Abstract
AIMS—Ultrasound biomicroscopy was used to study the shape of the iris and the iridolenticular contact in pigment dispersion syndrome (PDS) eyes, to compare them with matched normal eyes, and to assess the morphological effects of laser iridotomy in PDS eyes. METHODS—50 eyes of 50 patients suffering from PDS (group 1), and 15 normal eyes of 15 subjects matched for age and refraction (group 2), were studied by ultrasound biomicroscopy (UBM, Humphrey-Zeiss). Nd:YAG laser iridotomy was proposed to the 30 PDS patients with concave iris and 18 underwent the treatment. RESULTS—The iris was concave in 27 eyes in group 1, and three more eyes showed a concave iris during accommodation. Among normals, iris concavity was present in two eyes. The height of the iris convexity was −0.15 (0.24) mm (range −0.65 to +0.21), in the eyes of group 1, whereas it was +0.07 (0.10) mm (range −0.21 to +0.16) in group 2 (p<0.0012). Group 1 had greater iridolenticular contact than group 2: 1.55 (0.78) mm (range 0.30-2.88) and 1.07 (0.61) (range 0.30-2.50; p=0.0304). After laser iridotomy, only one eye still had a concave iris. Pre- and post-treatment deflections were −0.35 (0.18) mm (range −0.61 to -0.05) and +0.01 (0.06) mm (range −0.12 to +0.17), respectively (p<0.0001). Pre- and post-treatment iridolenticular contact was 2.10 (0.65) mm (range 0.70-2.88) and 0.93 (0.38) mm (range 0.4-1.75), respectively (p<0.0001). After laser iridotomy, the treated irises were flatter than normal (p=0.0207), whereas the iridolenticular contact was not significantly different. CONCLUSIONS—Laser iridotomy can restore a normal iris shape and iridolenticular contact in eyes suffering from PDS. Keywords: glaucoma; pigment dispersion syndrome; laser iridotomy; ultrasound biomicroscopy
Full Text
The Full Text of this article is available as a PDF (115.8 KB).
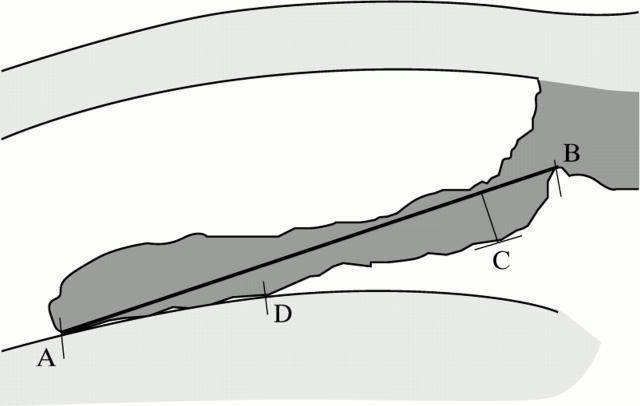
Figure 1 .
Iris deflection was measured by determining the maximum distance reached by the pigment epithelium (C) from a line joining the innermost point of the pigment epithelium in contact with the lens (A) with its outermost point at the iris root (B). Conventionally, the value was considered positive if the iris showed an anterior deflection (convexity) and negative in case of posterior deflection (concavity). Iridolenticular contact was quantified by measuring the distance between A and the outermost point of the pigment epithelium in contact with the lens (D).
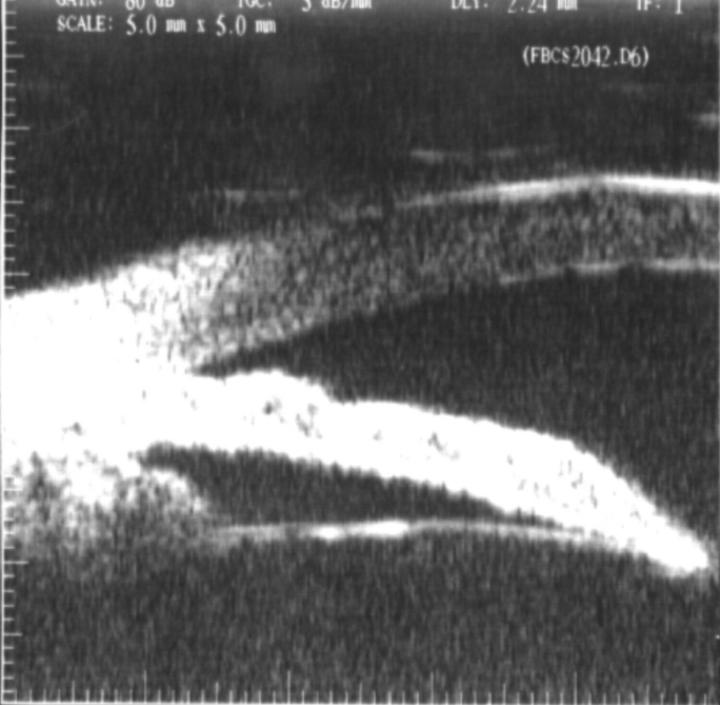
Figure 2 .
Ultrasound biomicroscopy image showing an evidently concave iris, before iridotomy.
Figure 3 .
Ultrasound biomicroscopy image showing the iridotomy in the same eye as Figure 2.
Figure 4 .
Same eye as Figures 2 and 3 after laser treatment: the iris is flat.
Figure 5 .
Ultrasound biomicroscopy appearance of a normal eye: the iris is slightly convex and iridolenticular contact is limited.
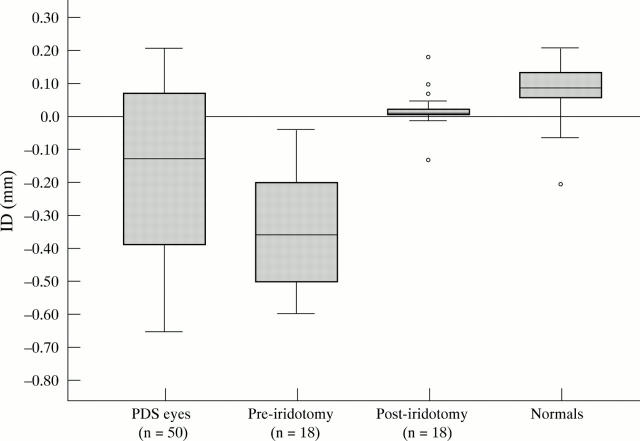
Figure 6 .
Box plot of the distribution of iris deflection (ID) in all PDS eyes, in PDS eyes before and after laser iridotomy, and in normal eyes.
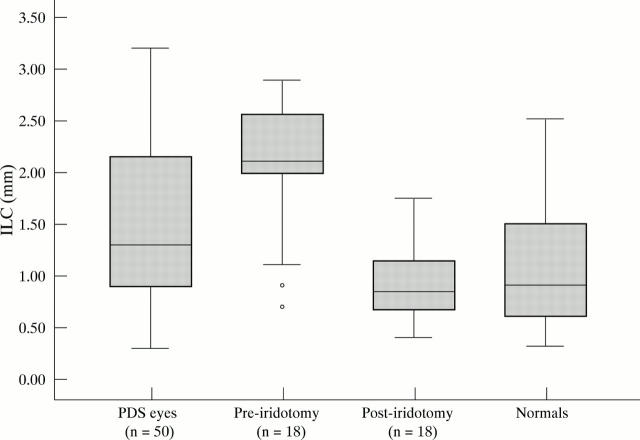
Figure 7 .
Box plot of the distribution of iridolenticular contact (ILC) in all PDS eyes, in PDS eyes before and after laser iridotomy, and in normal eyes.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Karickhoff J. R. Pigmentary dispersion syndrome and pigmentary glaucoma: a new mechanism concept, a new treatment, and a new technique. Ophthalmic Surg. 1992 Apr;23(4):269–277. [PubMed] [Google Scholar]
- Liebmann J. M., Tello C., Chew S. J., Cohen H., Ritch R. Prevention of blinking alters iris configuration in pigment dispersion syndrome and in normal eyes. Ophthalmology. 1995 Mar;102(3):446–455. doi: 10.1016/s0161-6420(95)31001-9. [DOI] [PubMed] [Google Scholar]
- Pavlin C. J., Harasiewicz K., Foster F. S. Posterior iris bowing in pigmentary dispersion syndrome caused by accommodation. Am J Ophthalmol. 1994 Jul 15;118(1):114–116. doi: 10.1016/s0002-9394(14)72855-7. [DOI] [PubMed] [Google Scholar]
- Pavlin C. J., Harasiewicz K., Sherar M. D., Foster F. S. Clinical use of ultrasound biomicroscopy. Ophthalmology. 1991 Mar;98(3):287–295. doi: 10.1016/s0161-6420(91)32298-x. [DOI] [PubMed] [Google Scholar]
- Pavlin C. J., Sherar M. D., Foster F. S. Subsurface ultrasound microscopic imaging of the intact eye. Ophthalmology. 1990 Feb;97(2):244–250. doi: 10.1016/s0161-6420(90)32598-8. [DOI] [PubMed] [Google Scholar]
- Potash S. D., Tello C., Liebmann J., Ritch R. Ultrasound biomicroscopy in pigment dispersion syndrome. Ophthalmology. 1994 Feb;101(2):332–339. doi: 10.1016/s0161-6420(94)31331-5. [DOI] [PubMed] [Google Scholar]