Abstract
BACKGROUND—The authors have previously concluded that fluid from an optic disc pit creates an inner layer separation (ILS) of the retina. An outer layer detachment (OLD) centred on the macula is a secondary phenomenon that causes a dense central scotoma. Pneumatic displacement of the OLD effects an improvement in central vision. Pathology to confirm these conclusions is lacking. Intraretinal images obtained by optical coherence tomography (OCT), however, are confirmatory. METHODS—Three patients with optic disc pit maculopathy were studied with stereoscopic photographs, visual fields, and OCT before and after intravitreal gas was injected to displace the central retinal elevation to below the inferior temporal vascular arcade. RESULTS—Preoperatively, OCT demonstrated an ILS that connected with the optic disc pit. External to it was an OLD that centred on the fovea and did not connect with the optic disc pit. Pneumatic displacement of the OLD was accompanied by an improvement in central vision. Long term follow up indicates that the effect of displacement may be temporary. CONCLUSION—OCT confirmed the two layer structure of optic disc pit maculopathy and that the improvement in central vision after pneumatic displacement coincides with a reattachment of the OLD in the macula. It also supports the hypothesis that the ILS, which persists, provides a conduit for the continuous flow of fluid from the pit to the displaced retinal elevation. Keywords: optical coherence tomography; optic disc pit maculopathy; intraocular gas; retinoschisis
Full Text
The Full Text of this article is available as a PDF (240.1 KB).
Figure 1 .
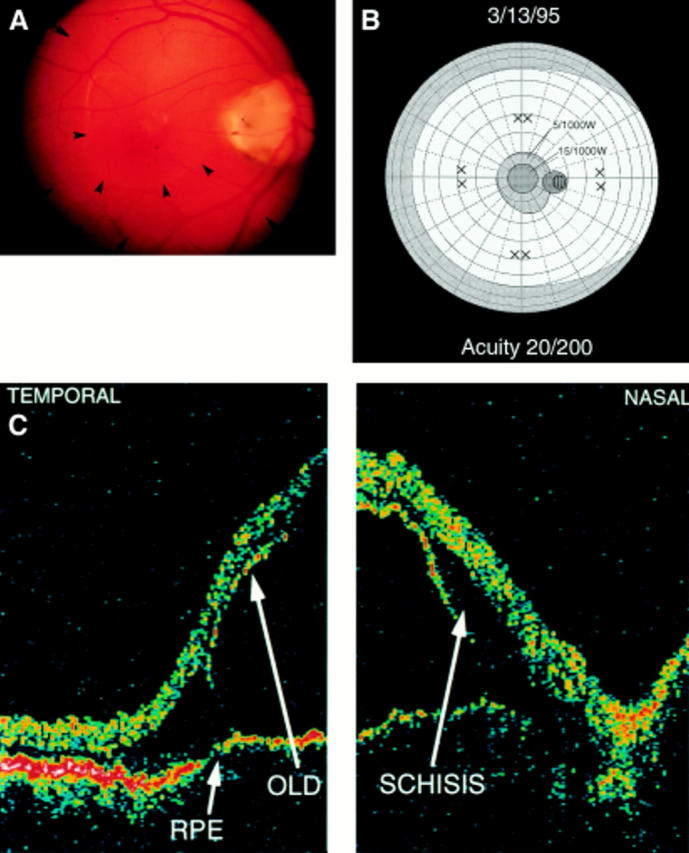
(A) The posterior pole of an eye with an optic disc pit maculopathy of 1 week's duration (patient no 1): a transparent ILS connects with the pit and extends to the superior and inferior vascular arcades (short arrows; outer circle). A relatively dense OLD (arrowheads) centres on the macula. (B) Central visual field of the patient whose eye is depicted in (A). There is a dense central scotoma (15/1000W) which is consistent with the OLD. It is surrounded by a less dense scotoma (5/1000W) which is consistent with the extent of the ILS. W = white. (C) OCT of the posterior pole of the eye depicted in (A). A schisis-like cavity is evident between the OLD and the internal layer separation. RPE = retinal pigment epithelium; OLD = outer layer detachment; − horizontal section through macula.
Figure 2 .
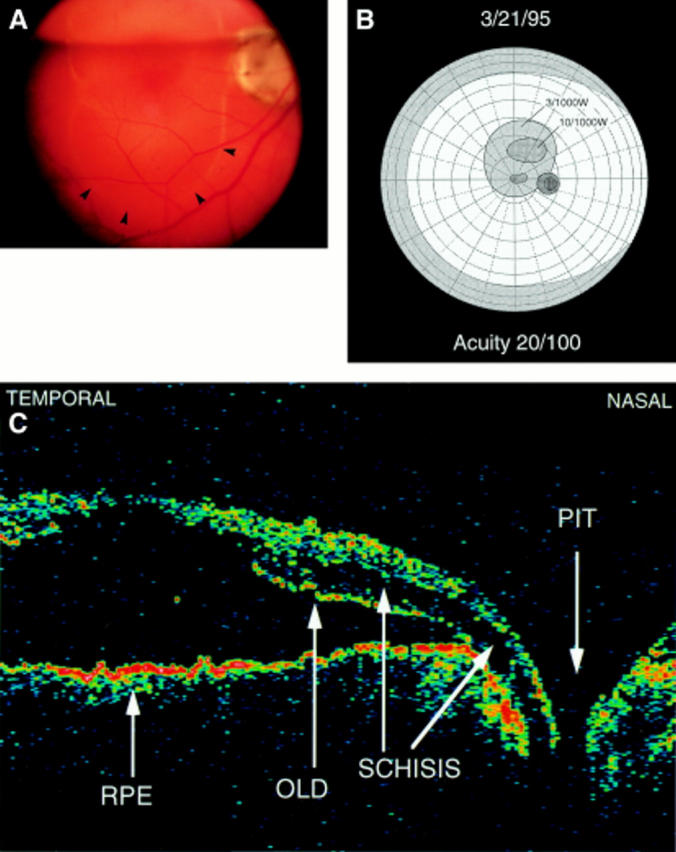
(A) Posterior pole (patient no 1) at 1 week after the injection of C2F6: the gas meniscus is at the upper border of the disc. The OLD has been displaced below the disc (arrowheads). (B) Central field at 1 week: It demonstrates a dense scotoma (10/1000W) consistent with the OLD, that has been displaced above the posterior pole. A less dense scotoma (3/1000W) is consistent with the extent of the ILS. (C) OCT of the posterior pole at 1 week. It reveals the retinal elevation diminished by half. The schisis-like cavity connects to the disc pit. The OLD attaches to the retinal pigment epithelium at the edge of the disc. RPE = retinal pigment epithelium; OLD = outer layer detachment; − horizontal section through macula and disc.
Figure 3 .
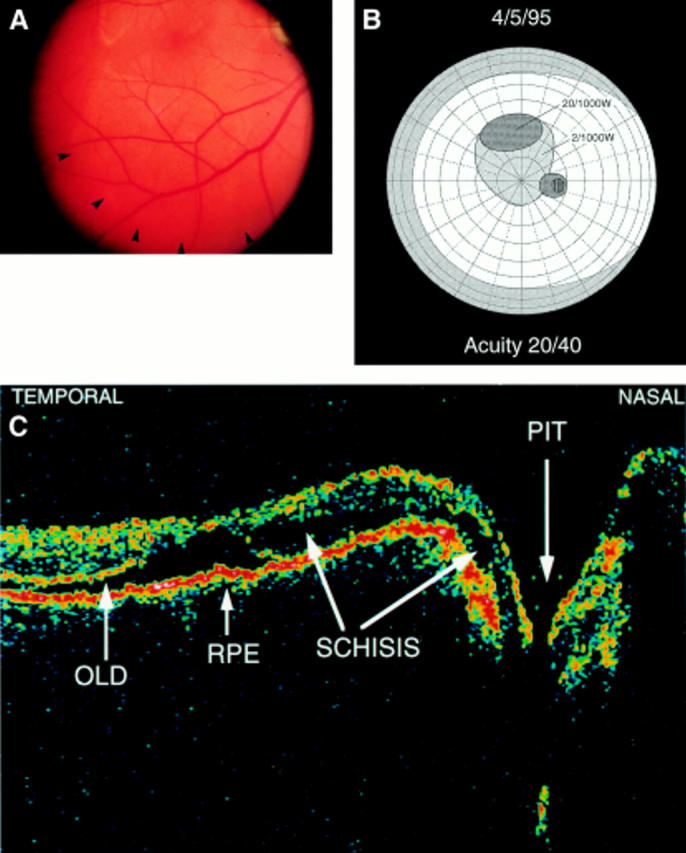
(A) Posterior pole (patient 1) at 3 weeks. The OLD is displaced below the inferior temporal vein (arrowheads). (B) Central visual field at 3 weeks. It demonstrates a dense scotoma (20/1000W) between 15° and 25° above fixation consistent with the OLD. A less dense scotoma (2/1000W) persists in the posterior pole. (C) OCT at 3 weeks. It reveals the retinal layers almost attached to the pigment epithelium. A hole in the OLD at the macula is apparent. The schisis-like cavity persists and is confluent with the optic disc pit. RPE = retinal pigment epithelium; OLD = outer layer detachment; − horizontal section through macula and disc.
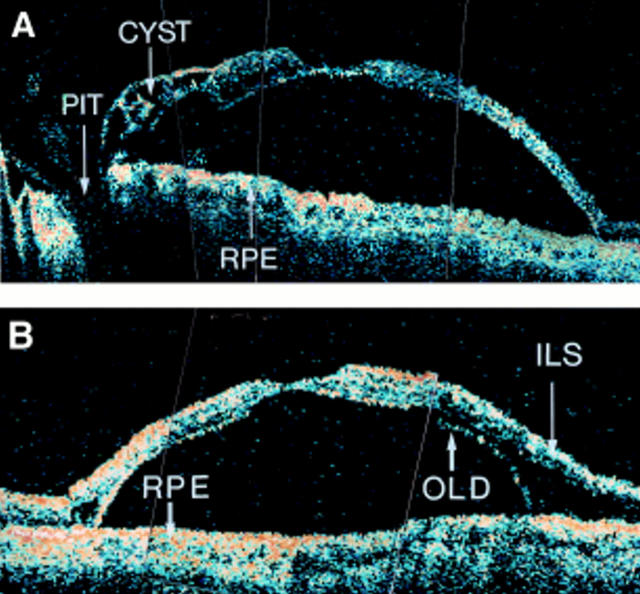
Figure 4 .
(A) OCT demonstrating recurrence of the OLD in patient no 3 five years after gas displacement. The OLD is in close approximation to the ILS except at its margins. Nasally the ILS is cystic. The visual acuity had diminished from 20/40 to 20/100. RPE = retinal pigment epithelium; − horizontal section through macula and disc. (B) Vertical section through the macula of patient no 3. RPE = retinal pigment epithelium; OLD = outer layer detachment; ILS = inner layer separation.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brockhurst R. J. Optic pits and posterior retinal detachment. Trans Am Ophthalmol Soc. 1975;73:264–291. [PMC free article] [PubMed] [Google Scholar]
- Brown G. C., Shields J. A., Patty B. E., Goldberg R. E. Congenital pits of the optic nerve head. I. Experimental studies in collie dogs. Arch Ophthalmol. 1979 Jul;97(7):1341–1344. doi: 10.1001/archopht.1979.01020020083020. [DOI] [PubMed] [Google Scholar]
- Huang D., Swanson E. A., Lin C. P., Schuman J. S., Stinson W. G., Chang W., Hee M. R., Flotte T., Gregory K., Puliafito C. A. Optical coherence tomography. Science. 1991 Nov 22;254(5035):1178–1181. doi: 10.1126/science.1957169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreissig I., Kamel H. The balloon-gas procedure: a technique for repair of retinal detachments requiring large volumes of gas. Eur J Ophthalmol. 1991 Jan-Mar;1(1):11–16. doi: 10.1177/112067219100100103. [DOI] [PubMed] [Google Scholar]
- Kreissig I. The balloon-gas-procedure. Another move towards minimum surgery. Dev Ophthalmol. 1987;13:99–106. [PubMed] [Google Scholar]
- Krivoy D., Gentile R., Liebmann J. M., Stegman Z., Rosen R., Walsh J. B., Ritch R. Imaging congenital optic disc pits and associated maculopathy using optical coherence tomography. Arch Ophthalmol. 1996 Feb;114(2):165–170. doi: 10.1001/archopht.1996.01100130159008. [DOI] [PubMed] [Google Scholar]
- Lincoff A., Haft D., Liggett P., Reifer C. Intravitreal expansion of perfluorocarbon bubbles. Arch Ophthalmol. 1980 Sep;98(9):1646–1646. doi: 10.1001/archopht.1980.01020040498023. [DOI] [PubMed] [Google Scholar]
- Lincoff H., Schiff W., Krivoy D., Ritch R. Optic coherence tomography of optic disk pit maculopathy. Am J Ophthalmol. 1996 Aug;122(2):264–266. doi: 10.1016/s0002-9394(14)72021-5. [DOI] [PubMed] [Google Scholar]
- Lincoff H., Yannuzzi L., Singerman L., Kreissig I., Fisher Y. Improvement in visual function after displacement of the retinal elevations emanating from optic pits. Arch Ophthalmol. 1993 Aug;111(8):1071–1079. doi: 10.1001/archopht.1993.01090080067020. [DOI] [PubMed] [Google Scholar]
- Puliafito C. A., Hee M. R., Lin C. P., Reichel E., Schuman J. S., Duker J. S., Izatt J. A., Swanson E. A., Fujimoto J. G. Imaging of macular diseases with optical coherence tomography. Ophthalmology. 1995 Feb;102(2):217–229. doi: 10.1016/s0161-6420(95)31032-9. [DOI] [PubMed] [Google Scholar]
- Rutledge B. K., Puliafito C. A., Duker J. S., Hee M. R., Cox M. S. Optical coherence tomography of macular lesions associated with optic nerve head pits. Ophthalmology. 1996 Jul;103(7):1047–1053. doi: 10.1016/s0161-6420(96)30568-x. [DOI] [PubMed] [Google Scholar]
- Sugar H. S. Congenital pits in the optic disc and their equivalents (congenital colobomas and colobomalike excavations) associated with submacular fluid. Am J Ophthalmol. 1967 Feb;63(2):298–307. [PubMed] [Google Scholar]