Abstract
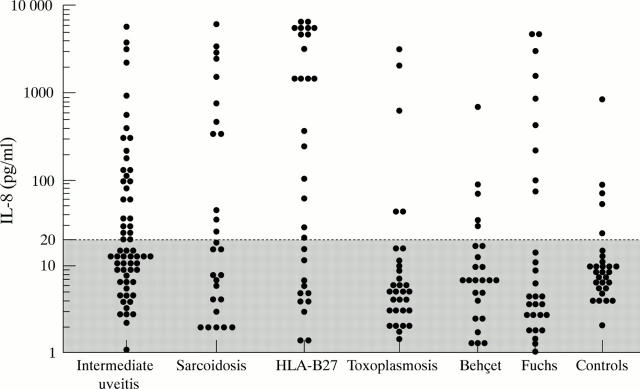
AIM—To find a laboratory indicator for systemic involvement in intermediate uveitis. METHODS—Interleukin 8 (IL-8) and C reactive protein (CRP) serum levels were measured in patients with idiopathic intermediate uveitis (n=61), uveitis controls (n=143), and normal controls (n=29). The records of those with intermediate uveitis were reviewed with the emphasis on disease activity and severity as characterised by the presence of cystoid macular oedema, vitreous exudates or snowbank formation, papillitis, and periphlebitis. RESULTS—Increased serum IL-8 (⩾20 pg/ml) was found in 27 out of 61 patients with intermediate uveitis (p< 0.01), 12 of 27 patients with sarcoid uveitis (p<0.05), in 19 of 30 patients with HLA-B27 associated acute anterior uveitis (p<0.05), and in five of 29 healthy controls. Raised IL-8 levels in intermediate uveitis were significantly associated with active disease (p<0.001) and the presence of vitreous exudates (p<0.001), papillitis, and periphlebitis (p<0.01). Elevated CRP levels were found in 12 of the 143 uveitis controls but in none of the intermediate uveitis patients or normal controls. During follow up an associated systemic disease was more frequently noticed in patients with an elevated serum IL-8 at entry into the study. CONCLUSIONS—Elevated IL-8 serum levels were found in patients with active intermediate uveitis of unknown origin. An elevated IL-8 level seems to predispose the patient to a later development of associated systemic disease. Keywords: C reactive protein; interleukin 8; uveitis; multiple sclerosis; sarcoidosis
Full Text
The Full Text of this article is available as a PDF (105.4 KB).
Figure 1 .
IL-8 levels in serum from intermediate uveitis patients, uveitis controls, and normal controls. The broken line represents the detection limit of the assay.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arocker-Mettinger E., Steurer-Georgiew L., Steurer M., Huber-Spitzy V., Hoelzl E., Grabner G., Kuchar A. Circulating ICAM-1 levels in serum of uveitis patients. Curr Eye Res. 1992;11 (Suppl):161–166. doi: 10.3109/02713689208999527. [DOI] [PubMed] [Google Scholar]
- Baggiolini M., Walz A., Kunkel S. L. Neutrophil-activating peptide-1/interleukin 8, a novel cytokine that activates neutrophils. J Clin Invest. 1989 Oct;84(4):1045–1049. doi: 10.1172/JCI114265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bamford C. R., Ganley J. P., Sibley W. A., Laguna J. F. Uveitis, perivenous sheathing and multiple sclerosis. Neurology. 1978 Sep;28(9 Pt 2):119–124. doi: 10.1212/wnl.28.9_part_2.119. [DOI] [PubMed] [Google Scholar]
- Bloch-Michel E., Nussenblatt R. B. International Uveitis Study Group recommendations for the evaluation of intraocular inflammatory disease. Am J Ophthalmol. 1987 Feb 15;103(2):234–235. doi: 10.1016/s0002-9394(14)74235-7. [DOI] [PubMed] [Google Scholar]
- Bora N. S., Bora P. S., Kaplan H. J. Identification, quantitation, and purification of a 36 kDa circulating protein associated with active pars planitis. Invest Ophthalmol Vis Sci. 1996 Aug;37(9):1870–1876. [PubMed] [Google Scholar]
- Diamond G. Ocular manifestations of genetic and developmental diseases. Curr Opin Ophthalmol. 1994 Dec;5(6):72–78. doi: 10.1097/00055735-199412000-00012. [DOI] [PubMed] [Google Scholar]
- Elner V. M., Strieter R. M., Elner S. G., Baggiolini M., Lindley I., Kunkel S. L. Neutrophil chemotactic factor (IL-8) gene expression by cytokine-treated retinal pigment epithelial cells. Am J Pathol. 1990 Apr;136(4):745–750. [PMC free article] [PubMed] [Google Scholar]
- Hack C. E., Hart M., van Schijndel R. J., Eerenberg A. J., Nuijens J. H., Thijs L. G., Aarden L. A. Interleukin-8 in sepsis: relation to shock and inflammatory mediators. Infect Immun. 1992 Jul;60(7):2835–2842. doi: 10.1128/iai.60.7.2835-2842.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderly D. E., Genstler A. J., Rao N. A., Smith R. E. Pars planitis. Trans Ophthalmol Soc U K. 1986;105(Pt 2):227–232. [PubMed] [Google Scholar]
- Kilpatrick J. M., Volanakis J. E. Molecular genetics, structure, and function of C-reactive protein. Immunol Res. 1991;10(1):43–53. doi: 10.1007/BF02918166. [DOI] [PubMed] [Google Scholar]
- Kolb-Bachofen V. A review on the biological properties of C-reactive protein. Immunobiology. 1991 Sep;183(1-2):133–145. doi: 10.1016/S0171-2985(11)80193-2. [DOI] [PubMed] [Google Scholar]
- Leonard E. J., Yoshimura T. Neutrophil attractant/activation protein-1 (NAP-1 [interleukin-8]). Am J Respir Cell Mol Biol. 1990 Jun;2(6):479–486. doi: 10.1165/ajrcmb/2.6.479. [DOI] [PubMed] [Google Scholar]
- Mahida Y. R., Ceska M., Effenberger F., Kurlak L., Lindley I., Hawkey C. J. Enhanced synthesis of neutrophil-activating peptide-1/interleukin-8 in active ulcerative colitis. Clin Sci (Lond) 1992 Mar;82(3):273–275. doi: 10.1042/cs0820273. [DOI] [PubMed] [Google Scholar]
- Malinowski S. M., Pulido J. S., Folk J. C. Long-term visual outcome and complications associated with pars planitis. Ophthalmology. 1993 Jun;100(6):818–825. doi: 10.1016/s0161-6420(93)31567-8. [DOI] [PubMed] [Google Scholar]
- Steel D. M., Whitehead A. S. The major acute phase reactants: C-reactive protein, serum amyloid P component and serum amyloid A protein. Immunol Today. 1994 Feb;15(2):81–88. doi: 10.1016/0167-5699(94)90138-4. [DOI] [PubMed] [Google Scholar]
- Strieter R. M., Kunkel S. L., Elner V. M., Martonyi C. L., Koch A. E., Polverini P. J., Elner S. G. Interleukin-8. A corneal factor that induces neovascularization. Am J Pathol. 1992 Dec;141(6):1279–1284. [PMC free article] [PubMed] [Google Scholar]
- Tang W. M., Pulido J. S., Eckels D. D., Han D. P., Mieler W. F., Pierce K. The association of HLA-DR15 and intermediate uveitis. Am J Ophthalmol. 1997 Jan;123(1):70–75. doi: 10.1016/s0002-9394(14)70994-8. [DOI] [PubMed] [Google Scholar]
- Yokoyama T., Kanda T., Kobayashi I., Suzuki T. Serum levels of interleukin-8 as a marker of disease activity in patients with chronic sarcoidosis. J Med. 1995;26(5-6):209–219. [PubMed] [Google Scholar]
- Zierhut M., Foster C. S. Multiple sclerosis, sarcoidosis and other diseases in patients with pars planitis. Dev Ophthalmol. 1992;23:41–47. doi: 10.1159/000429628. [DOI] [PubMed] [Google Scholar]
- de Boer J. H., Hack C. E., Verhoeven A. J., Baarsma G. S., de Jong P. T., Rademakers A. J., de Vries-Knoppert W. A., Rothova A., Kijlstra A. Chemoattractant and neutrophil degranulation activities related to interleukin-8 in vitreous fluid in uveitis and vitreoretinal disorders. Invest Ophthalmol Vis Sci. 1993 Nov;34(12):3376–3385. [PubMed] [Google Scholar]