Abstract
AIM—To report the outcome of a series of patients with stem cell deficiency who underwent allo-limbal transplantation and to describe a technique for this procedure. METHODS—Six consecutive patients underwent allo-limbal stem cell transplantation. The primary diagnosis included alkali burn (n=2), trachoma (n=1), chronic rosacea blepharitis and keratoconjunctivitis (n=1), aniridia (n=1), and Stevens-Johnson syndrome (n=1). The limbal rim consisted of peripheral cornea and perilimbal sclera. FK-506 was used postoperatively for immunosuppression. RESULTS—The length of follow up ranged from 3 to 24 months (mean follow up 11.8 (SD 9.3) months). The outcome was considered satisfactory in five of six cases. The corneal surface was completely epithelialised within 2 weeks, and there was a substantial improvement in vision and symptoms. One patient had recurrent epithelial defects related to eyelid abnormalities. No side effects associated with systemic immunosuppression were noted. CONCLUSION—Allo-limbal transplantation, with systemic immunosuppression with FK-506 is useful in reconstruction of the ocular surface with improvement in vision in patients with severe stem cell deficiency. Keywords: limbal stem cell deficiency; limbal transplantation; cornea
Full Text
The Full Text of this article is available as a PDF (216.2 KB).
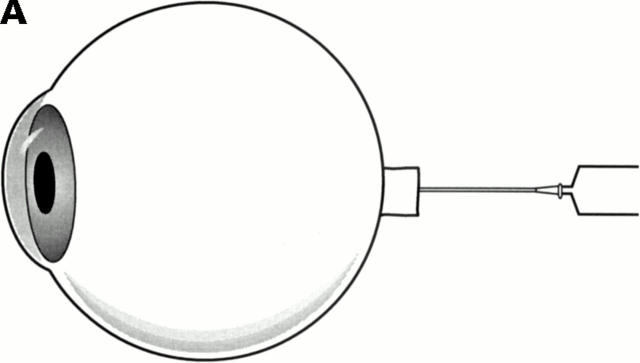
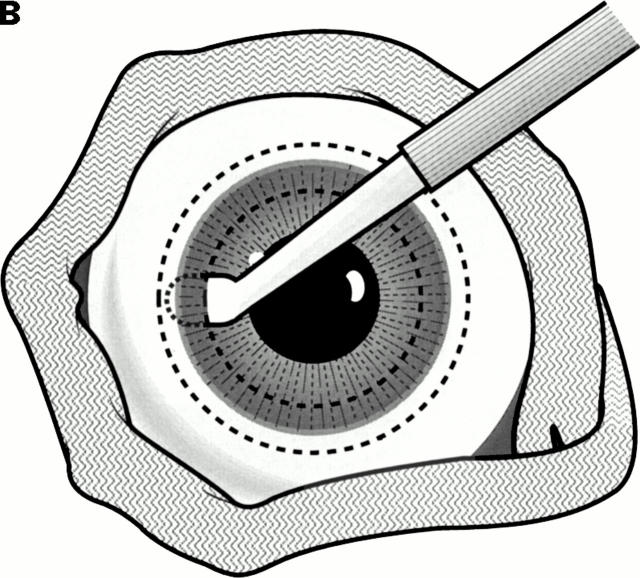
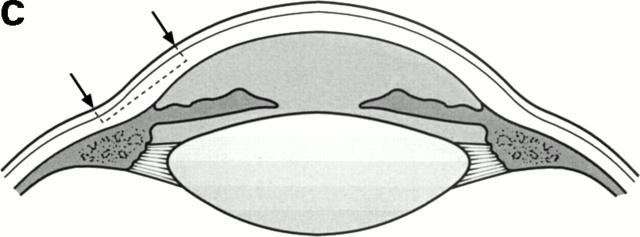
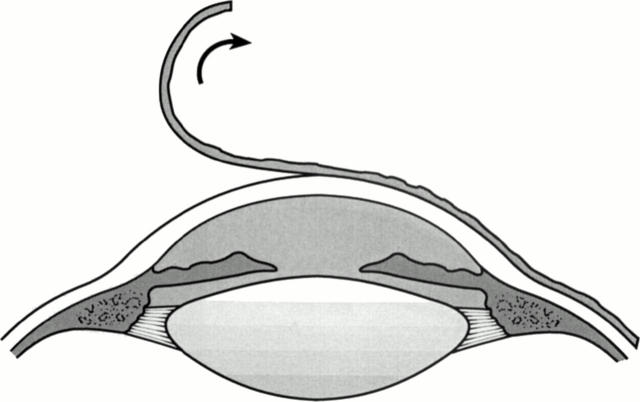
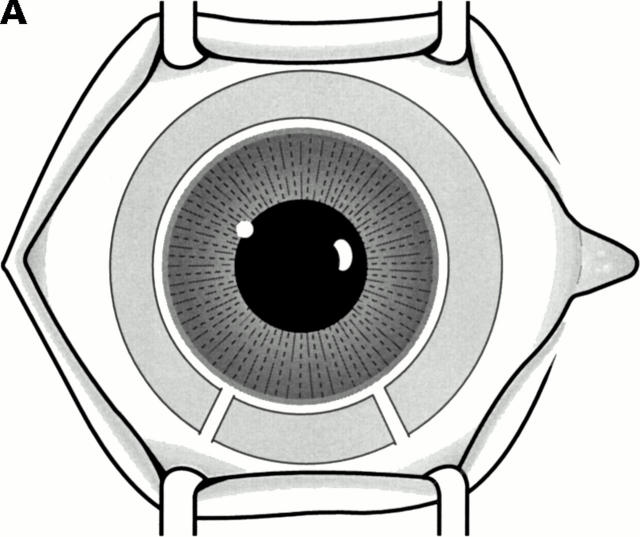
Figure 1 .
Surgical technique. Harvesting donor limbus. (A) Inflating eyeball with sterile air injected through the optic nerve. This route allows air to remain trapped in the vitreous cavity and keeps the eye firm during tissue dissection. (B) Lamellar dissection of a ring of peripheral cornea, limbus, and adjacent sclera with an angled bevel up blade. The donor eyeball is wrapped with a strip of gauze to facilitate handling. (C) The diagram illustrates the location of tissue dissected.
Figure 2 .
Surgical technique. Preparing the host bed. After a 360° peritomy, a plane of dissection superficial to corneal stroma is created and the entire fibrovascular membrane is lifted off the surface.
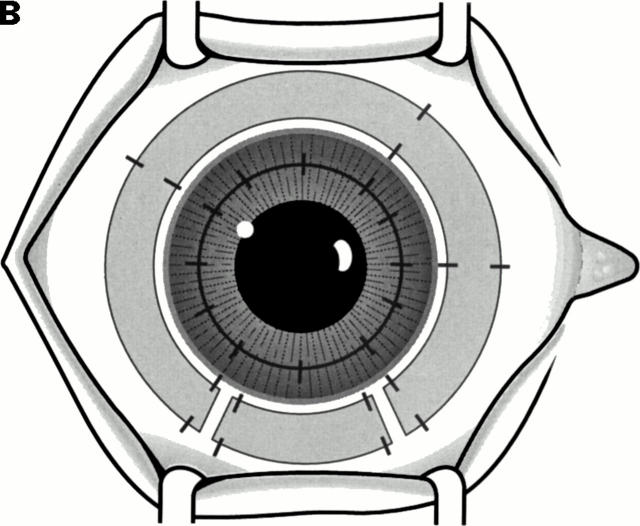
Figure 3 .
Surgical technique. Transplanting the donor limbal ring. (A) The harvested ring of tissue carrying the "stem cells" is placed around the recipient limbus. A small arc of similar tissue, to fill the gap between the cut ends of the limbal ring, is cut to size and appropriately placed. (B) The limbal explants are sutured along both inner and outer circumferences using 10-0 nylon sutures. The sutures are placed directly opposite to each other. In this illustration a central penetrating keratoplasty is also shown.
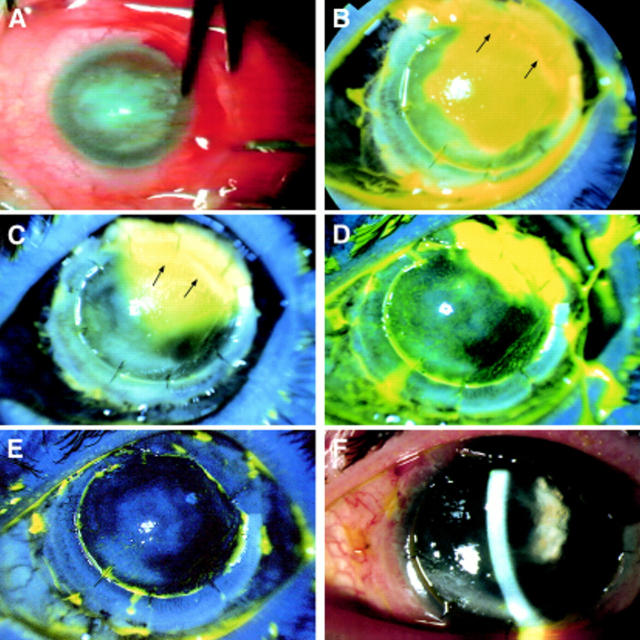
Figure 4 .
Results of limbal transplant in case 2 (primary diagnosis: aniridia). (A) The external appearance of the right eye showing an extensive fibrovascular membrane covering the cornea. The picture was taken during surgery while a peritomy was being done. (B) Slit lamp photograph (fluorescein stained) of the same eye 3 days after surgery. Corneal epithelial cells have started to migrate from the transplanted limbus and are migrating across the host cornea. The quadrant indicated with arrows, where no epithelial cell migration is seen, corresponds to the site where a spacer, fashioned from corneal collagen (without epithelial cover), was placed. (C) Slit lamp photograph (fluorescein stained) of the same eye, 5 days after surgery. Three quarters of the host surface is re-epithelialised. The quadrant corresponding to the spacer (arrows) has remained bare. (D) Slit lamp photograph (fluorescein stained) of the same eye, 7 days after surgery. The remaining quadrant is almost covered by cells migrating from the other quadrants. (E) Slit lamp photograph (fluorescein stained) of the same eye taken on day 8 post surgery. Re-epithelialisation of the host corneal surface from donor limbus is complete. (F) Slit lamp photograph of the same eye 6 weeks after surgery. The cornea is clear and the surface is smooth as illustrated by the broad slit beam. Remnants of the lens capsule (following needling for congenital cataract) with a central opening are now clearly visible.
Figure 5 .
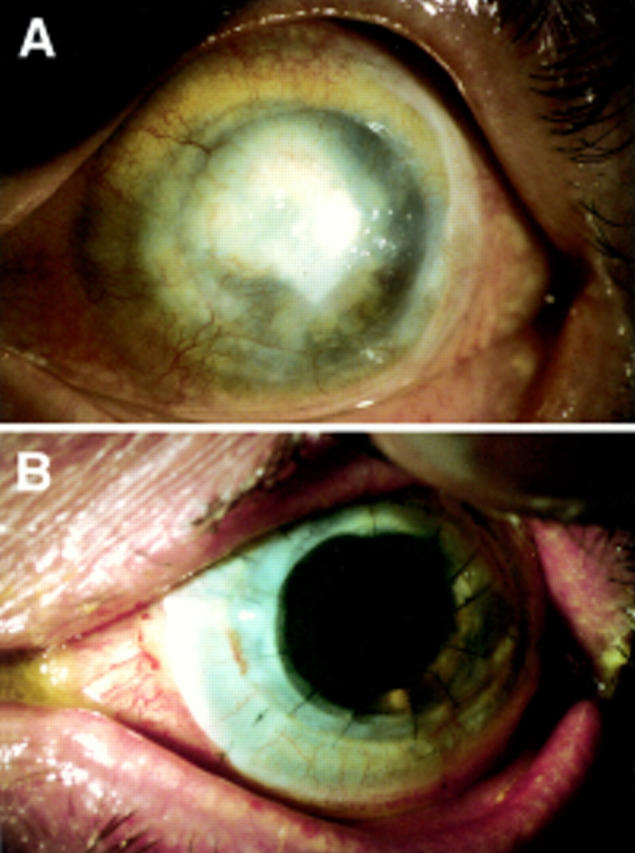
Results of combined limbal and corneal transplant with lens extraction and implant (quadruple procedure) in case 3. (A) Preoperative picture of the left eye of a patient with clinical diagnosis of trachoma of 30 years' duration. The cornea is scarred and vascularised with calcium deposition. The outline of a previously failed corneal graft is visible. Preoperative vision was hand movements. (B) The same eye 8 weeks after surgery. The patient has a follow up of 9 months and maintains a vision of 6/12 unaided and 6/9 with a pinhole.
Figure 6 .
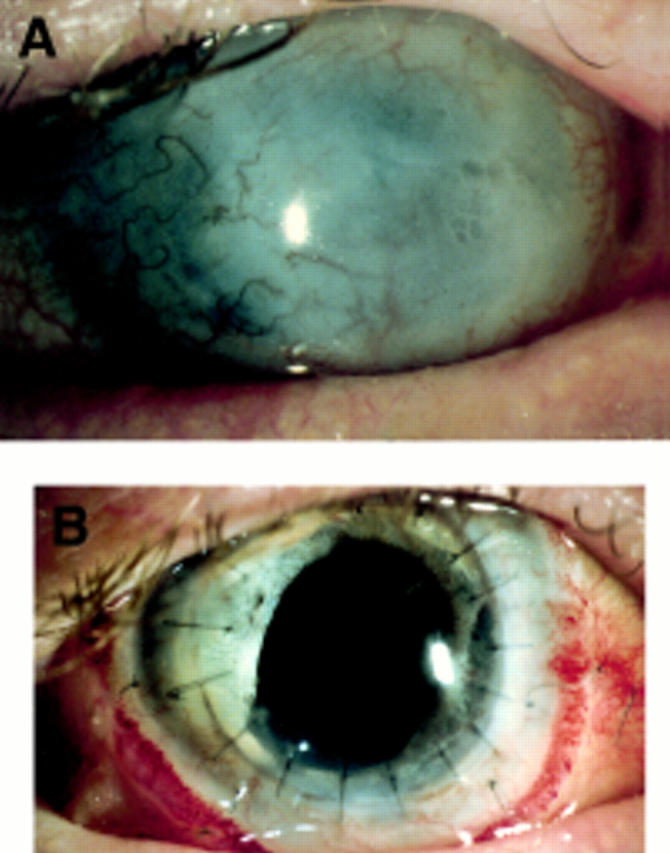
Results of combined limbal and corneal transplant with lens extraction and implant (quadruple procedure) in case 6. (A) Preoperative picture of the right eye of a patient with clinical diagnosis of Stevens-Johnson syndrome. The cornea is scarred and vascularised. Preoperative vision was light perception. (B) The same eye 4 weeks after surgery.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brown S. I., Bloomfield S. E., Pearce D. B. A follow-up report on transplantation of the alkali-burned cornea. Am J Ophthalmol. 1974 Apr;77(4):538–542. doi: 10.1016/0002-9394(74)90468-1. [DOI] [PubMed] [Google Scholar]
- Chen J. J., Tseng S. C. Corneal epithelial wound healing in partial limbal deficiency. Invest Ophthalmol Vis Sci. 1990 Jul;31(7):1301–1314. [PubMed] [Google Scholar]
- Clinch T. E., Goins K. M., Cobo L. M. Treatment of contact lens-related ocular surface disorders with autologous conjunctival transplantation. Ophthalmology. 1992 Apr;99(4):634–638. doi: 10.1016/s0161-6420(92)31925-6. [DOI] [PubMed] [Google Scholar]
- Copeland R. A., Jr, Char D. H. Limbal autograft reconstruction after conjunctival squamous cell carcinoma. Am J Ophthalmol. 1990 Oct 15;110(4):412–415. doi: 10.1016/s0002-9394(14)77023-0. [DOI] [PubMed] [Google Scholar]
- Holland E. J. Epithelial transplantation for the management of severe ocular surface disease. Trans Am Ophthalmol Soc. 1996;94:677–743. [PMC free article] [PubMed] [Google Scholar]
- Holland E. J., Schwartz G. S. The evolution of epithelial transplantation for severe ocular surface disease and a proposed classification system. Cornea. 1996 Nov;15(6):549–556. [PubMed] [Google Scholar]
- Huang A. J., Tseng S. C. Corneal epithelial wound healing in the absence of limbal epithelium. Invest Ophthalmol Vis Sci. 1991 Jan;32(1):96–105. [PubMed] [Google Scholar]
- Ishioka M., Ohno S., Nakamura S., Isobe K., Watanabe N., Ishigatsubo Y., Tanaka S. FK506 treatment of noninfectious uveitis. Am J Ophthalmol. 1994 Dec 15;118(6):723–729. doi: 10.1016/s0002-9394(14)72551-6. [DOI] [PubMed] [Google Scholar]
- Jenkins C., Tuft S., Liu C., Buckley R. Limbal transplantation in the management of chronic contact-lens-associated epitheliopathy. Eye (Lond) 1993;7(Pt 5):629–633. doi: 10.1038/eye.1993.145. [DOI] [PubMed] [Google Scholar]
- Kenyon K. R., Tseng S. C. Limbal autograft transplantation for ocular surface disorders. Ophthalmology. 1989 May;96(5):709–723. doi: 10.1016/s0161-6420(89)32833-8. [DOI] [PubMed] [Google Scholar]
- Kino T., Hatanaka H., Hashimoto M., Nishiyama M., Goto T., Okuhara M., Kohsaka M., Aoki H., Imanaka H. FK-506, a novel immunosuppressant isolated from a Streptomyces. I. Fermentation, isolation, and physico-chemical and biological characteristics. J Antibiot (Tokyo) 1987 Sep;40(9):1249–1255. doi: 10.7164/antibiotics.40.1249. [DOI] [PubMed] [Google Scholar]
- Kinoshita S., Kiorpes T. C., Friend J., Thoft R. A. Limbal epithelium in ocular surface wound healing. Invest Ophthalmol Vis Sci. 1982 Jul;23(1):73–80. [PubMed] [Google Scholar]
- Kruse F. E. Stem cells and corneal epithelial regeneration. Eye (Lond) 1994;8(Pt 2):170–183. doi: 10.1038/eye.1994.42. [DOI] [PubMed] [Google Scholar]
- Kwitko S., Marinho D., Barcaro S., Bocaccio F., Rymer S., Fernandes S., Neumann J. Allograft conjunctival transplantation for bilateral ocular surface disorders. Ophthalmology. 1995 Jul;102(7):1020–1025. doi: 10.1016/s0161-6420(95)30918-9. [DOI] [PubMed] [Google Scholar]
- Mochizuki M., Masuda K., Sakane T., Ito K., Kogure M., Sugino N., Usui M., Mizushima Y., Ohno S., Inaba G. A clinical trial of FK506 in refractory uveitis. Am J Ophthalmol. 1993 Jun 15;115(6):763–769. doi: 10.1016/s0002-9394(14)73645-1. [DOI] [PubMed] [Google Scholar]
- Nishida K., Kinoshita S., Ohashi Y., Kuwayama Y., Yamamoto S. Ocular surface abnormalities in aniridia. Am J Ophthalmol. 1995 Sep;120(3):368–375. doi: 10.1016/s0002-9394(14)72167-1. [DOI] [PubMed] [Google Scholar]
- Pels E., van der Gaag R. HLA-A,B,C, and HLA-DR antigens and dendritic cells in fresh and organ culture preserved corneas. Cornea. 1984 1985;3(4):231–239. [PubMed] [Google Scholar]
- Pfister R. R. Corneal stem cell disease: concepts, categorization, and treatment by auto- and homotransplantation of limbal stem cells. CLAO J. 1994 Jan;20(1):64–72. [PubMed] [Google Scholar]
- Puangsricharern V., Tseng S. C. Cytologic evidence of corneal diseases with limbal stem cell deficiency. Ophthalmology. 1995 Oct;102(10):1476–1485. doi: 10.1016/s0161-6420(95)30842-1. [DOI] [PubMed] [Google Scholar]
- Rubsamen P. E., Irvin W. D., McCuen B. W., 2nd, Smiddy W. E., Bowman C. B. Primary intraocular lens implantation in the setting of penetrating ocular trauma. Ophthalmology. 1995 Jan;102(1):101–107. doi: 10.1016/s0161-6420(95)31073-1. [DOI] [PubMed] [Google Scholar]
- Schermer A., Galvin S., Sun T. T. Differentiation-related expression of a major 64K corneal keratin in vivo and in culture suggests limbal location of corneal epithelial stem cells. J Cell Biol. 1986 Jul;103(1):49–62. doi: 10.1083/jcb.103.1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starzl T. E., Todo S., Fung J., Demetris A. J., Venkataramman R., Jain A. FK 506 for liver, kidney, and pancreas transplantation. Lancet. 1989 Oct 28;2(8670):1000–1004. doi: 10.1016/s0140-6736(89)91014-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundmacher R., Reinhard T. Central corneolimbal transplantation under systemic ciclosporin A cover for severe limbal stem cell insufficiency. Graefes Arch Clin Exp Ophthalmol. 1996 Aug;234 (Suppl 1):S122–S125. doi: 10.1007/BF02343060. [DOI] [PubMed] [Google Scholar]
- Tan D. T., Ficker L. A., Buckley R. J. Limbal transplantation. Ophthalmology. 1996 Jan;103(1):29–36. doi: 10.1016/s0161-6420(96)30737-9. [DOI] [PubMed] [Google Scholar]
- Thoft R. A. Keratoepithelioplasty. Am J Ophthalmol. 1984 Jan;97(1):1–6. doi: 10.1016/0002-9394(84)90438-0. [DOI] [PubMed] [Google Scholar]
- Tocci M. J., Matkovich D. A., Collier K. A., Kwok P., Dumont F., Lin S., Degudicibus S., Siekierka J. J., Chin J., Hutchinson N. I. The immunosuppressant FK506 selectively inhibits expression of early T cell activation genes. J Immunol. 1989 Jul 15;143(2):718–726. [PubMed] [Google Scholar]
- Tsai R. J., Tseng S. C. Human allograft limbal transplantation for corneal surface reconstruction. Cornea. 1994 Sep;13(5):389–400. doi: 10.1097/00003226-199409000-00003. [DOI] [PubMed] [Google Scholar]
- Tseng S. C., Prabhasawat P., Barton K., Gray T., Meller D. Amniotic membrane transplantation with or without limbal allografts for corneal surface reconstruction in patients with limbal stem cell deficiency. Arch Ophthalmol. 1998 Apr;116(4):431–441. doi: 10.1001/archopht.116.4.431. [DOI] [PubMed] [Google Scholar]
- Tsubota K., Toda I., Saito H., Shinozaki N., Shimazaki J. Reconstruction of the corneal epithelium by limbal allograft transplantation for severe ocular surface disorders. Ophthalmology. 1995 Oct;102(10):1486–1496. doi: 10.1016/s0161-6420(95)30841-x. [DOI] [PubMed] [Google Scholar]
- Turgeon P. W., Nauheim R. C., Roat M. I., Stopak S. S., Thoft R. A. Indications for keratoepithelioplasty. Arch Ophthalmol. 1990 Feb;108(2):233–236. doi: 10.1001/archopht.1990.01070040085036. [DOI] [PubMed] [Google Scholar]