Abstract
AIM—To present the clinical profile of a new entity in advanced proliferative diabetic vitreoretinopathy (PDVR). Mechanisms of vision loss due to vitreopapillary traction on the nasal optic disc are described, followed by an introduction of methods for prevention and treatment in such cases. METHODS—17 patients with PDVR and traction on the nasal side of the optic disc, pallor of the optic nerve head, and reduced visual acuity were included in the study. Six patients were observed retrospectively and 11 patients prospectively before and after pars plana vitrectomy. Pre- and postoperative examinations included visual acuity, Goldmann's visual field, fluorescein angiography, and measurements of visual evoked potentials (VEP). RESULTS—During a postoperative follow up period of 3 to 24.5 months (mean 14.5 months) an improvement in optic disc appearance combined with an increased visual acuity (mean increase in VA = 0.171) was observed in 15/17 (88.3%) patients. In addition, 8/17 (47%) of these patients showed higher VEP amplitudes (mean 3.83 µV), and eight (6/8 of the same patients as VEP amplitudes) patients showed a reduction of latency (mean reduction 22.25 ms) during VEP assessment. CONCLUSION—These results suggest that vitreopapillary traction may damage the anterior optic nerve, via decreased axoplasmatic flow in the optic nerve fibres and/or mechanical reduction of perfusion in the posterior ciliary arteries. The effects of each mechanism appear to be reversible, but in the long term might lead to irreversible optic nerve atrophy. Therefore, in patients with vitreopapillary traction, early vitrectomy should be considered as a method to prevent optic neuropathy. Keywords: diabetic vitreopapillary traction; proliferative diabetic vitreoretinopathy; vitrectomy
Full Text
The Full Text of this article is available as a PDF (135.1 KB).
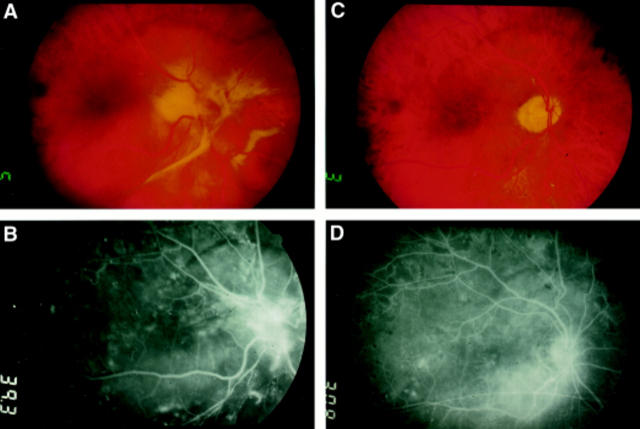
Figure 1 .
Diabetic patient with severe nasal vitreopapillary traction before (A) and after (C) vitrectomy for removal of membranes. In (B) and (D) the corresponding fluorescein angiograms for fundus photos (A) and (C) are shown, respectively. In the preoperative state vitreopapillary traction is accompanied by leakage from the papillary region. The leakage resolved once traction is alleviated by membrane removal as shown in (D).
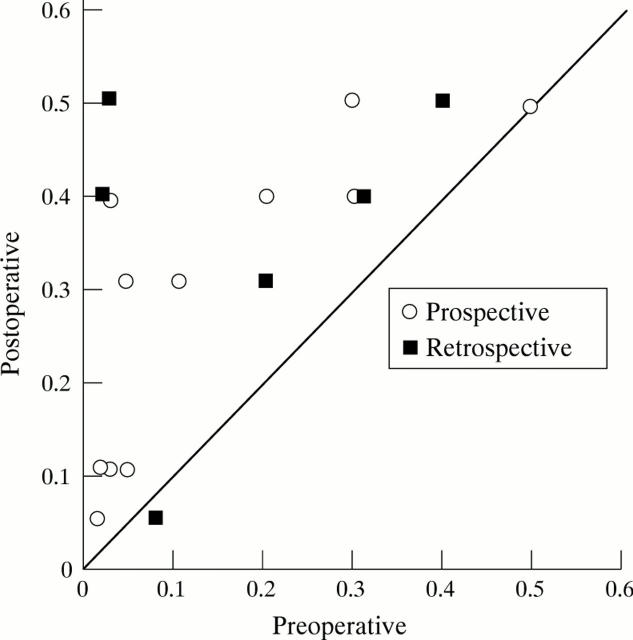
Figure 2 .
Scattergram of visual acuity in eyes with diabetic vitreopapillary traction before and 2 months after vitreoretinal surgery: in 15 of 17 eyes visual acuity improved postoperatively.
Figure 3 .
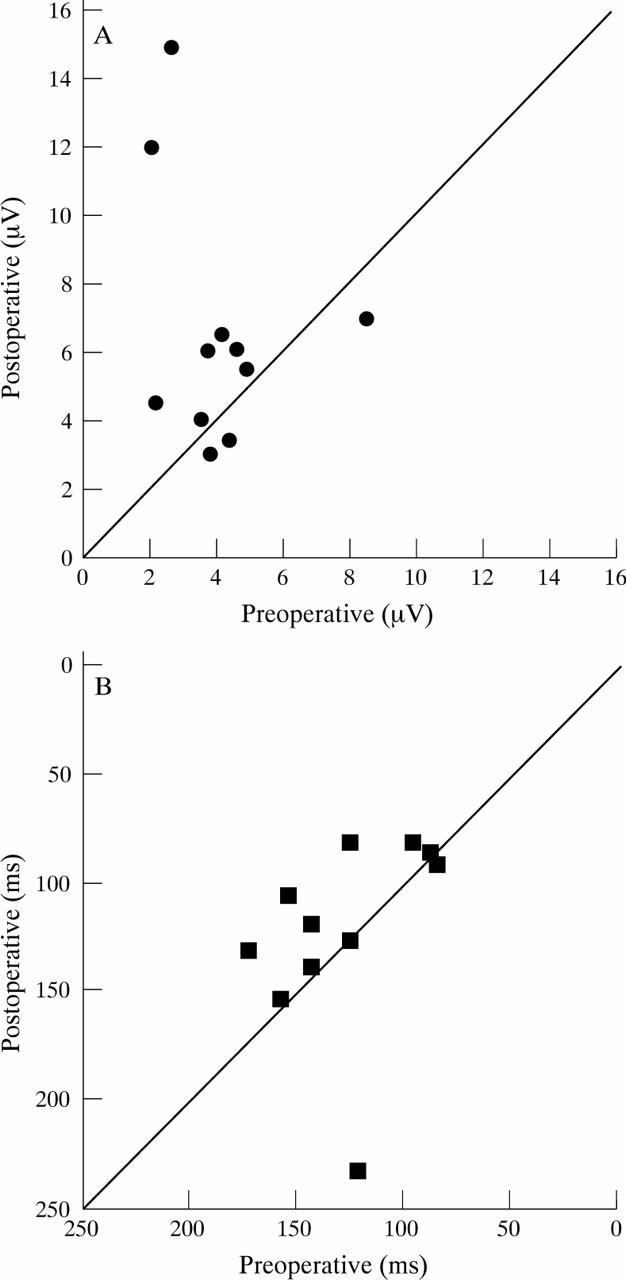
Visual evoked potentials (VEP) in diabetic vitreopapillary traction. VEP amplitudes (A) and VEP latency (B) before and 2 months after vitreoretinal surgery: in eight of 11 patients amplitudes improved after vitrectomy; in 10 of 11 patients a postoperative reduction of latency was observed.
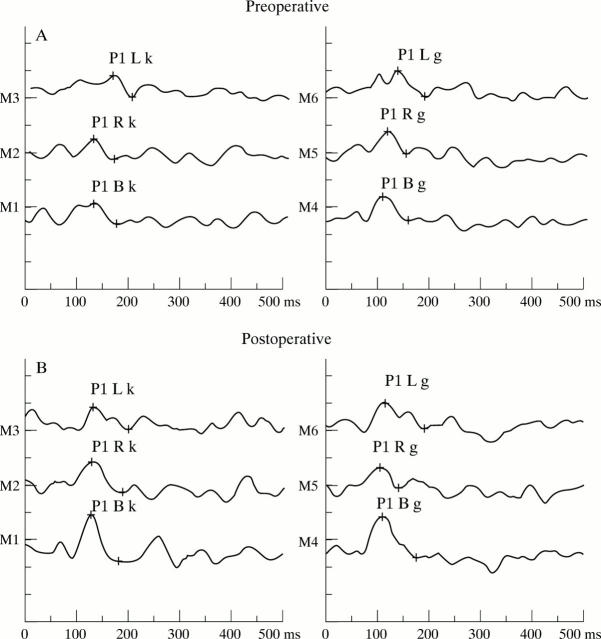
Figure 4 .
Pattern visual evoked potentials (PVEP) in a 50 year old patient with diabetic vitreopapillary traction in the left eye before (A) and 1 week after (B) vitrectomy. (R = right eye, L = left eye, k = small pattern, g = large pattern). An increase in amplitude is seen in tracings M1, M3, and M4.
Figure 5 .
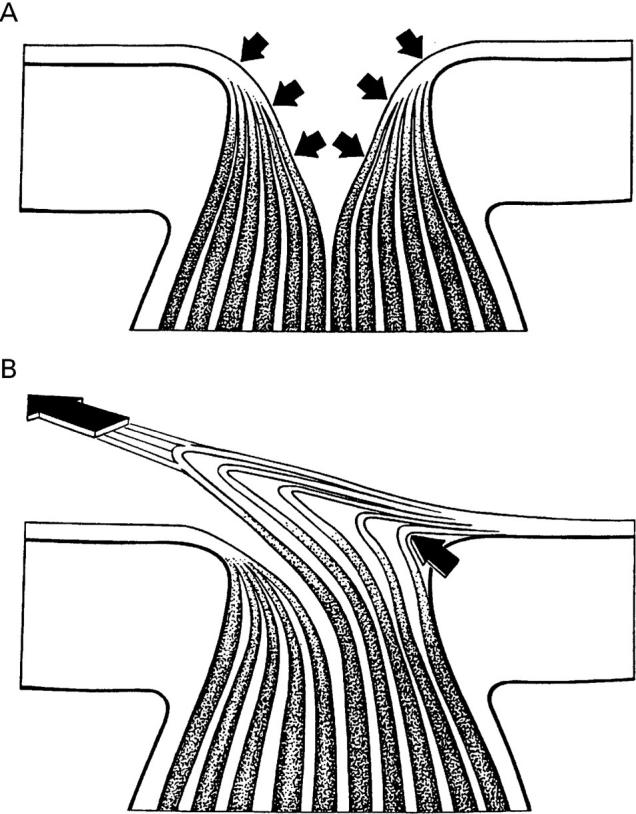
Schematic diagram of changes in the optic nerve head secondary to vitreopapillary traction (A) and in glaucoma (B). (A) Tractional forces of the vitreous on the nerve fibres to the nasal side are responsible for elongation and thinning of these nerve fibres and their vessels, leading to a reduction of axoplasmatic flow and blood flow. This causes visual dysfunction and optic nerve head changes. (B) Typical optic nerve head damage caused by elevated intraocular pressure. Damage arises at the edges of the optic nerve head, leading to thinning of nerve fibres and vessels followed by a reduction of perfusion.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bergin D. J. Nasal heterotopia of the macula with persistent hyaloid vessel. J Pediatr Ophthalmol Strabismus. 1978 Nov-Dec;15(6):373–375. doi: 10.3928/0191-3913-19781101-10. [DOI] [PubMed] [Google Scholar]
- Bottoni F. G., Eggink C. A., Cruysberg J. R., Verbeek A. M. Dominant inherited tilted disc syndrome and lacquer cracks. Eye (Lond) 1990;4(Pt 3):504–509. doi: 10.1038/eye.1990.66. [DOI] [PubMed] [Google Scholar]
- Faulborn J., Bowald S. Microproliferations in proliferative diabetic retinopathy and their relationship to the vitreous: corresponding light and electron microscopic studies. Graefes Arch Clin Exp Ophthalmol. 1985;223(3):130–138. doi: 10.1007/BF02148888. [DOI] [PubMed] [Google Scholar]
- Kroll P., Meyer-Rüsenberg H. W., Busse H. Vorschlag zur Stadieneinteilung der proliferativen diabetischen Retinopathie. Fortschr Ophthalmol. 1987;84(4):360–363. [PubMed] [Google Scholar]
- Maguire A. M., Green W. R., Michels R. G., Erozan Y. S. Recovery of intraocular Toxocara canis by pars plana vitrectomy. Ophthalmology. 1990 May;97(5):675–680. doi: 10.1016/s0161-6420(90)32528-9. [DOI] [PubMed] [Google Scholar]
- Pendergast S. D., Martin D. F., Proia A. D., Jaffe G. J., McCuen B. W., 2nd Removal of optic disc stalks during diabetic vitrectomy. Retina. 1995;15(1):25–28. doi: 10.1097/00006982-199515010-00005. [DOI] [PubMed] [Google Scholar]
- Sawada A., Kitazawa Y., Yamamoto T., Okabe I., Ichien K. Prevention of visual field defect progression with brovincamine in eyes with normal-tension glaucoma. Ophthalmology. 1996 Feb;103(2):283–288. doi: 10.1016/s0161-6420(96)30703-3. [DOI] [PubMed] [Google Scholar]
- Sebag J. Anatomy and pathology of the vitreo-retinal interface. Eye (Lond) 1992;6(Pt 6):541–552. doi: 10.1038/eye.1992.119. [DOI] [PubMed] [Google Scholar]
- Sebag J., Buckingham B., Charles M. A., Reiser K. Biochemical abnormalities in vitreous of humans with proliferative diabetic retinopathy. Arch Ophthalmol. 1992 Oct;110(10):1472–1476. doi: 10.1001/archopht.1992.01080220134035. [DOI] [PubMed] [Google Scholar]
- Sebag J. Diabetic vitreopathy. Ophthalmology. 1996 Feb;103(2):205–206. doi: 10.1016/s0161-6420(96)30716-1. [DOI] [PubMed] [Google Scholar]
- Slavin M. L. Chronic asymptomatic ischemic optic neuropathy. A report of two cases in adults with diabetes mellitus. J Clin Neuroophthalmol. 1987 Dec;7(4):198–201. [PubMed] [Google Scholar]
- Stransky T. J. Diabetic papillopathy and proliferative retinopathy. Graefes Arch Clin Exp Ophthalmol. 1986;224(1):46–50. doi: 10.1007/BF02144133. [DOI] [PubMed] [Google Scholar]
- de Bustros S., Thompson J. T., Michels R. G., Rice T. A. Vitrectomy for progressive proliferative diabetic retinopathy. Arch Ophthalmol. 1987 Feb;105(2):196–199. doi: 10.1001/archopht.1987.01060020050026. [DOI] [PubMed] [Google Scholar]