Abstract
AIM—To evaluate the optical coherence tomographic characteristics of choroidal neovascularisation (CNV) in age related macular degeneration (AMD) and in idiopathic and inflammatory CNV. The use of this technique in the selection of patients for surgery is discussed. METHODS—Ocular coherence tomography (OCT), fluorescein, and indocyanine green angiography were performed in 23 patients affected by AMD complicated by well defined CNV and in 10 patients affected by inflammatory or idiopathic CNV. The neovascular membrane was surgically removed in five age related CNVs, two inflammatory choroidopathies, and two idiopathic CNVs. RESULTS—In inflammatory and idiopathic CNV, the OCT displayed a neovascularisation on the retinal pigment epithelium (RPE). In three cases the CNV was excised with an improvement of visual acuity equal to or greater than two Snellen lines; in a fourth case, the visual acuity after surgery was unchanged. In the cases of AMD the OCT fell into three different patterns: (A) CNV above the RPE (five cases); (B) focal, irregular thickening of the retinal pigment epithelial band (12 cases); (C) CNV above and below the RPE (six cases). The five pattern A CNV patients underwent the surgical excision of the neovascularisation. In four cases the visual acuity improved by two or more Snellen lines; in the fifth case the visual acuity remained unchanged. CONCLUSIONS—The authors suggest that the surgical removal of early age related CNV could be performed in those cases where the OCT shows a neovascular membrane on the RPE, as in idiopathic and inflammatory CNVs. Keywords: age related macular degeneration; choroidal neovascularisation; optical coherence tomography; vitreoretinal surgery
Full Text
The Full Text of this article is available as a PDF (199.0 KB).
Figure 1 .
(A) Fluorescein angiogram shows an idiopathic subfoveal CNV in a 34 year old woman. (The broken line on FA frame indicates the OCT scan direction). (B) The OCT shows a marked thickening (481 µm) of the neurosensory retina corresponding to the CNV. The CNV can be identified as an area of hyperreflectivity lying above the band corresponding to the RPE.
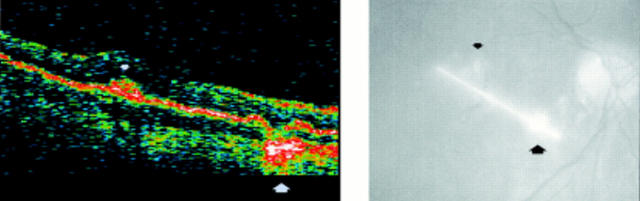
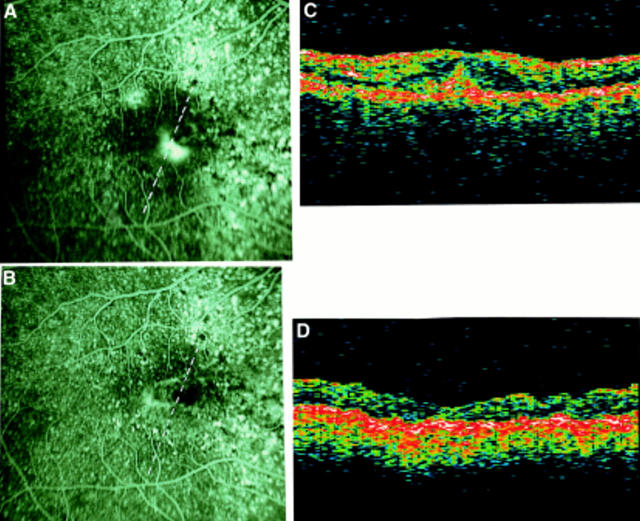
Figure 2 .
Multifocal choroidopathy. The OCT displays a focal hyperreflectivity lying above the RPE corresponding to the CNV (small arrows); at the same site of the atrophic spot a deep hyperreflectivity can be detected (large arrows).
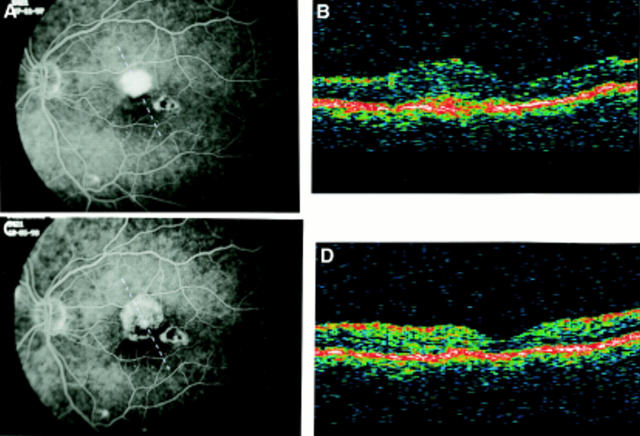
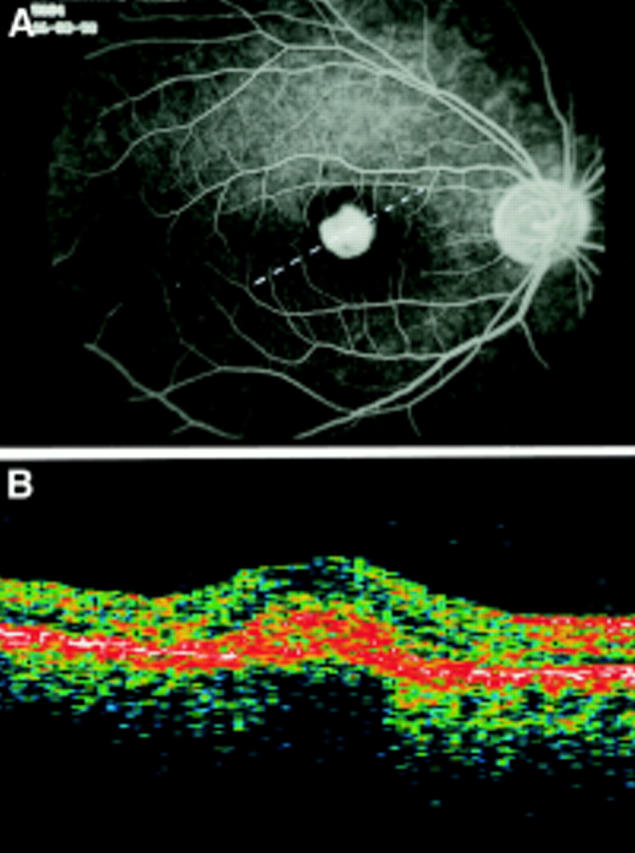
Figure 3 .
Multifocal choroidopathy. (A) Fluorescein angiography before surgery (VA= 20/40). (The broken line on FA frame indicates the OCT scan direction). (B) OCT before surgery: the neurosensory thickness is 475 µm; a focal hyperreflectivity lying above the band corresponding to the RPE can be visualised. (C) Fluorescein angiography after surgery (VA= 20/30): the CNV has been completely removed. (The broken line on FA frame indicates the OCT scan direction). (D) OCT after surgery: the normal foveal profile is restored and retinal thickness is 160 µm. The hyperreflectivity interpreted as the CNV is no longer visible.
Figure 4 .
AMD complicated by CNV (OCT pattern A). (A) Fluorescein angiography shows a juxtafoveal and a peripapillary CNV. (The broken line on FA frame indicates the OCT scan direction). (B) The OCT scan performed through the juxtafoveal CNV reveals a marked thickening (503 µm) of the neurosensory retina and an increased reflectivity above the RPE interpreted as the CNV. A thin optically empty space, signifying neurosensory detachment, surrounds the CNV.
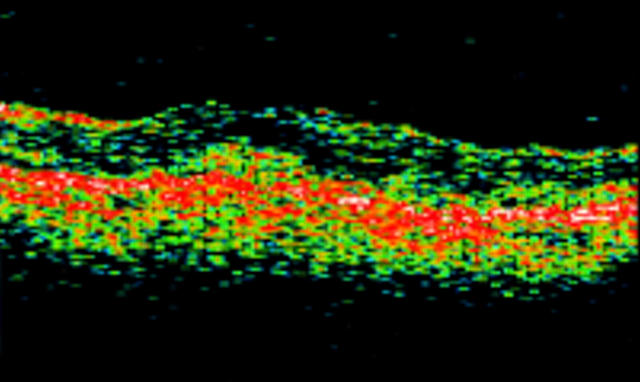
Figure 5 .
AMD complicated by CNV (OCT pattern B). The OCT shows a focal, irregular thickening of the band corresponding to the RPE, that appears fragmented and disorganised.
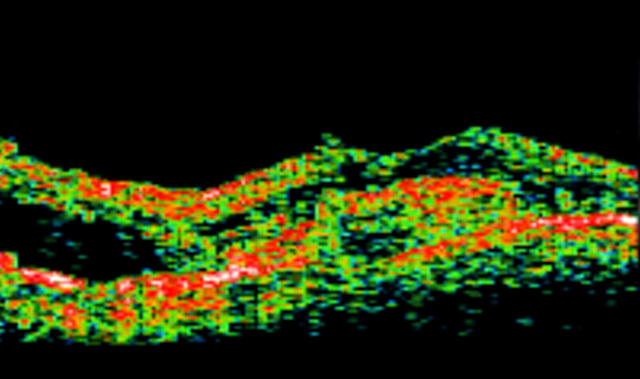
Figure 6 .
AMD complicated by CNV (OCT pattern C). An irregular hyperreflectivity can be visualised both above and below the level of the band corresponding to the RPE. The retinal pigment epithelial band presents a focal duplication.
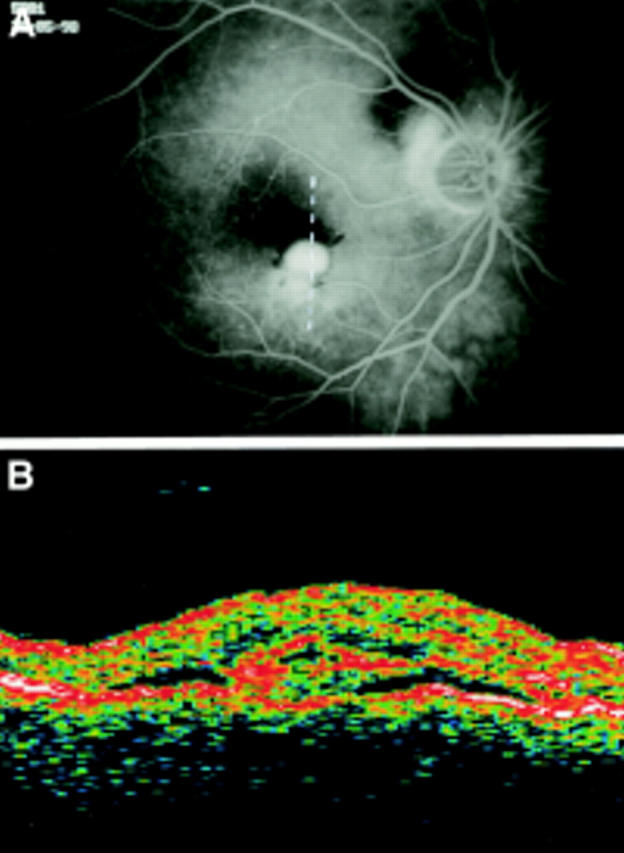
Figure 7 .
AMD complicated by subfoveal CNV. (A) Fluorescein angiography before surgery (VA=20/200). (The broken line on FA frame indicates the OCT scan direction). (B) The OCT clearly displays a focal hyperreflectivity lying above the RPE interpreted as the CNV. In this case the OCT shows the relation between CNV and the centre of the fovea. The adjacent neuroretina presents a non-homogeneous, reduced, hyperreflectivity due to oedema. The retinal thickness is 379 µm. (C) Fluorescein angiography after surgery (VA= 20/60). The loss of retinal pigment epithelial cells and choriocapillaris is minimal. (The broken line on FA frame indicates the OCT scan direction). (D) The focal hyperreflectivity identified by OCT before surgery is no longer visible. The retinal thickness is 154 µm.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berger A. S., Conway M., Del Priore L. V., Walker R. S., Pollack J. S., Kaplan H. J. Submacular surgery for subfoveal choroidal neovascular membranes in patients with presumed ocular histoplasmosis. Arch Ophthalmol. 1997 Aug;115(8):991–996. doi: 10.1001/archopht.1997.01100160161004. [DOI] [PubMed] [Google Scholar]
- Berger A. S., Kaplan H. J. Clinical experience with the surgical removal of subfoveal neovascular membranes. Short-term postoperative results. Ophthalmology. 1992 Jun;99(6):969–976. doi: 10.1016/s0161-6420(92)31869-x. [DOI] [PubMed] [Google Scholar]
- Gass J. D. Biomicroscopic and histopathologic considerations regarding the feasibility of surgical excision of subfoveal neovascular membranes. Am J Ophthalmol. 1994 Sep 15;118(3):285–298. [PubMed] [Google Scholar]
- Grossniklaus H. E., Hutchinson A. K., Capone A., Jr, Woolfson J., Lambert H. M. Clinicopathologic features of surgically excised choroidal neovascular membranes. Ophthalmology. 1994 Jun;101(6):1099–1111. doi: 10.1016/s0161-6420(13)31216-0. [DOI] [PubMed] [Google Scholar]
- Grossniklaus H. E., Hutchinson A. K., Capone A., Jr, Woolfson J., Lambert H. M. Clinicopathologic features of surgically excised choroidal neovascular membranes. Ophthalmology. 1994 Jun;101(6):1099–1111. doi: 10.1016/s0161-6420(13)31216-0. [DOI] [PubMed] [Google Scholar]
- Hee M. R., Baumal C. R., Puliafito C. A., Duker J. S., Reichel E., Wilkins J. R., Coker J. G., Schuman J. S., Swanson E. A., Fujimoto J. G. Optical coherence tomography of age-related macular degeneration and choroidal neovascularization. Ophthalmology. 1996 Aug;103(8):1260–1270. doi: 10.1016/s0161-6420(96)30512-5. [DOI] [PubMed] [Google Scholar]
- Hee M. R., Izatt J. A., Swanson E. A., Huang D., Schuman J. S., Lin C. P., Puliafito C. A., Fujimoto J. G. Optical coherence tomography of the human retina. Arch Ophthalmol. 1995 Mar;113(3):325–332. doi: 10.1001/archopht.1995.01100030081025. [DOI] [PubMed] [Google Scholar]
- Huang D., Swanson E. A., Lin C. P., Schuman J. S., Stinson W. G., Chang W., Hee M. R., Flotte T., Gregory K., Puliafito C. A. Optical coherence tomography. Science. 1991 Nov 22;254(5035):1178–1181. doi: 10.1126/science.1957169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang D., Wang J., Lin C. P., Puliafito C. A., Fujimoto J. G. Micron-resolution ranging of cornea anterior chamber by optical reflectometry. Lasers Surg Med. 1991;11(5):419–425. doi: 10.1002/lsm.1900110506. [DOI] [PubMed] [Google Scholar]
- Hudson H. L., Frambach D. A., Lopez P. F. Relation of the functional and structural fundus changes after submacular surgery for neovascular age-related macular degeneration. Br J Ophthalmol. 1995 May;79(5):417–423. doi: 10.1136/bjo.79.5.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert H. M., Capone A., Jr, Aaberg T. M., Sternberg P., Jr, Mandell B. A., Lopez P. F. Surgical excision of subfoveal neovascular membranes in age-related macular degeneration. Am J Ophthalmol. 1992 Mar 15;113(3):257–262. doi: 10.1016/s0002-9394(14)71576-4. [DOI] [PubMed] [Google Scholar]
- Mietz H., Merrill P. T., Lambert H. M., Font R. L. Combined subretinal and sub-retinal pigment epithelium neovascular membranes in age-related macular degeneration: a clinicopathologic study of six cases. Ophthalmic Surg Lasers. 1997 Aug;28(8):645–652. [PubMed] [Google Scholar]
- Nasir M. A., Sugino I., Zarbin M. A. Decreased choriocapillaris perfusion following surgical excision of choroidal neovascular membranes in age-related macular degeneration. Br J Ophthalmol. 1997 Jun;81(6):481–489. doi: 10.1136/bjo.81.6.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ormerod L. D., Puklin J. E., Frank R. N. Long-term outcomes after the surgical removal of advanced subfoveal neovascular membranes in age-related macular degeneration. Ophthalmology. 1994 Jul;101(7):1201–1210. doi: 10.1016/s0161-6420(94)31200-0. [DOI] [PubMed] [Google Scholar]
- Pollack J. S., Del Priore L. V., Smith M. E., Feiner M. A., Kaplan H. J. Postoperative abnormalities of the choriocapillaris in exudative age-related macular degeneration. Br J Ophthalmol. 1996 Apr;80(4):314–318. doi: 10.1136/bjo.80.4.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puliafito C. A., Hee M. R., Lin C. P., Reichel E., Schuman J. S., Duker J. S., Izatt J. A., Swanson E. A., Fujimoto J. G. Imaging of macular diseases with optical coherence tomography. Ophthalmology. 1995 Feb;102(2):217–229. doi: 10.1016/s0161-6420(95)31032-9. [DOI] [PubMed] [Google Scholar]
- Schuman J. S., Hee M. R., Puliafito C. A., Wong C., Pedut-Kloizman T., Lin C. P., Hertzmark E., Izatt J. A., Swanson E. A., Fujimoto J. G. Quantification of nerve fiber layer thickness in normal and glaucomatous eyes using optical coherence tomography. Arch Ophthalmol. 1995 May;113(5):586–596. doi: 10.1001/archopht.1995.01100050054031. [DOI] [PubMed] [Google Scholar]
- Thomas M. A., Dickinson J. D., Melberg N. S., Ibanez H. E., Dhaliwal R. S. Visual results after surgical removal of subfoveal choroidal neovascular membranes. Ophthalmology. 1994 Aug;101(8):1384–1396. doi: 10.1016/s0161-6420(94)31172-9. [DOI] [PubMed] [Google Scholar]
- Thomas M. A., Grand M. G., Williams D. F., Lee C. M., Pesin S. R., Lowe M. A. Surgical management of subfoveal choroidal neovascularization. Ophthalmology. 1992 Jun;99(6):952–976. doi: 10.1016/s0161-6420(92)31888-3. [DOI] [PubMed] [Google Scholar]
- Yannuzzi L. A., Hope-Ross M., Slakter J. S., Guyer D. R., Sorenson J. A., Ho A. C., Sperber D. E., Freund K. B., Orlock D. A. Analysis of vascularized pigment epithelial detachments using indocyanine green videoangiography. Retina. 1994;14(2):99–113. doi: 10.1097/00006982-199414020-00003. [DOI] [PubMed] [Google Scholar]
- Yannuzzi L. A., Slakter J. S., Sorenson J. A., Guyer D. R., Orlock D. A. Digital indocyanine green videoangiography and choroidal neovascularization. Retina. 1992;12(3):191–223. [PubMed] [Google Scholar]