Abstract
BACKGROUND/AIM—Elevated plasma homocysteine is a newly identified vascular risk factor among patients under age 55 years with cerebrovascular, cardiovascular, or peripheral vascular disease. This study sought to evaluate retrospectively the plasma homocysteine status among healthy younger patients with ischaemic optic disc disease. METHODS—12 non-diabetic patients who had been diagnosed with non-arteritic anterior ischaemic optic neuropathy (NAION) before the age of 50 years were identified from chart review. None had experienced previous ischaemic cerebrovascular, cardiovascular, or peripheral vascular events. Plasma homocysteine, CBC, renal function, vitamin B6, vitamin B12, and folate levels were sampled in the fasting state. RESULTS—Two of 12 patients (17%) had hyperhomocysteinaemia. Both had experienced NAION in both eyes with recurrent episodes. Neither patient was hypertensive nor had a smoking history. One of these two patients had mild hypercholesterolaemia which did not warrant medication. CONCLUSIONS—Elevated plasma homocysteine may be associated with NAION. An evaluation for hyperhomocysteinaemia should be considered in patients with NAION who do not have the typical risk factor such as older age, diabetes, hypertension, or tobacco use. It should also be considered in young patients with bilateral or recurrent attacks of NAION.
Full Text
The Full Text of this article is available as a PDF (74.3 KB).
Figure 1 .
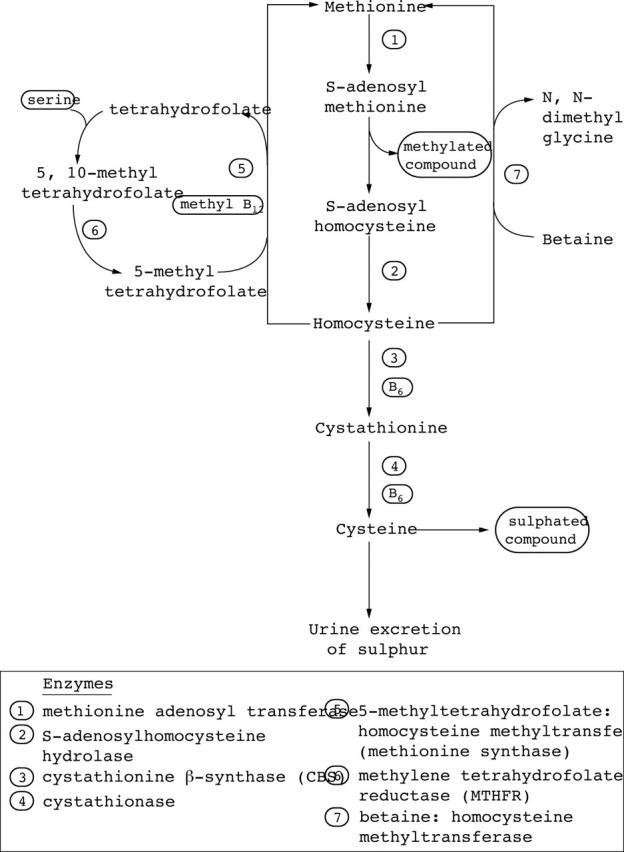
Metabolic pathway of homocysteine.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Biousse V., Newman N. J., Sternberg P., Jr Retinal vein occlusion and transient monocular visual loss associated with hyperhomocystinemia. Am J Ophthalmol. 1997 Aug;124(2):257–260. doi: 10.1016/s0002-9394(14)70800-1. [DOI] [PubMed] [Google Scholar]
- Boushey C. J., Beresford S. A., Omenn G. S., Motulsky A. G. A quantitative assessment of plasma homocysteine as a risk factor for vascular disease. Probable benefits of increasing folic acid intakes. JAMA. 1995 Oct 4;274(13):1049–1057. doi: 10.1001/jama.1995.03530130055028. [DOI] [PubMed] [Google Scholar]
- Clarke R., Daly L., Robinson K., Naughten E., Cahalane S., Fowler B., Graham I. Hyperhomocysteinemia: an independent risk factor for vascular disease. N Engl J Med. 1991 Apr 25;324(17):1149–1155. doi: 10.1056/NEJM199104253241701. [DOI] [PubMed] [Google Scholar]
- Coull B. M., Malinow M. R., Beamer N., Sexton G., Nordt F., de Garmo P. Elevated plasma homocyst(e)ine concentration as a possible independent risk factor for stroke. Stroke. 1990 Apr;21(4):572–576. doi: 10.1161/01.str.21.4.572. [DOI] [PubMed] [Google Scholar]
- D'Angelo A., Selhub J. Homocysteine and thrombotic disease. Blood. 1997 Jul 1;90(1):1–11. [PubMed] [Google Scholar]
- Engbersen A. M., Franken D. G., Boers G. H., Stevens E. M., Trijbels F. J., Blom H. J. Thermolabile 5,10-methylenetetrahydrofolate reductase as a cause of mild hyperhomocysteinemia. Am J Hum Genet. 1995 Jan;56(1):142–150. [PMC free article] [PubMed] [Google Scholar]
- Jacques P. F., Bostom A. G., Williams R. R., Ellison R. C., Eckfeldt J. H., Rosenberg I. H., Selhub J., Rozen R. Relation between folate status, a common mutation in methylenetetrahydrofolate reductase, and plasma homocysteine concentrations. Circulation. 1996 Jan 1;93(1):7–9. doi: 10.1161/01.cir.93.1.7. [DOI] [PubMed] [Google Scholar]
- Loewenstein A., Winder A., Goldstein M., Lazar M., Eldor A. Bilateral retinal vein occlusion associated with 5,10-methylenetetrahydrofolate reductase mutation. Am J Ophthalmol. 1997 Dec;124(6):840–841. doi: 10.1016/s0002-9394(14)71703-9. [DOI] [PubMed] [Google Scholar]
- Mayer E. L., Jacobsen D. W., Robinson K. Homocysteine and coronary atherosclerosis. J Am Coll Cardiol. 1996 Mar 1;27(3):517–527. doi: 10.1016/0735-1097(95)00508-0. [DOI] [PubMed] [Google Scholar]
- Selhub J., Jacques P. F., Wilson P. W., Rush D., Rosenberg I. H. Vitamin status and intake as primary determinants of homocysteinemia in an elderly population. JAMA. 1993 Dec 8;270(22):2693–2698. doi: 10.1001/jama.1993.03510220049033. [DOI] [PubMed] [Google Scholar]
- Stampfer M. J., Malinow M. R., Willett W. C., Newcomer L. M., Upson B., Ullmann D., Tishler P. V., Hennekens C. H. A prospective study of plasma homocyst(e)ine and risk of myocardial infarction in US physicians. JAMA. 1992 Aug 19;268(7):877–881. [PubMed] [Google Scholar]
- Wenzler E. M., Rademakers A. J., Boers G. H., Cruysberg J. R., Webers C. A., Deutman A. F. Hyperhomocysteinemia in retinal artery and retinal vein occlusion. Am J Ophthalmol. 1993 Feb 15;115(2):162–167. doi: 10.1016/s0002-9394(14)73919-4. [DOI] [PubMed] [Google Scholar]
- den Heijer M., Koster T., Blom H. J., Bos G. M., Briet E., Reitsma P. H., Vandenbroucke J. P., Rosendaal F. R. Hyperhomocysteinemia as a risk factor for deep-vein thrombosis. N Engl J Med. 1996 Mar 21;334(12):759–762. doi: 10.1056/NEJM199603213341203. [DOI] [PubMed] [Google Scholar]


