Abstract
AIMS—To describe a new surgical technique for deep stromal anterior lamellar keratoplasty. METHODS—In eye bank eyes and sighted human eyes, aqueous was exchanged by air, to visualise the posterior corneal surface−that is, the "air to endothelium" interface. Through a 5.0 mm scleral incision, a deep stromal pocket was created across the cornea, using the air to endothelium interface as a reference plane for dissection depth. The pocket was filled with viscoelastic, and an anterior corneal lamella was excised. A full thickness donor button was sutured into the recipient bed after stripping its Descemet's membrane. RESULTS—In 25 consecutive human eye bank eyes, a 12% microperforation rate was found. Corneal dissection depth averaged 95.4% (SD 2.7%). Six patient eyes had uneventful surgeries; in a seventh eye, perforation of the lamellar bed occurred. All transplants cleared. Central pachymetry ranged from 0.62 to 0.73 mm. CONCLUSION—With this technique a deep stromal anterior lamellar keratoplasty can be performed with the donor to recipient interface just anterior to the posterior corneal surface. The technique has the advantage that the dissection can be completed in the event of inadvertent microperforation, or that the procedure can be aborted to perform a planned penetrating keratoplasty. Keywords: corneal surgery; lamellar keratoplasty; air; optical interface
Full Text
The Full Text of this article is available as a PDF (187.5 KB).
Figure 1 .
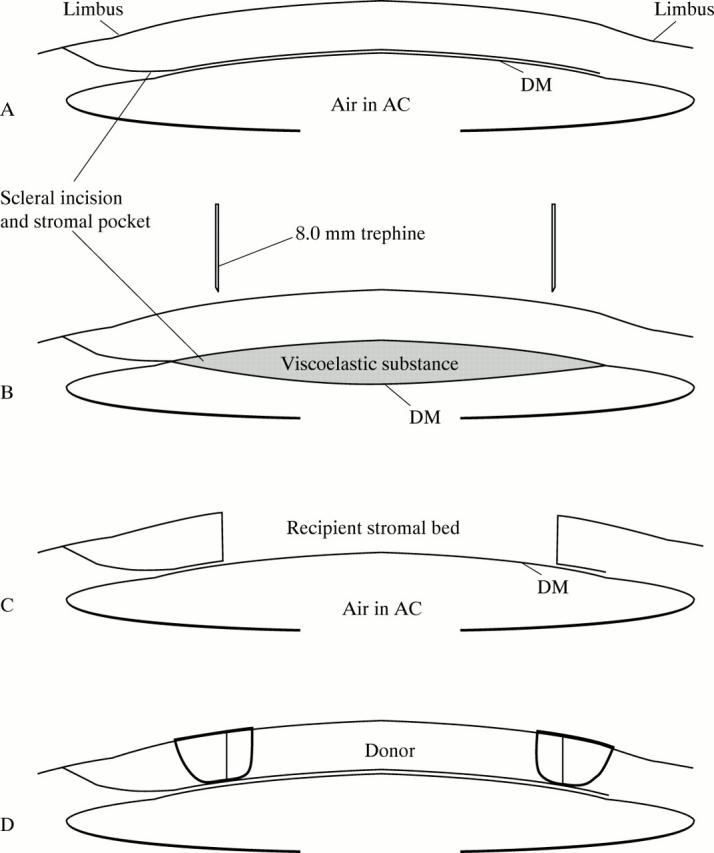
Diagrammatic representation of the deep, anterior lamellar keratoplasty technique. (A) After dissection of a deep stromal pocket through a scleral incision. (B and C) Viscoelastic is injected into the pocket, and an anterior corneal lamella is trephinated from the recipient cornea. (D) After stripping Descemet's membrane, a full thickness donor corneal button is sutured into the recipient stromal bed. Compare with Figures 2A-C and 3A-F.
Figure 2 .
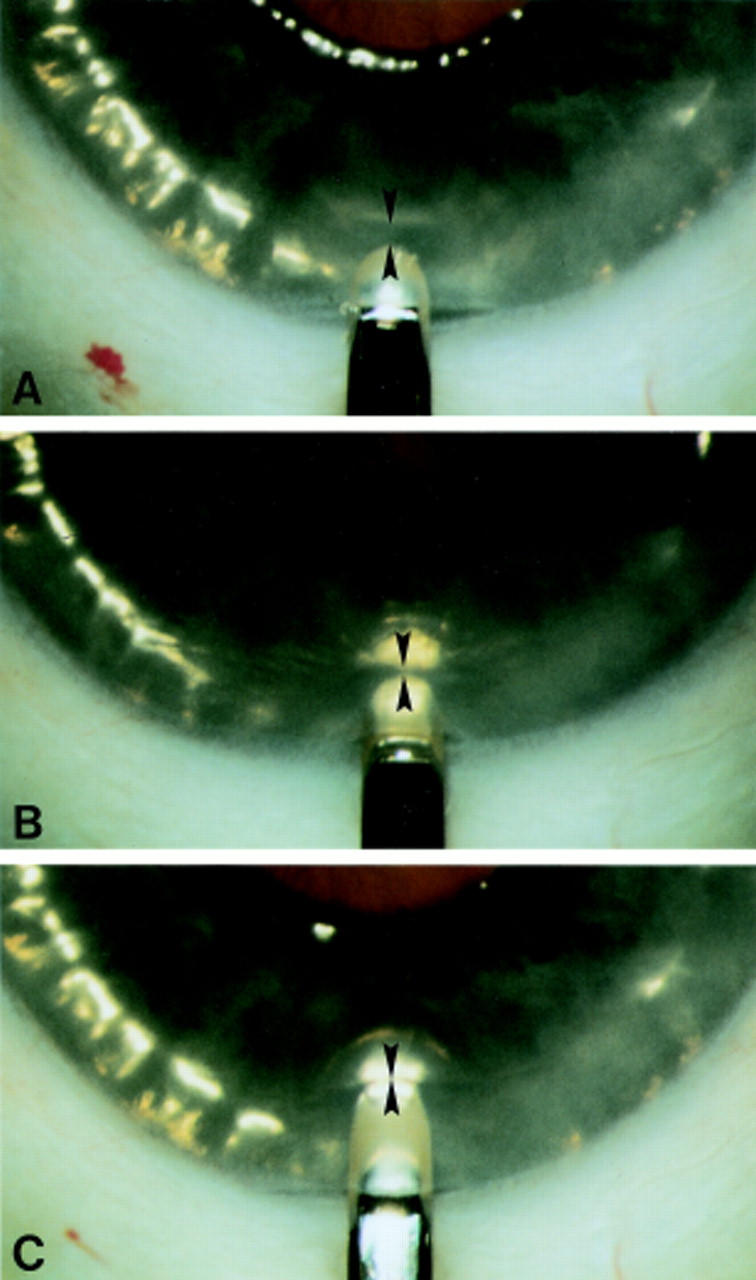
Demonstration of the surgical technique in a human eye bank eye. (A) The anterior chamber has been filled with air. In between the blade tip and the air to endothelial interface light reflex, a dark band (arrowheads) is visible. (B) Because the dark band reflects unincised posterior corneal tissue, the dark band decreases in width when the blade is advanced into the deeper stromal layers. (C) When the blade appears to touch the air to endothelium interface, a stromal dissection level just anterior to the posterior corneal surface is reached.
Figure 3 .
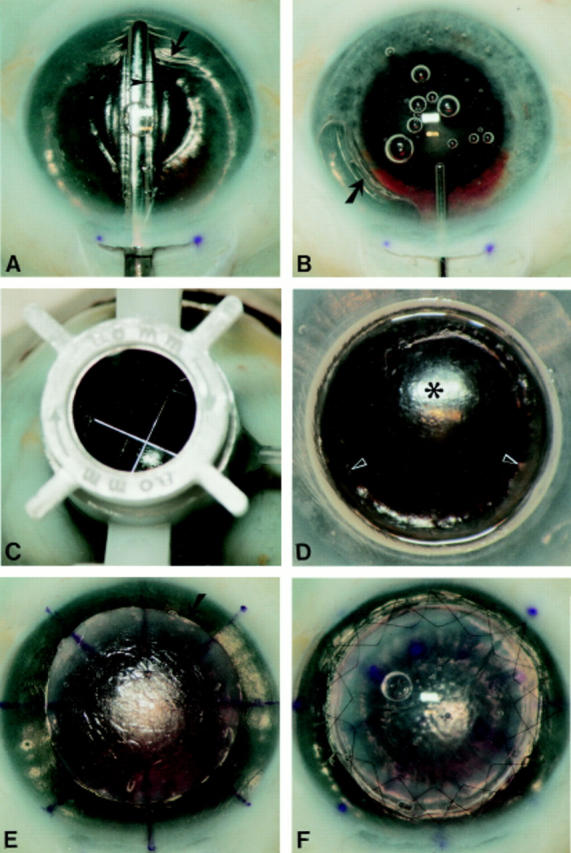
Demonstration of the surgical technique in a human eye bank eye. (A) The pocket is dissected first across the vertical meridian, and then extended sideways up to the limbus over 360°, with the same spatula. Note that the anterior chamber is completely filled with air, and that the dissection depth can be monitored by the width of the dark band (arrowhead) in between the spatula and the air to endothelium light reflex. Note also the wrinkling of the posterior corneal tissue (arrow). (B) After most air has been removed from the anterior chamber, the stromal pocket is filled with viscoelastic. Note the step ladder configuration of the relaxed posterior corneal tissue (arrow) which is pushed downward. (C) After trephination with a Hessburg-Barron trephine (D) an anterior corneal lamella is excised. Note the smooth recipient bed (asterisk) with some residual posterior stroma overlying the pupillary border (arrowheads). Pupillary dilatation was not intended as a part of the procedure. (E) After stripping Descemet's membrane, a "full thickness" donor button (arrow) is placed onto the recipient bed, and the donor and recipient corneal surfaces are marked with an eight incision radial keratotomy marker. (F) The donor button sutured in place with two running sutures. Pupillary dilatation was not an intended part of the procedure.
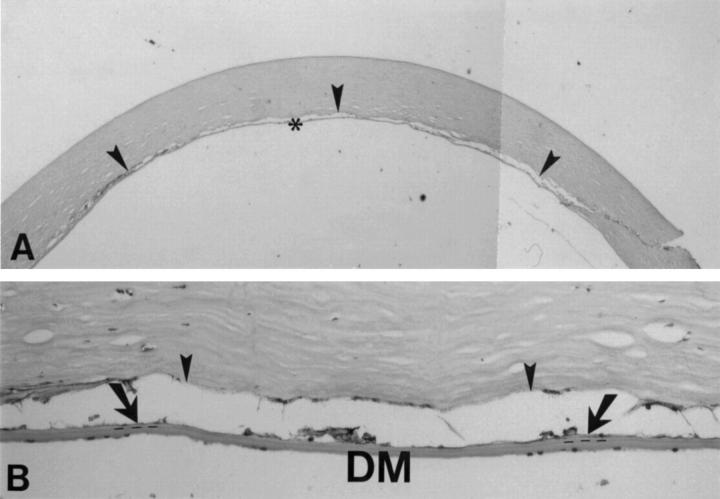
Figure 4 .
Light microscopy of a deep lamellar dissection through a scleral incision in a human eye bank eye. (A) A deep stromal dissection level (arrowheads) is seen (98% corneal depth). (B) Few stromal lamellae (arrows) are visible between the stromal dissection and Descemet's membrane; the dotted line indicates the junction of the stroma and Descemet's membrane (haematoxylin and eosin, original magnification ×35 and ×450).
Figure 5 .
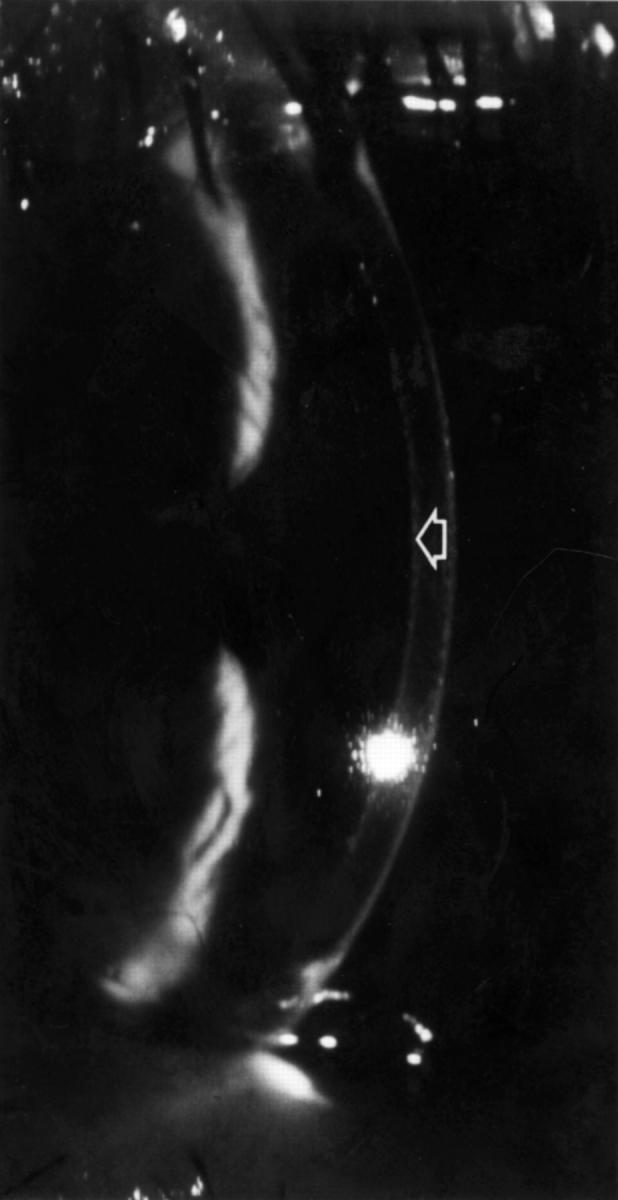
Slit lamp photograph 6 months (patient eye 1) after deep, anterior lamellar keratoplasty. A clear lamellar corneal transplant is visible, with a deep stromal, donor to recipient interface (arrow).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anwar M. Dissection technique in lamellar keratoplasty. Br J Ophthalmol. 1972 Sep;56(9):711–713. doi: 10.1136/bjo.56.9.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Archila E. A. Deep lamellar keratoplasty dissection of host tissue with intrastromal air injection. Cornea. 1984;3(3):217–218. [PubMed] [Google Scholar]
- Barraquer J. I. Lamellar keratoplasty. (Special techniques). Ann Ophthalmol. 1972 Jun;4(6):437–469. [PubMed] [Google Scholar]
- Benson W. H., Goosey C. B., Prager T. C., Goosey J. D. Visual improvement as a function of time after lamellar keratoplasty for keratoconus. Am J Ophthalmol. 1993 Aug 15;116(2):207–211. doi: 10.1016/s0002-9394(14)71287-5. [DOI] [PubMed] [Google Scholar]
- Bessant D. A., Dart J. K. Lamellar keratoplasty in the management of inflammatory corneal ulceration and perforation. Eye (Lond) 1994;8(Pt 1):22–28. doi: 10.1038/eye.1994.4. [DOI] [PubMed] [Google Scholar]
- Chau G. K., Dilly S. A., Sheard C. E., Rostron C. K. Deep lamellar keratoplasty on air with lyophilised tissue. Br J Ophthalmol. 1992 Nov;76(11):646–650. doi: 10.1136/bjo.76.11.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckhardt H. B., Hütz W. W., Heinrich A. W., Kaiser W. E. Lamellierende Keratoplastik mit dem Excimerlaser. Erste klinische Ergebnisse. Ophthalmologe. 1996 Jun;93(3):242–246. [PubMed] [Google Scholar]
- Ehrlich M. I., Phinney R. B., Mondino B. J., Pettit T. H. Techniques of lamellar keratoplasty. Int Ophthalmol Clin. 1988 Spring;28(1):24–29. doi: 10.1097/00004397-198802810-00004. [DOI] [PubMed] [Google Scholar]
- Eiferman R. A., Wilkins E. L. The effect of air on human corneal endothelium. Am J Ophthalmol. 1981 Sep;92(3):328–331. doi: 10.1016/0002-9394(81)90520-1. [DOI] [PubMed] [Google Scholar]
- Gasset A. R. Lamellar keratoplasty in the treatment of keratoconus: conectomy. Ophthalmic Surg. 1979 Feb;10(2):26–33. [PubMed] [Google Scholar]
- Khodadoust A. A., Silverstein A. M. Transplantation and rejection of individual cell layers of the cornea. Invest Ophthalmol. 1969 Apr;8(2):180–195. [PubMed] [Google Scholar]
- Kim E. K., Cristol S. M., Geroski D. H., McCarey B. E., Edelhauser H. F. Corneal endothelial damage by air bubbles during phacoemulsification. Arch Ophthalmol. 1997 Jan;115(1):81–88. doi: 10.1001/archopht.1997.01100150083014. [DOI] [PubMed] [Google Scholar]
- Krumeich J. H., Daniel J. Lebend-Epikeratophakie und Tiefe Lamelläre Keratoplastik zur Stadiengerechten chirurgischen Behandlung des Keratokonus (KK) I-III. Klin Monbl Augenheilkd. 1997 Aug;211(2):94–100. doi: 10.1055/s-2008-1035103. [DOI] [PubMed] [Google Scholar]
- Lyons C. J., McCartney A. C., Kirkness C. M., Ficker L. A., Steele A. D., Rice N. S. Granular corneal dystrophy. Visual results and pattern of recurrence after lamellar or penetrating keratoplasty. Ophthalmology. 1994 Nov;101(11):1812–1817. doi: 10.1016/s0161-6420(94)31096-7. [DOI] [PubMed] [Google Scholar]
- Melles G. R., Eggink F. A., Lander F., Pels E., Rietveld F. J., Beekhuis W. H., Binder P. S. A surgical technique for posterior lamellar keratoplasty. Cornea. 1998 Nov;17(6):618–626. doi: 10.1097/00003226-199811000-00010. [DOI] [PubMed] [Google Scholar]
- Melles G. R., Wijdh R. H., Cost B., Beekhuis W. H., Binder P. S., van Rij G., Groot K. Effect of blade configuration, knife action, and intraocular pressure on keratotomy incision depth and shape. Cornea. 1993 Jul;12(4):299–309. doi: 10.1097/00003226-199307000-00005. [DOI] [PubMed] [Google Scholar]
- Melles G. R., ten Hoope G. W., Rietveld F. J., Beekhuis W. H., Binder P. S. Depth predictability of stromal pockets in the posterior cornea. Cornea. 1998 Mar;17(2):174–179. doi: 10.1097/00003226-199803000-00010. [DOI] [PubMed] [Google Scholar]
- Morrison J. C., Swan K. C. Full-thickness lamellar keratoplasty. A histologic study in human eyes. Ophthalmology. 1982 Jun;89(6):715–719. doi: 10.1016/s0161-6420(82)34749-1. [DOI] [PubMed] [Google Scholar]
- Polack F. M. Lamellar keratoplasty. Malbran's "peeling off" technique. Arch Ophthalmol. 1971 Sep;86(3):293–295. doi: 10.1001/archopht.1971.01000010295010. [DOI] [PubMed] [Google Scholar]
- Price F. W., Jr Air lamellar keratoplasty. Refract Corneal Surg. 1989 Jul-Aug;5(4):240–243. [PubMed] [Google Scholar]
- Rich L. F., MacRae S. M., Fraunfelder F. T. An improved method for lamellar keratoplasty. CLAO J. 1988 Jan-Mar;14(1):42–46. [PubMed] [Google Scholar]
- Richard J. M., Paton D., Gasset A. R. A comparison of penetrating keratoplasty and lamellar keratoplasty in the surgical management of keratoconus. Am J Ophthalmol. 1978 Dec;86(6):807–811. doi: 10.1016/0002-9394(78)90126-5. [DOI] [PubMed] [Google Scholar]
- Sugita J., Kondo J. Deep lamellar keratoplasty with complete removal of pathological stroma for vision improvement. Br J Ophthalmol. 1997 Mar;81(3):184–188. doi: 10.1136/bjo.81.3.184. [DOI] [PMC free article] [PubMed] [Google Scholar]