article is available as a PDF (120.9 KB).
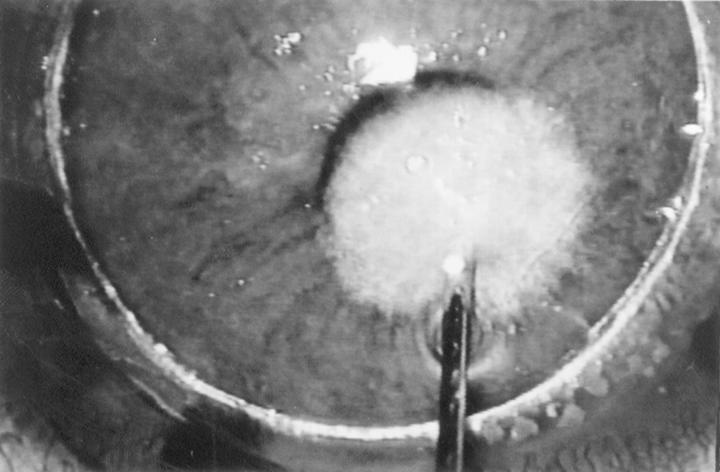
Figure 1 .
Hydrodelamination. A solution injected into the normal stroma spreads evenly in all directions and the remaining stroma whiten and swell.
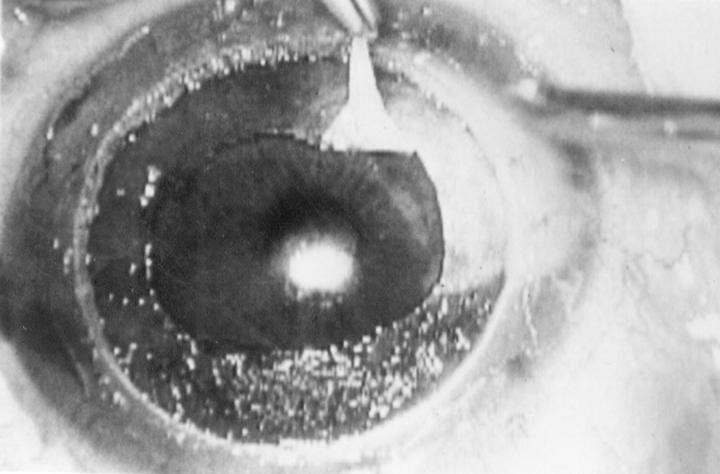
Figure 2 .
Spatula delamination. A fine spatula inserts rectilinearly into the hydrodelaminated stroma and comes back and is moved again and again fan-like in different directions.
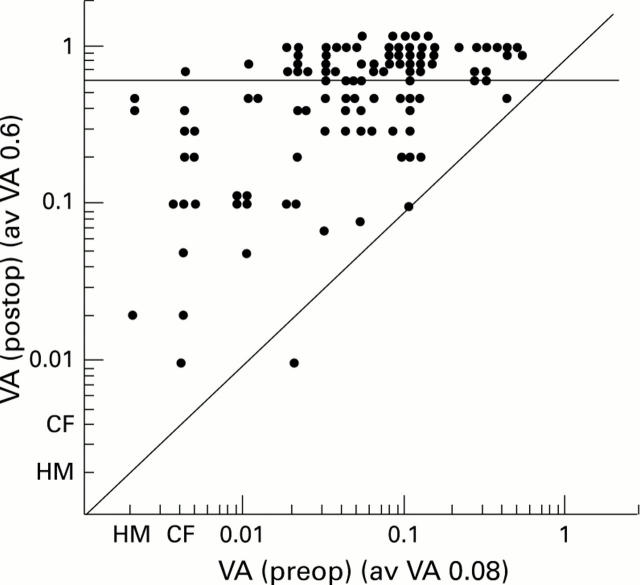
Figure 3 .
Descemet's membrane is smooth and even, clearly distinguishable from the stroma.
Figure 4 .
Change of preoperative and postoperative visual acuity (87 eyes were followed up for more than 6 months).
Figure 5 .
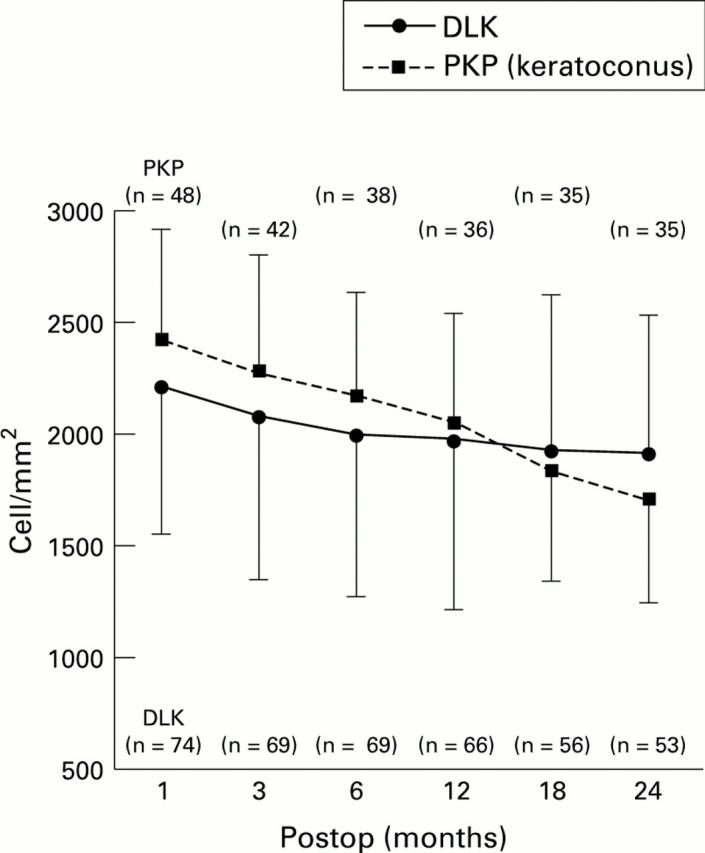
Trend of decrease in postoperative endothelial cell counts, in 74 eyes that underwent deep lamellar keratoplasty(DLK) and 48 eyes that underwent penetrating keratoplasty (PKP) with keratoconus.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Archila E. A. Deep lamellar keratoplasty dissection of host tissue with intrastromal air injection. Cornea. 1984;3(3):217–218. [PubMed] [Google Scholar]
- Bourne W. M., Hodge D. O., Nelson L. R. Corneal endothelium five years after transplantation. Am J Ophthalmol. 1994 Aug 15;118(2):185–196. doi: 10.1016/s0002-9394(14)72898-3. [DOI] [PubMed] [Google Scholar]
- Chau G. K., Dilly S. A., Sheard C. E., Rostron C. K. Deep lamellar keratoplasty on air with lyophilised tissue. Br J Ophthalmol. 1992 Nov;76(11):646–650. doi: 10.1136/bjo.76.11.646. [DOI] [PMC free article] [PubMed] [Google Scholar]