Abstract
AIM—To assess the centre of fixation before laser photocoagulation of well defined juxtafoveal or extrafoveal choroidal neovascularisation (CNV) secondary to age related macular degeneration (AMD), and to better predict visual function after treatment using scanning laser ophthalmoscope (SLO) fundus perimetry. METHODS—19 consecutive eyes with juxtafoveal or extrafoveal CNV were examined by fundus perimetry before and after laser treatment with documentation of the fixation point using the SLO. The stability of fixation was defined as standard deviation around the mean fixation point. Overlays of fluorescein angiographic pictures and fundus perimetry were obtained using image analysis software. RESULTS—Fundus perimetry allowed accurate determination of the centre of fixation. Overlays demonstrated the precise geographic relation of the angiographically detectable foveal margin of the CNV and the centre of fixation. Thereby, prediction of the visual outcome with regard to reading ability was facilitated. Stability of fixation did not change significantly after treatment. CONCLUSIONS—Fundus perimetry using the SLO was helpful in patients who underwent laser treatment for juxtafoveal or extrafoveal CNV secondary to AMD and may aid the pretreatment counselling of such patients.
Full Text
The Full Text of this article is available as a PDF (247.1 KB).
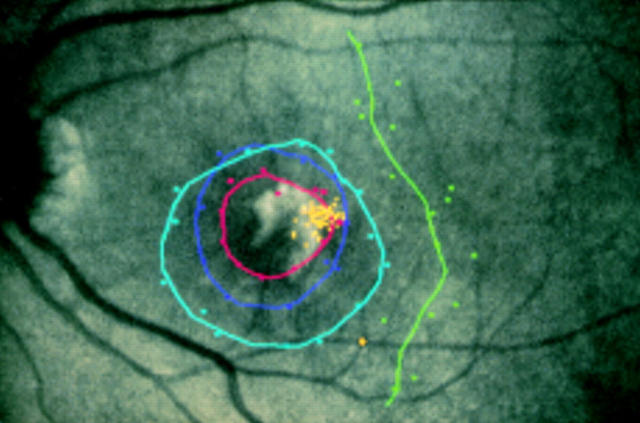
Figure 1 .
Comparison of the visibility of the choroidal neovascularisation (CNV) using different illumination wavelengths in a left eye. (A) Fundus image using the SLO with argon blue light, as obtained during beginning of the angiography, does not show the CNV. (B) Midphase of angiography clearly outlines the choroidal neovascular membrane. (C) Fundus image obtained using infrared diode laser of the SLO with mean fixation point and a circle demonstrating the standard deviation of fixation; the CNV is clearly visible.
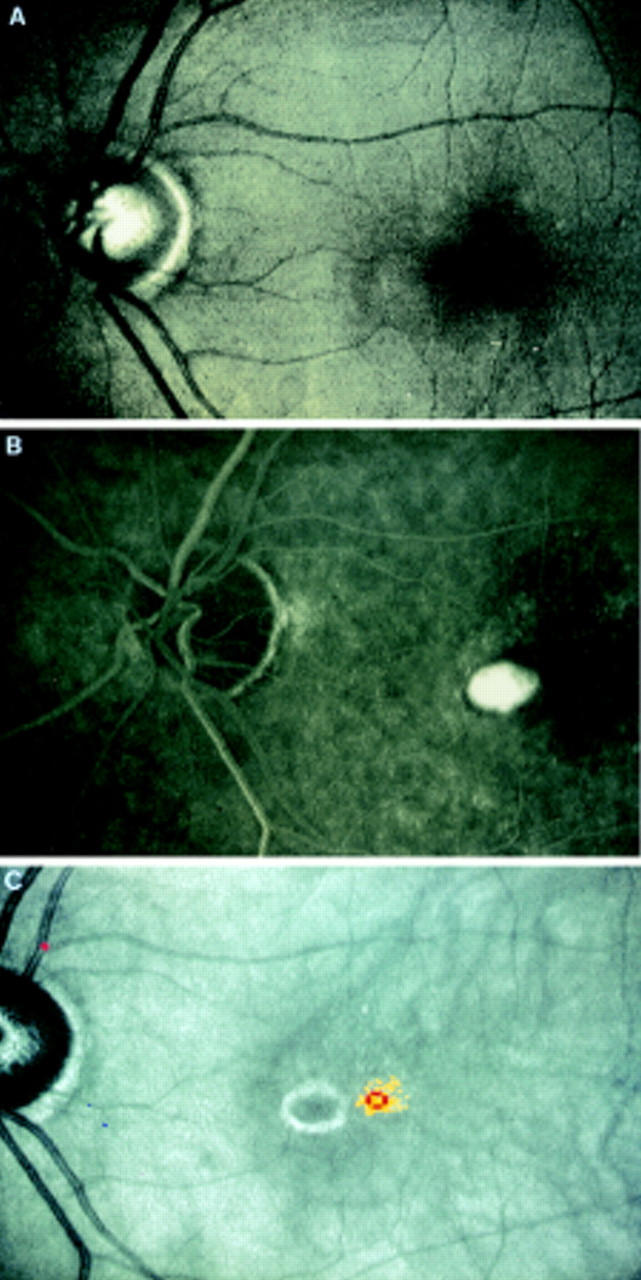
Figure 2 .
Results of static fundus perimetry in a right eye of a patient with choroidal neovascularisation (CNV). (A) Standard image with threshold values according to the right hand scale with brightest stimuli at the top and smallest contrast between stimuli and background at the bottom. Single fixation points are drawn as yellow dots. (B) Results converted onto the mid time sequence of fluorescence angiography which enables direct visualisation of mean fixation point in relation to classic CNV.
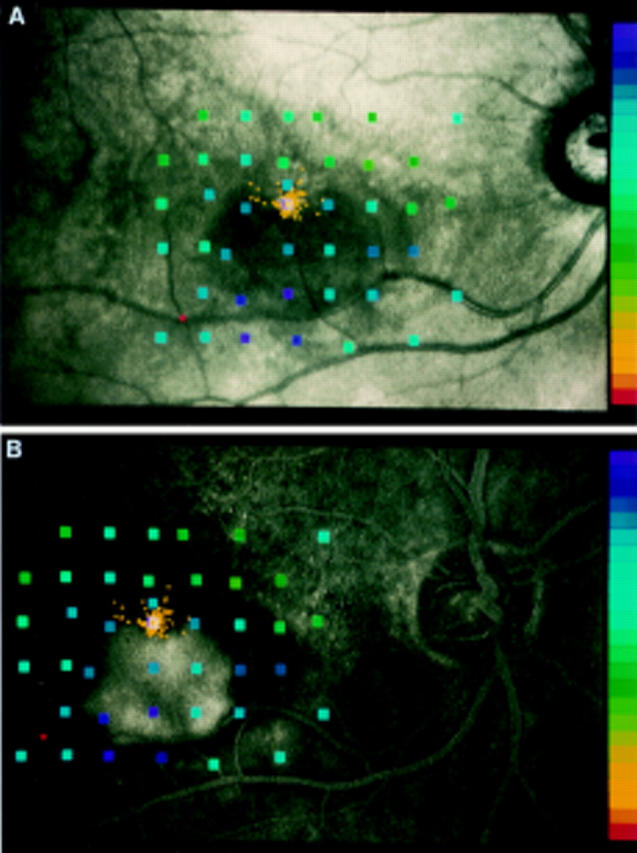
Figure 3 .
Example of subjectively poor visual outcome in a left eye after treatment although visual acuity by conventional testing has remained unchanged. The mean fixation point is located at the right margin of the laser scar at the fundus (yellow points). This will lead to a scotoma at the left of the point of fixation which makes reading more difficult owing to missing of the words or digits which have just been read. Kinetic perimetry shows an absolute scotoma (0 dB, Goldmann II, red circle) and a larger relative scotoma (5 dB purple, 10 dB blue, 15 dB green).
Figure 4 .
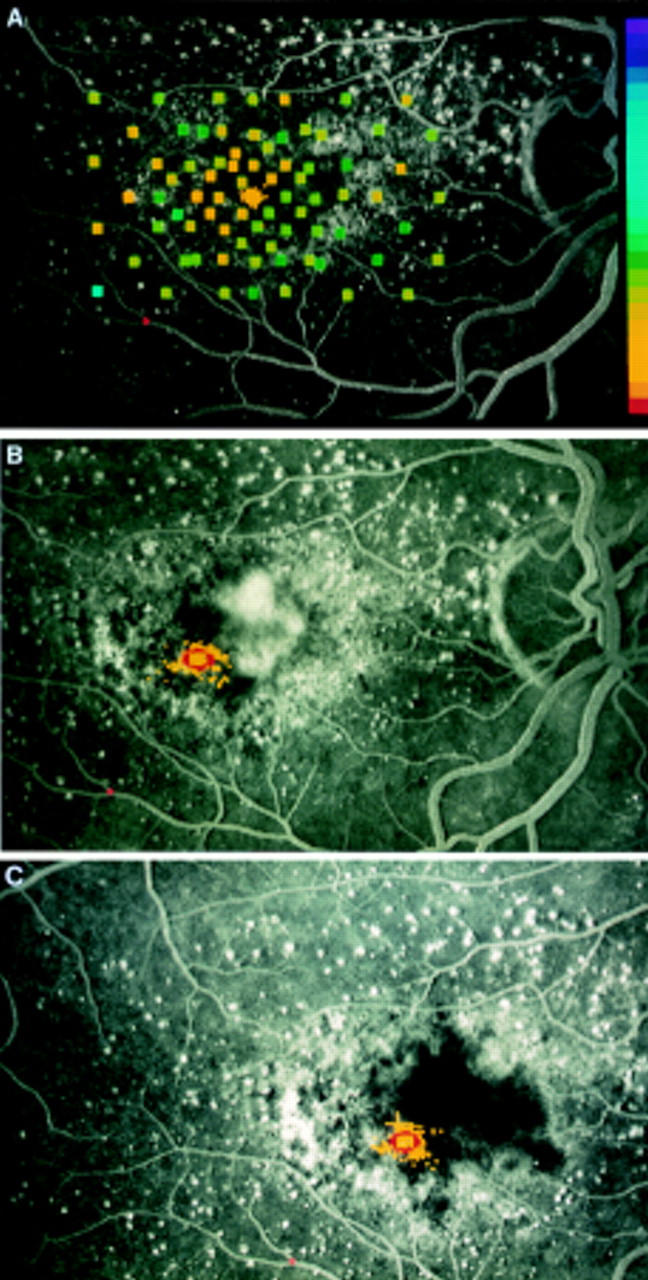
Right eye of a 67-year-old woman first presenting with decrease of visual acuity in the left eye. Right eye showed nearly normal perimetric results with the SLO (right hand scale with brightest stimuli at the top and smallest contrast between stimuli and background at the bottom) and central fixation (yellow dots) while angiography demonstrates macular degeneration without defined leakage (A). (B) Six months later juxtafoveolar CNV nasally of the fovea can be seen during fluorescein angiography, mean fixation point has shifted temporally and stability of fixation is worse (red circle). (C) Four months after laser treatment no recurrence can be seen, visual acuity is 0.4, and reading ability is improved subjectively. Location and stability of fixation as measured during SLO perimetry are about the same.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aulhorn E., Michelfelder F. Vergleich der Fixationsverlagerung bei organischen Maculaerkrankungen und beim physiologischen Dunkelskotom. Ber Zusammenkunft Dtsch Ophthalmol Ges. 1972;71:487–491. [PubMed] [Google Scholar]
- Delori F. C., Gragoudas E. S., Francisco R., Pruett R. C. Monochromatic ophthalmoscopy and fundus photography. The normal fundus. Arch Ophthalmol. 1977 May;95(5):861–868. doi: 10.1001/archopht.1977.04450050139018. [DOI] [PubMed] [Google Scholar]
- Kaling M., Kugler W., Ross K., Zoidl C., Ryffel G. U. Liver-specific gene expression: A-activator-binding site, a promoter module present in vitellogenin and acute-phase genes. Mol Cell Biol. 1991 Jan;11(1):93–101. doi: 10.1128/mcb.11.1.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein M. L., Jorizzo P. A., Watzke R. C. Growth features of choroidal neovascular membranes in age-related macular degeneration. Ophthalmology. 1989 Sep;96(9):1416–1421. doi: 10.1016/s0161-6420(89)32741-2. [DOI] [PubMed] [Google Scholar]
- Rohrschneider K., Becker M., Fendrich T., Völcker H. E. Kinetische funduskontrollierte Perimetrie mit dem Scanning-Laser-Ophthalmoskop. Klin Monbl Augenheilkd. 1995 Aug;207(2):102–110. doi: 10.1055/s-2008-1035356. [DOI] [PubMed] [Google Scholar]
- Rohrschneider K., Becker M., Kruse F. E., Fendrich T., Völcker H. E. Stability of fixation: results of fundus-controlled examination using the scanning laser ophthalmoscope. Ger J Ophthalmol. 1995 Jul;4(4):197–202. [PubMed] [Google Scholar]
- Rohrschneider K., Fendrich T., Becker M., Krastel H., Kruse F. E., Völcker H. E. Static fundus perimetry using the scanning laser ophthalmoscope with an automated threshold strategy. Graefes Arch Clin Exp Ophthalmol. 1995 Dec;233(12):743–749. doi: 10.1007/BF00184084. [DOI] [PubMed] [Google Scholar]
- Sjaarda R. N., Frank D. A., Glaser B. M., Thompson J. T., Murphy R. P. Resolution of an absolute scotoma and improvement of relative scotomata after successful macular hole surgery. Am J Ophthalmol. 1993 Aug 15;116(2):129–139. doi: 10.1016/s0002-9394(14)71276-0. [DOI] [PubMed] [Google Scholar]
- Sunness J. S., Bressler N. M., Maguire M. G. Scanning laser ophthalmoscopic analysis of the pattern of visual loss in age-related geographic atrophy of the macula. Am J Ophthalmol. 1995 Feb;119(2):143–151. doi: 10.1016/s0002-9394(14)73866-8. [DOI] [PubMed] [Google Scholar]
- Sunness J. S., Schuchard R. A., Shen N., Rubin G. S., Dagnelie G., Haselwood D. M. Landmark-driven fundus perimetry using the scanning laser ophthalmoscope. Invest Ophthalmol Vis Sci. 1995 Aug;36(9):1863–1874. [PMC free article] [PubMed] [Google Scholar]