Abstract
AIM/BACKGROUND—Alport syndrome is an X linked disease that results in renal failure, deafness, and ocular abnormalities including a dot and fleck retinopathy and anterior lenticonus. The ultrastructural appearance of the glomerular basement membrane in thin basement membrane disease (TBMD) resembles that seen in some patients with Alport syndrome, and in some cases this disease is inherited too. The aim of this study was to determine whether patients with TBMD have any ocular abnormalities. METHODS—The eyes of 17 unrelated individuals with TBMD were studied by slit-lamp, including biomicroscopic fundus examination with a 78 D lens, by direct ophthalmoscopy, and by fundal photographs. The findings were compared with those in patients with IgA glomerulonephritis or Alport syndrome, and in normals. RESULTS—No patient with TBMD had a dot and fleck retinopathy or anterior lenticonus. A corneal dystrophy (n = 2) or pigmentation (n = 1), and retinal pigment epithelial clumping and maculopathy (n = 1) were noted. Corneal, lens, and retinal dots were found in five (29%), three (18%), and 16 (94%) patients, respectively, but these were also demonstrated in individuals with other renal diseases and in normal individuals. CONCLUSIONS—The dot and fleck retinopathy and anterior lenticonus typical of Alport syndrome do not occur in TBMD. The protein abnormality and genetic defect in TBMD are not known, but the lack of ocular lesions suggests that the abnormal protein in this disease is more sparsely distributed or less important in the basement membranes of the eye than of the kidney. Alternatively, the protein may be less affected by the mutations responsible for TBMD.
Full Text
The Full Text of this article is available as a PDF (196.9 KB).
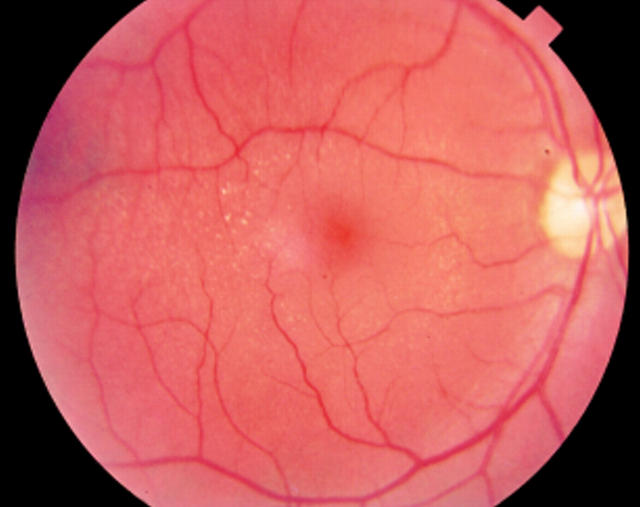
Figure 1 .
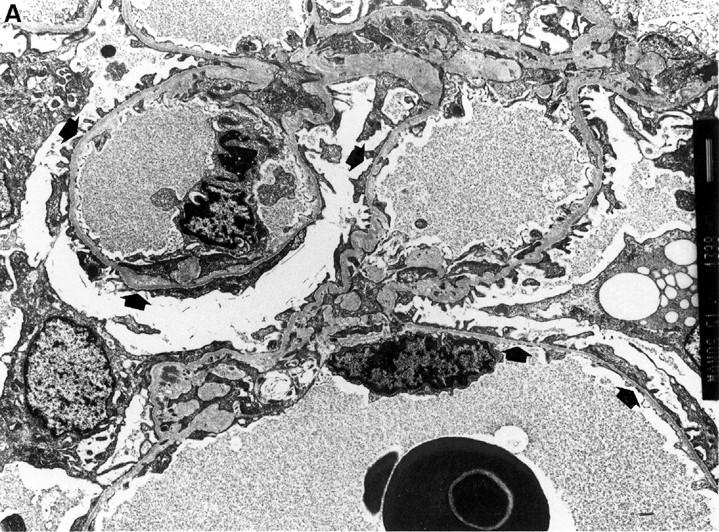
(A) Electron micrograph showing diffuse thinning of the glomerular basement membrane (arrows) in a patient with thin basement membrane disease (TBMD) whose optic fundus is shown in (B) and (C) (× 1440). (B) There is retinal pigment epithelial clumping and maculopathy (thick arrow), and scattered small yellow-white round dots (small arrows), both close to vessels and in the intervascular spaces in the fundal photograph of the left eye of a patient (IM) with TBMD. (C) Fluorescein angiogram of the fundus of the left eye in the same patient, showing increased fluorescence in the perifoveolar region, but no increased fluorescence of white dots, indicating that these are not small hard drusen.
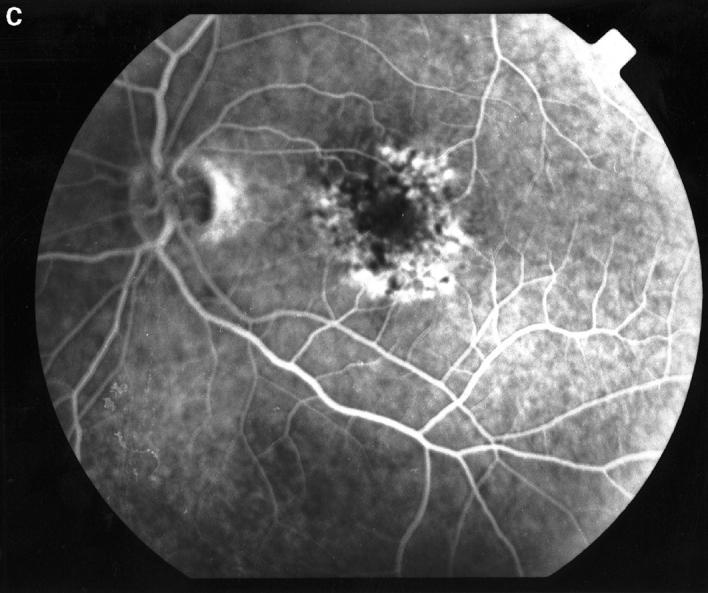
Figure 2 .
The perifoveal dot and fleck retinopathy in a patient with X linked Alport syndrome (NH).
Figure 3 .
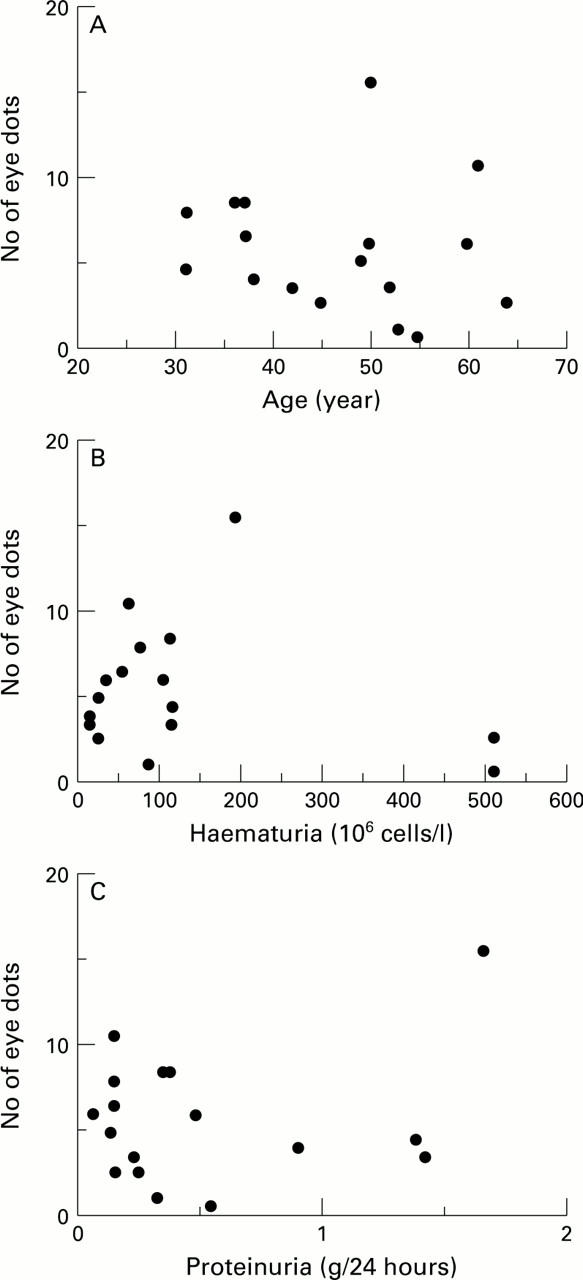
There is no correlation between the average number of retinal dots in any individual and (A) the age of the patients, (B) the number of urinary RBC × 106/l at presentation, or (C) the amount of proteinuria at presentation.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BROWNELL R. D., WOLTER J. R. ANTERIOR LENTICONUS IN FAMILIAL HEMORRHAGIC NEPHRITIS. DEMONSTRATION OF LENS PATHOLOGY. Arch Ophthalmol. 1964 Apr;71:481–483. doi: 10.1001/archopht.1964.00970010497007. [DOI] [PubMed] [Google Scholar]
- Barker D. F., Hostikka S. L., Zhou J., Chow L. T., Oliphant A. R., Gerken S. C., Gregory M. C., Skolnick M. H., Atkin C. L., Tryggvason K. Identification of mutations in the COL4A5 collagen gene in Alport syndrome. Science. 1990 Jun 8;248(4960):1224–1227. doi: 10.1126/science.2349482. [DOI] [PubMed] [Google Scholar]
- Cheong H. I., Kashtan C. E., Kim Y., Kleppel M. M., Michael A. F. Immunohistologic studies of type IV collagen in anterior lens capsules of patients with Alport syndrome. Lab Invest. 1994 Apr;70(4):553–557. [PubMed] [Google Scholar]
- Dische F. E., Anderson V. E., Keane S. J., Taube D., Bewick M., Parsons V. Incidence of thin membrane nephropathy: morphometric investigation of a population sample. J Clin Pathol. 1990 Jun;43(6):457–460. doi: 10.1136/jcp.43.6.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dische F. E., Weston M. J., Parsons V. Abnormally thin glomerular basement membranes associated with hematuria, proteinuria or renal failure in adults. Am J Nephrol. 1985;5(2):103–109. doi: 10.1159/000166914. [DOI] [PubMed] [Google Scholar]
- Fine B. S., Kwapien R. P. Pigment epithelial windows and drusen: an animal model. Invest Ophthalmol Vis Sci. 1978 Nov;17(11):1059–1068. [PubMed] [Google Scholar]
- Fine B. S. Lipoidal degeneration of the retinal pigment epithelium. Am J Ophthalmol. 1981 Apr;91(4):469–473. doi: 10.1016/0002-9394(81)90234-8. [DOI] [PubMed] [Google Scholar]
- Flinter F. Molecular genetics of Alport's syndrome. Q J Med. 1993 May;86(5):289–292. [PubMed] [Google Scholar]
- Govan J. A. Ocular manifestations of Alport's syndrome: a hereditary disorder of basement membranes? Br J Ophthalmol. 1983 Aug;67(8):493–503. doi: 10.1136/bjo.67.8.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill G. S., Jenis E. H., Goodloe S., Jr The nonspecificity of the ultrastructural alterations in hereditary nephritis with additional observations on benign familial hematuria. Lab Invest. 1974 Nov;31(5):516–532. [PubMed] [Google Scholar]
- Ishizaki M., Westerhausen-Larson A., Kino J., Hayashi T., Kao W. W. Distribution of collagen IV in human ocular tissues. Invest Ophthalmol Vis Sci. 1993 Aug;34(9):2680–2689. [PubMed] [Google Scholar]
- Iversen U. M. Hereditary nephropathy with hearing loss. "Alport's syndrome". Acta Paediatr Scand Suppl. 1974;(245):1–23. [PubMed] [Google Scholar]
- Jensen E. B., Gundersen H. J., Osterby R. Determination of membrane thickness distribution from orthogonal intercepts. J Microsc. 1979 Jan;115(1):19–33. doi: 10.1111/j.1365-2818.1979.tb00149.x. [DOI] [PubMed] [Google Scholar]
- Mochizuki T., Lemmink H. H., Mariyama M., Antignac C., Gubler M. C., Pirson Y., Verellen-Dumoulin C., Chan B., Schröder C. H., Smeets H. J. Identification of mutations in the alpha 3(IV) and alpha 4(IV) collagen genes in autosomal recessive Alport syndrome. Nat Genet. 1994 Sep;8(1):77–81. doi: 10.1038/ng0994-77. [DOI] [PubMed] [Google Scholar]
- Perrin D., Jungers P., Grünfeld J. P., Delons S., Noël L. H., Zenatti C. Perimacular changes in Alport's syndrome. Clin Nephrol. 1980 Apr;13(4):163–167. [PubMed] [Google Scholar]
- Perry G. J., George C. R., Field M. J., Collett P. V., Kalowski S., Wyndham R. N., Newland R. C., Lin B. P., Kneale K. L., Lawrence J. R. Thin-membrane nephropathy--a common cause of glomerular haematuria. Med J Aust. 1989 Dec 4;151(11-12):638–642. doi: 10.5694/j.1326-5377.1989.tb139637.x. [DOI] [PubMed] [Google Scholar]
- Reeders S. T. Molecular genetics of hereditary nephritis. Kidney Int. 1992 Sep;42(3):783–792. doi: 10.1038/ki.1992.348. [DOI] [PubMed] [Google Scholar]
- Rogers P. W., Kurtzman N. A., Bunn S. M., Jr, White M. G. Familial benign essential hematuria. Arch Intern Med. 1973 Feb;131(2):257–262. [PubMed] [Google Scholar]
- Sabates R., Krachmer J. H., Weingeist T. A. Ocular findings in Alport's syndrome. Ophthalmologica. 1983;186(4):204–210. doi: 10.1159/000309287. [DOI] [PubMed] [Google Scholar]
- Tiebosch A. T., Frederik P. M., van Breda Vriesman P. J., Mooy J. M., van Rie H., van de Wiel T. W., Wolters J., Zeppenfeldt E. Thin-basement-membrane nephropathy in adults with persistent hematuria. N Engl J Med. 1989 Jan 5;320(1):14–18. doi: 10.1056/NEJM198901053200103. [DOI] [PubMed] [Google Scholar]
- el Baba F., Green W. R., Fleischmann J., Finkelstein D., de la Cruz Z. C. Clinicopathologic correlation of lipidization and detachment of the retinal pigment epithelium. Am J Ophthalmol. 1986 May 15;101(5):576–583. doi: 10.1016/0002-9394(86)90948-7. [DOI] [PubMed] [Google Scholar]