Abstract
AIM—To assess the dimensions and patency of the surgical epithelial fistula after external dacryocystorhinostomy, using B mode ultrasonography to define the postoperative soft tissue anastomosis. METHODS—12 patients undergoing 16 external dacryocystorhinostomies, with the creation of large osteotomies, were included in a prospective study. The horizontal and vertical dimensions of the bone ostium was recorded during surgery and compared with the ultrasonographic dimensions of the soft tissue anastomosis at 1 day, 2 weeks, and 6 months after surgery. Functional patency was confirmed with dye testing and irrigation. RESULTS—Compared with an osteotomy of between 100 and 380 mm2 (mean 235 mm2), the soft tissue anastomosis on the day after surgery was, in all cases, markedly smaller (72-252 mm2; mean 144 mm2, or 61% of the bone window). The soft tissue anastomosis decreased to between 8 and 208 mm2 (mean 98 mm2; 68% of immediate postoperative value) at 2 weeks and 3-208 mm2 (mean 71 mm2; 49% of immediate postoperative value) at 6 months. 14 of the 16 (88%) dacryocystorhinostomies were functional at the end of the study, the two failures being associated with marked contracture of the soft tissue anastomosis; the outcome of surgery correlated significantly with the area of the anastomosis at 2 weeks (χ2 = 16.3; p<0.01) and at 6 months (χ2= 16.0, p= 0.01). CONCLUSIONS—B mode ultrasonography provides a simple and effective method for assessing the size of the soft tissue anastomosis after external dacryocystorhinostomy and there is a significant reduction in size after surgery, to which the functional outcome of surgery appears related. As the initial soft tissue anastomosis cannot be larger than (and is, on average, about 60% of) the area of the osteotomy, this emphasises the paramount importance of a large rhinostomy to the success of lacrimal surgery. Keywords: ultrasonography; dacryocystorhinostomy; rhinostomy; healing
Full Text
The Full Text of this article is available as a PDF (135.0 KB).
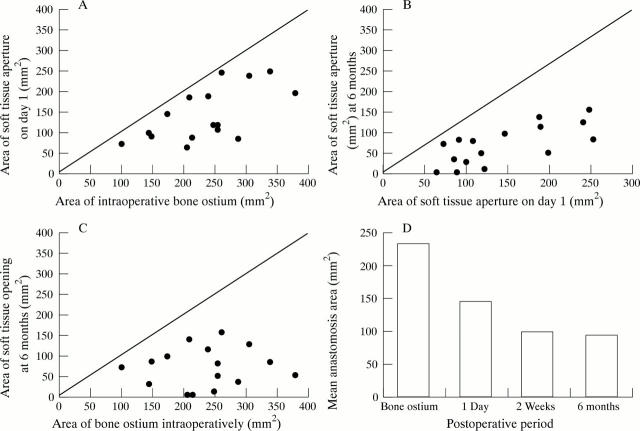
Figure 1 .
Change in the estimated area of the soft tissue anastomosis immediately after surgery in 16 dacrocystorhinostomies (DCRs) and (A) the bone window measured at surgery or (B) the soft tissue anastomosis when healed at 6 months. Likewise, the size of the fistula at 6 months is related to that immediately after surgery (C). The mean areas of the rhinostomy and the soft tissue anastomosis at 1 day, 2 weeks, and 6 months are compared, this showing that contracture of the mucosal fistula occurs mainly during the first 2 weeks after surgery (D). The oblique lines (A-C) represent the loci of equality, demonstrating that all anastomoses become smaller with time.
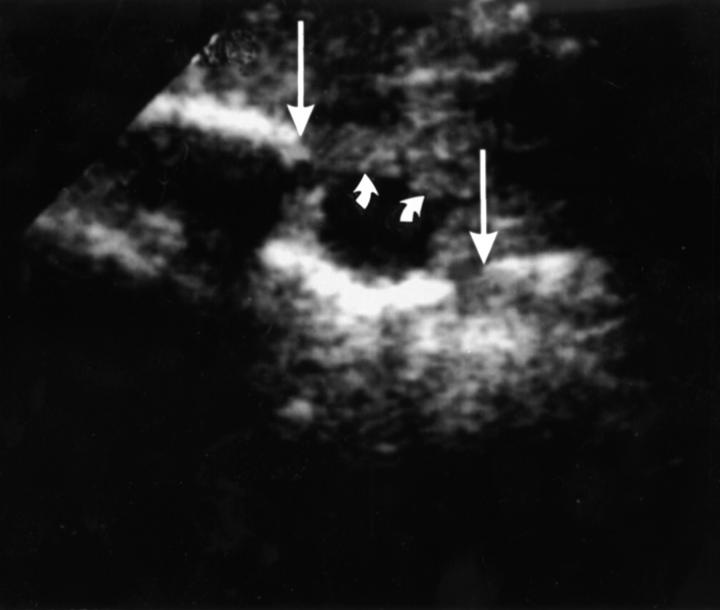
Figure 2 .
Preoperative ultrasound image (case 6) showing a dilated lacrimal sac (small arrows) and the vertical limits of the lacrimal sac fossa (large arrows).
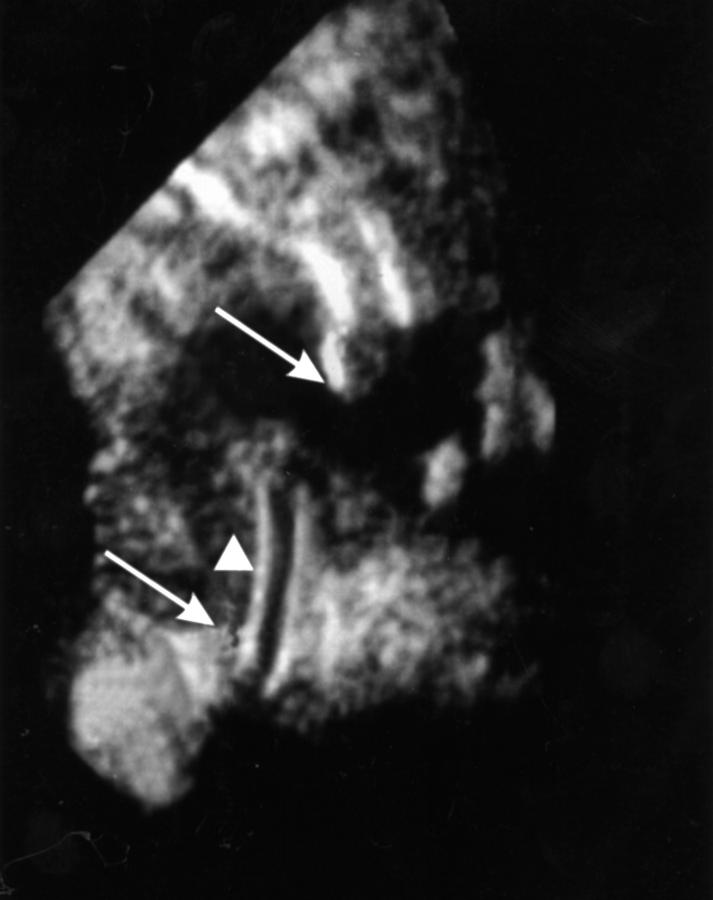
Figure 3 .
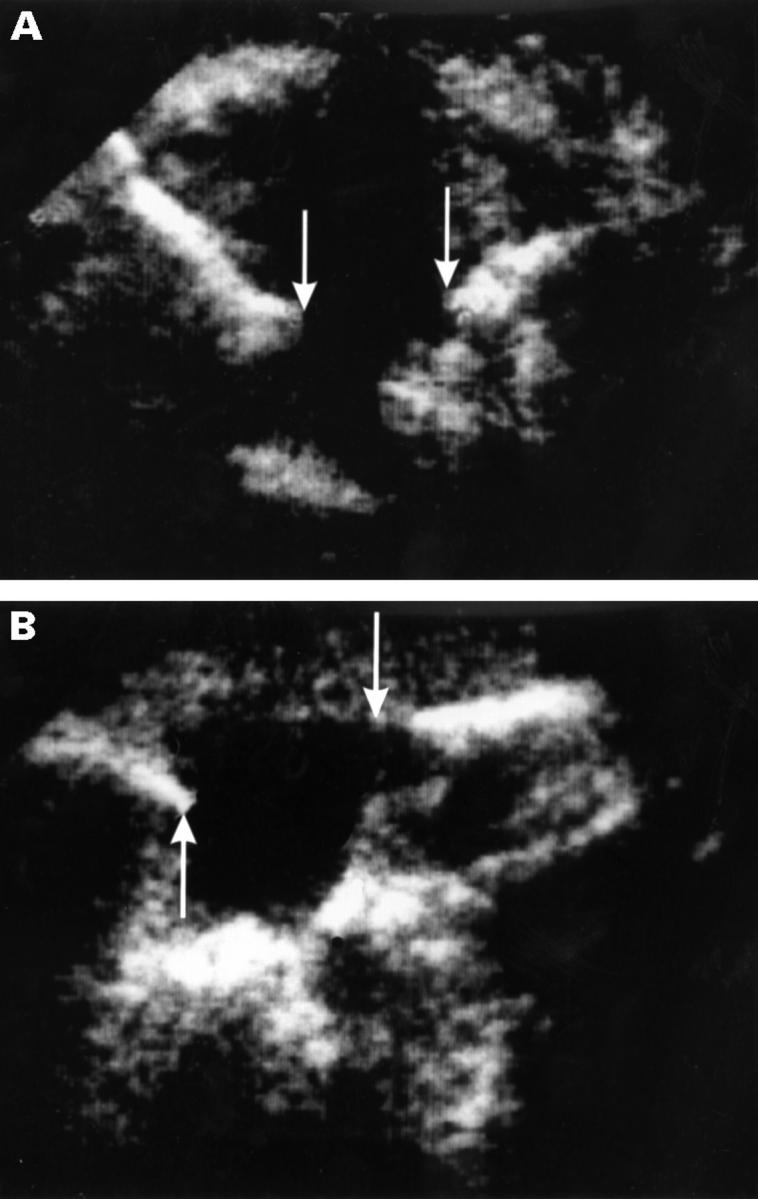
B mode ultrasonogram of the soft tissue anastomosis at 2 weeks after surgery (case 6) showing (A) the anteroposterior dimensions (8.0 mm; between arrows) and (B) the vertical dimensions (9.0 mm; between arrows).
Figure 4 .
Ultrasonogram of a postoperative anastomosis at 2 weeks (case 11, right side), showing vertical limits of 11.3 mm (arrows). A part of the silicone intubation (arrowhead) is seen to pass inferiorly through this plane of section.
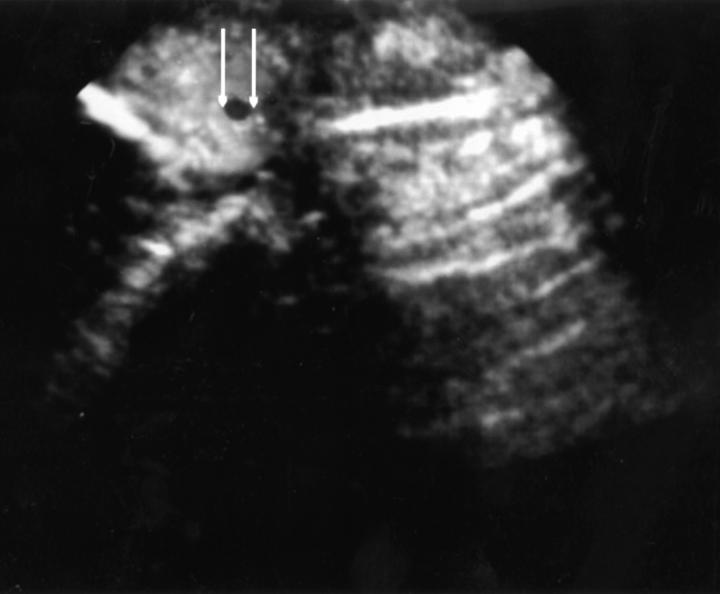
Figure 5 .
Failed anastomosis at 6 months after surgery (case 14), the vertical dimension of the soft tissue aperture being 2 mm (arrows).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson R. L., Edwards J. J. Indications, complications and results with silicone stents. Ophthalmology. 1979 Aug;86(8):1474–1487. doi: 10.1016/s0161-6420(79)35374-x. [DOI] [PubMed] [Google Scholar]
- Divine R. D., Anderson R. L., Bumsted R. M. Bilateral congenital lacrimal sac mucoceles with nasal extension and drainage. Arch Ophthalmol. 1983 Feb;101(2):246–248. doi: 10.1001/archopht.1983.01040010248013. [DOI] [PubMed] [Google Scholar]
- Dutton J. J. Standardized echography in the diagnosis of lacrimal drainage dysfunction. Arch Ophthalmol. 1989 Jul;107(7):1010–1012. doi: 10.1001/archopht.1989.01070020072032. [DOI] [PubMed] [Google Scholar]
- Jedrzynski M. S., Bullock J. D. Lacrimal ultrasonography. Ophthal Plast Reconstr Surg. 1994 Jun;10(2):114–120. doi: 10.1097/00002341-199406000-00008. [DOI] [PubMed] [Google Scholar]
- Linberg J. V., Anderson R. L., Bumsted R. M., Barreras R. Study of intranasal ostium external dacryocystorhinostomy. Arch Ophthalmol. 1982 Nov;100(11):1758–1762. doi: 10.1001/archopht.1982.01030040738005. [DOI] [PubMed] [Google Scholar]
- Montanara A., Mannino G., Contestabile M. T. Macrodacryocystography and echography in diagnosis of disorders of the lacrimal pathways. Surv Ophthalmol. 1983 Jul-Aug;28(1):33–41. doi: 10.1016/0039-6257(83)90176-5. [DOI] [PubMed] [Google Scholar]
- OKSALA A. Diagnosis by ultrasound in acute dacryocystitis. Acta Ophthalmol (Copenh) 1959;37(2):176–179. doi: 10.1111/j.1755-3768.1959.tb03421.x. [DOI] [PubMed] [Google Scholar]
- Picó G. A modified technique of external dacryocystorhinostomy. Am J Ophthalmol. 1971 Oct;72(4):679–690. doi: 10.1016/0002-9394(71)90001-8. [DOI] [PubMed] [Google Scholar]
- Rosen N., Sharir M., Moverman D. C., Rosner M. Dacryocystorhinostomy with silicone tubes: evaluation of 253 cases. Ophthalmic Surg. 1989 Feb;20(2):115–119. [PubMed] [Google Scholar]
- Scott W. E., Fabre J. A., Ossoinig K. C. Congenital mucocele of the lacrimal sac. Arch Ophthalmol. 1979 Sep;97(9):1656–1658. doi: 10.1001/archopht.1979.01020020224008. [DOI] [PubMed] [Google Scholar]
- Walland M. J., Rose G. E. Factors affecting the success rate of open lacrimal surgery. Br J Ophthalmol. 1994 Dec;78(12):888–891. doi: 10.1136/bjo.78.12.888. [DOI] [PMC free article] [PubMed] [Google Scholar]