Abstract
AIM—To investigate the effect of prophylactic laser treatment on drusen area and incidence of exudative lesions in patients with soft drusen maculopathy. METHODS—In a prospective study, patients with early age related maculopathy (ARM) and good visual acuity were randomised to laser treatment or to a control group. Each group consisted of two subgroups: a fellow eye group and a bilateral drusen group. At 3 years, 36 of 38 enrolled patients remained in the study. Photocoagulation was performed with an argon green laser, approximately 100 mild laser burns being placed on and between the drusen in a perifoveal temporal horseshoe-shaped area. Both cases and controls were subjected to fundus colour photographs and fluorescein angiograms at regular intervals, and the drusen area was calculated in both photographs and angiograms. At baseline, there were no significant differences (p>0.3-0.8) in drusen area between the groups. RESULTS—In the treatment group, mean drusen area decreased significantly in the fundus photographs as well as in the angiograms (p<0.001). Visual acuity and colour contrast sensitivity (CCS) did not change significantly. All these results are valid also for the subgroups. In the control group, however, mean drusen area increased significantly (p<0.001). Mean visual acuity decreased significantly (p<0.01) as did the colour contrast sensitivity along the tritan axis (p=0.02). For the fellow eye control group (n=7), the increase in drusen area in fundus photographs and the decrease in CCS along the tritan axis were not statistically significant (p=0.57 and p=0.37, respectively). Furthermore, at 3 years, five patients in the control group showed exudative lesions (1/7 in the fellow eye group and 4/12 in the bilateral drusen group), whereas no such complications occurred in the treatment group. One patient developed a small atrophy, however. Thus, there is now a significant difference (p=0.047), however with a large 95% confidence interval, 0.06-0.46, regarding exudative complications between the treated group and the control group in our small patient material. CONCLUSION—Perifoveal mild laser treatment causes a reduction in drusen area in patients with soft drusen maculopathy and may lower the incidence of exudative lesions. Keywords: age related maculopathy; exudative complications; laser photocoagulation; soft drusen
Full Text
The Full Text of this article is available as a PDF (124.1 KB).
Figure 1 .
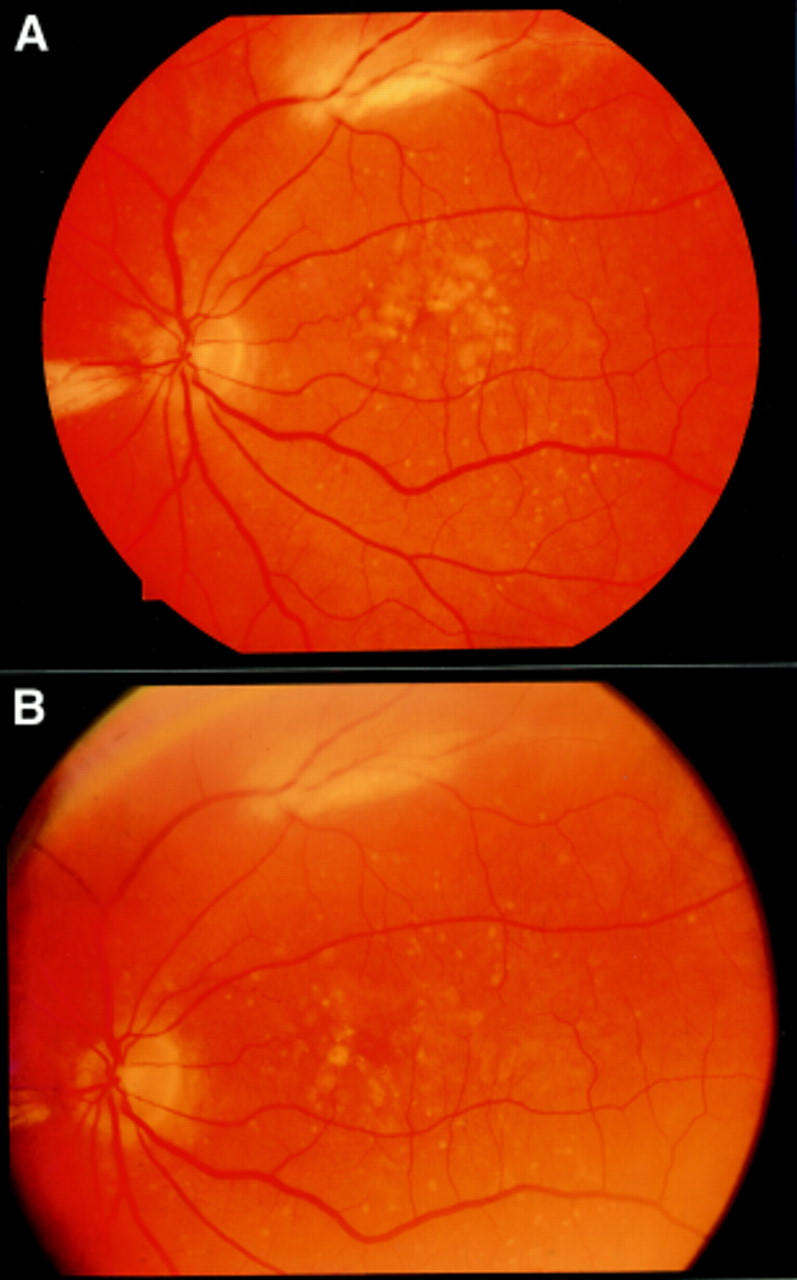
Colour fundus photographs of a 70 year old man (A) before and (B) 3 years after perifoveal laser photocoagulation.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arden G. B., Berninger T., Hogg C. R., Perry S. A survey of color discrimination in German ophthalmologists. Changes associated with the use of lasers and operating microscopes. Ophthalmology. 1991 May;98(5):567–575. [PubMed] [Google Scholar]
- Bressler S. B., Maguire M. G., Bressler N. M., Fine S. L. Relationship of drusen and abnormalities of the retinal pigment epithelium to the prognosis of neovascular macular degeneration. The Macular Photocoagulation Study Group. Arch Ophthalmol. 1990 Oct;108(10):1442–1447. doi: 10.1001/archopht.1990.01070120090035. [DOI] [PubMed] [Google Scholar]
- Campochiaro P. A., Hackett S. F., Vinores S. A., Freund J., Csaky C., LaRochelle W., Henderer J., Johnson M., Rodriguez I. R., Friedman Z. Platelet-derived growth factor is an autocrine growth stimulator in retinal pigmented epithelial cells. J Cell Sci. 1994 Sep;107(Pt 9):2459–2469. doi: 10.1242/jcs.107.9.2459. [DOI] [PubMed] [Google Scholar]
- Cleasby G. W., Nakanishi A. S., Norris J. L. Prophylactic photocoagulation of the fellow eye in exudative senile maculopathy. A preliminary report. Mod Probl Ophthalmol. 1979;20:141–147. [PubMed] [Google Scholar]
- Duvall J., Tso M. O. Cellular mechanisms of resolution of drusen after laser coagulation. An experimental study. Arch Ophthalmol. 1985 May;103(5):694–703. doi: 10.1001/archopht.1985.01050050086024. [DOI] [PubMed] [Google Scholar]
- Figueroa M. S., Regueras A., Bertrand J. Laser photocoagulation to treat macular soft drusen in age-related macular degeneration. Retina. 1994;14(5):391–396. doi: 10.1097/00006982-199414050-00001. [DOI] [PubMed] [Google Scholar]
- Frennesson C., Nilsson U. L., Nilsson S. E. Colour contrast sensitivity in patients with soft drusen, an early stage of ARM. Doc Ophthalmol. 1995;90(4):377–386. doi: 10.1007/BF01268123. [DOI] [PubMed] [Google Scholar]
- Frennesson I. C., Nilsson S. E. Effects of argon (green) laser treatment of soft drusen in early age-related maculopathy: a 6 month prospective study. Br J Ophthalmol. 1995 Oct;79(10):905–909. doi: 10.1136/bjo.79.10.905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frennesson I. C., Nilsson S. E. Laser photocoagulation of soft drusen in early age-related maculopathy (ARM). The one-year results of a prospective, randomised trial. Eur J Ophthalmol. 1996 Jul-Sep;6(3):307–314. doi: 10.1177/112067219600600315. [DOI] [PubMed] [Google Scholar]
- Freund K. B., Yannuzzi L. A., Sorenson J. A. Age-related macular degeneration and choroidal neovascularization. Am J Ophthalmol. 1993 Jun 15;115(6):786–791. doi: 10.1016/s0002-9394(14)73649-9. [DOI] [PubMed] [Google Scholar]
- Gass J. D. Drusen and disciform macular detachment and degeneration. Arch Ophthalmol. 1973 Sep;90(3):206–217. doi: 10.1001/archopht.1973.01000050208006. [DOI] [PubMed] [Google Scholar]
- Gregor Z., Bird A. C., Chisholm I. H. Senile disciform macular degeneration in the second eye. Br J Ophthalmol. 1977 Feb;61(2):141–147. doi: 10.1136/bjo.61.2.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guymer R. H., Gross-Jendroska M., Owens S. L., Bird A. C., Fitzke F. W. Laser treatment in subjects with high-risk clinical features of age-related macular degeneration. Posterior pole appearance and retinal function. Arch Ophthalmol. 1997 May;115(5):595–603. doi: 10.1001/archopht.1997.01100150597004. [DOI] [PubMed] [Google Scholar]
- Holz F. G., Wolfensberger T. J., Piguet B., Gross-Jendroska M., Wells J. A., Minassian D. C., Chisholm I. H., Bird A. C. Bilateral macular drusen in age-related macular degeneration. Prognosis and risk factors. Ophthalmology. 1994 Sep;101(9):1522–1528. doi: 10.1016/s0161-6420(94)31139-0. [DOI] [PubMed] [Google Scholar]
- Klein R., Klein B. E., Jensen S. C., Meuer S. M. The five-year incidence and progression of age-related maculopathy: the Beaver Dam Eye Study. Ophthalmology. 1997 Jan;104(1):7–21. doi: 10.1016/s0161-6420(97)30368-6. [DOI] [PubMed] [Google Scholar]
- Little H. L., Showman J. M., Brown B. W. A pilot randomized controlled study on the effect of laser photocoagulation of confluent soft macular drusen. Ophthalmology. 1997 Apr;104(4):623–631. doi: 10.1016/s0161-6420(97)30261-9. [DOI] [PubMed] [Google Scholar]
- Marshall J. Interactions between sensory cells, glial cells and the retinal pigment epithelium and their response to photocoagulation. Dev Ophthalmol. 1981;2:308–317. doi: 10.1159/000395340. [DOI] [PubMed] [Google Scholar]
- Miller H., Miller B., Ishibashi T., Ryan S. J. Pathogenesis of laser-induced choroidal subretinal neovascularization. Invest Ophthalmol Vis Sci. 1990 May;31(5):899–908. [PubMed] [Google Scholar]
- Sarks S. H., Arnold J. J., Sarks J. P., Gilles M. C., Walter C. J. Prophylactic perifoveal laser treatment of soft drusen. Aust N Z J Ophthalmol. 1996 Feb;24(1):15–26. doi: 10.1111/j.1442-9071.1996.tb01546.x. [DOI] [PubMed] [Google Scholar]
- Sigelman J. Foveal drusen resorption one year after perifoveal laser photocoagulation. Ophthalmology. 1991 Sep;98(9):1379–1383. doi: 10.1016/s0161-6420(91)32122-5. [DOI] [PubMed] [Google Scholar]
- Smiddy W. E., Fine S. L. Prognosis of patients with bilateral macular drusen. Ophthalmology. 1984 Mar;91(3):271–277. doi: 10.1016/s0161-6420(84)34309-3. [DOI] [PubMed] [Google Scholar]
- Strahlman E. R., Fine S. L., Hillis A. The second eye of patients with senile macular degeneration. Arch Ophthalmol. 1983 Aug;101(8):1191–1193. doi: 10.1001/archopht.1983.01040020193003. [DOI] [PubMed] [Google Scholar]
- Wallow I. H. Repair of the pigment epithelial barrier following photocoagulation. Arch Ophthalmol. 1984 Jan;102(1):126–135. doi: 10.1001/archopht.1984.01040030104047. [DOI] [PubMed] [Google Scholar]
- Wetzig P. C. Photocoagulation of drusen-related macular degeneration: a long-term outcome. Trans Am Ophthalmol Soc. 1994;92:299–306. [PMC free article] [PubMed] [Google Scholar]
- Yamamoto C., Ogata N., Yi X., Takahashi K., Miyashiro M., Yamada H., Uyama M., Matsuzaki K. Immunolocalization of basic fibroblast growth factor during wound repair in rat retina after laser photocoagulation. Graefes Arch Clin Exp Ophthalmol. 1996 Nov;234(11):695–702. doi: 10.1007/BF00292356. [DOI] [PubMed] [Google Scholar]


