Abstract
AIM—To evaluate the image quality produced by polypseudophakia used for strongly hypermetropic and nanophthalmic eyes. METHODS—Primary aberration theory and ray tracing analysis were used to calculate the optimum lens shapes and power distribution between the two intraocular lenses for two example eyes: one a strongly hypermetropic eye, the other a nanophthalmic eye. Spherical aberration and oblique astigmatism were considered. Modulation transfer function (MTF) curves were computed using commercial optical design software (Sigma 2100, Kidger Optics Ltd) to assess axial image quality, and the sagittal and tangential image surfaces were computed to study image quality across the field. RESULTS—A significant improvement in the axial MTF was found for the eyes with double implants. However, results indicate that this may be realised as a better contrast sensitivity in the low to mid spatial frequency range rather than as a better Snellen acuity. The optimum lens shapes for minimum spherical aberration (best axial image quality) were approximately convex-plano for both lenses with the convex surface facing the cornea. Conversely, the optimum lens shapes for zero oblique astigmatism were strongly meniscus with the anterior surface concave. Correction of oblique astigmatism was only achieved with a loss in axial performance. CONCLUSIONS—Optimum estimated visual acuity exceeds 6/5 in both the hypermetropic and the nanophthalmic eyes studied (pupil size of 4 mm) with polypseudophakic correction. These results can be attained using convex-plano or biconvex lenses with the most convex surface facing the cornea. If the posterior surface of the posterior intraocular lens is convex, as is commonly used to help prevent migration of lens epithelial cells causing posterior capsular opacification (PCO), then it is still possible to achieve 6/4.5 in the hypermetropic eye and 6/5.3 in the nanophthalmic eye provided the anterior intraocular lens has an approximately convex-plano shape with the convex surface anterior. It was therefore concluded that consideration of optical image quality does not demand that additional intraocular lens shapes need to be manufactured for polypseudophakic correction of extremely short eyes and that implanting the posterior intraocular lens in the conventional orientation to help prevent PCO does not necessarily limit estimated visual acuity.
Full Text
The Full Text of this article is available as a PDF (191.1 KB).
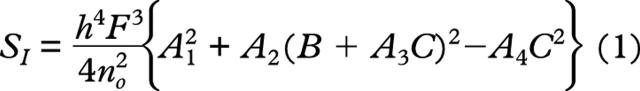
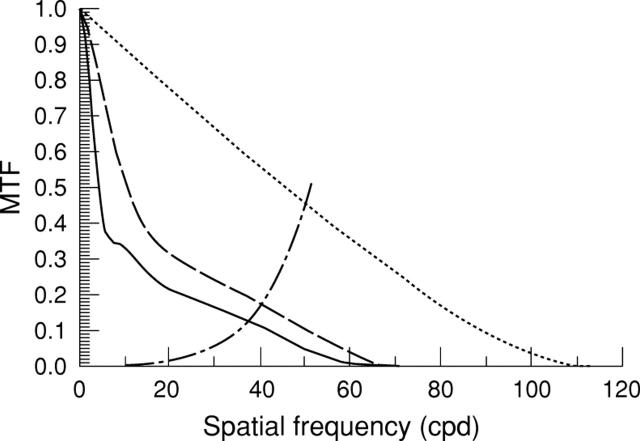
Figure 1 .
Axial modulation transfer function (MTF) curves for both a single (solid line) and double implant lenses (broken line) implanted in the hypermetropic example eye described in the text. The dotted curve represents the diffraction limit for a 4 mm pupil size with Stiles-Crawford correction and for a wavelength of 587.6 nm. The retina-brain contrast threshold (alternate dash-dot curve) has been superposed to allow estimates of visual acuity, which occur where the curves intersect, to be made.
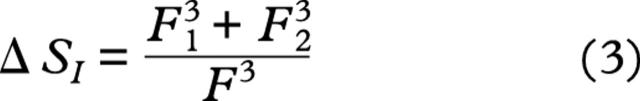
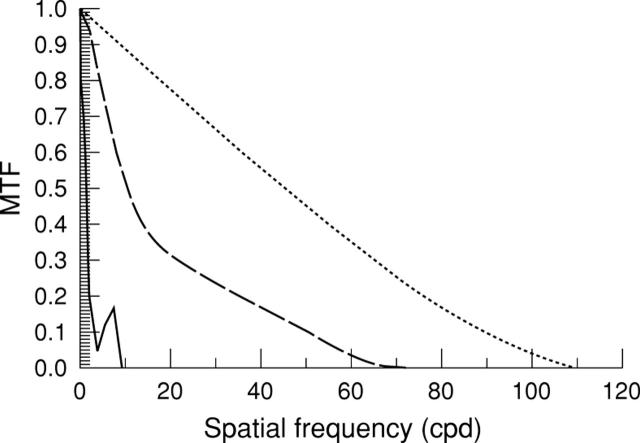
Figure 2 .
Axial modulation transfer function (MTF) curves for both a single (solid line) and double implant lenses (broken line) implanted in the nanophthalmic example eye described in the text. The dotted curve represents the diffraction limit for a 4 mm pupil size with Stiles-Crawford correction and for a wavelength of 587.6 nm. The retina-brain contrast threshold (alternate dash-dot curve) has been superposed to allow estimates of visual acuity, which occur where the curves intersect, to be made.
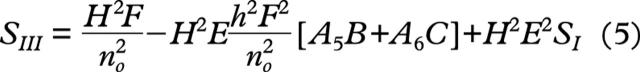
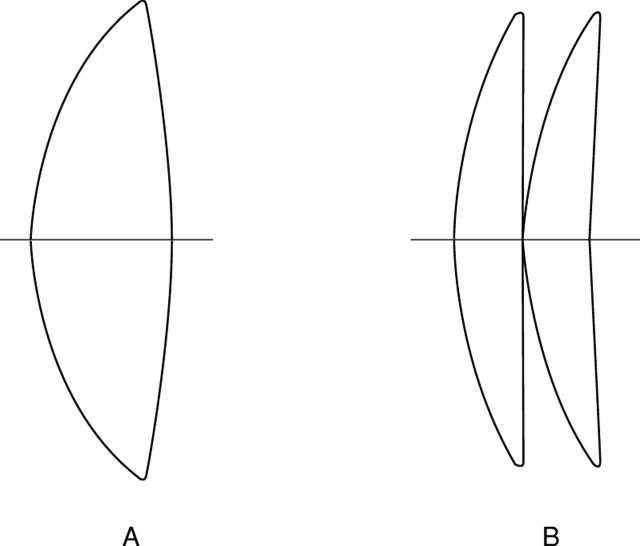
Figure 3 .
Single and double implant intraocular lens shapes to maximise axial image quality (minimise spherical aberration). Note that the lens shapes are the same for both the hypermetropic eye and the nanophthalmic eye described in the text.
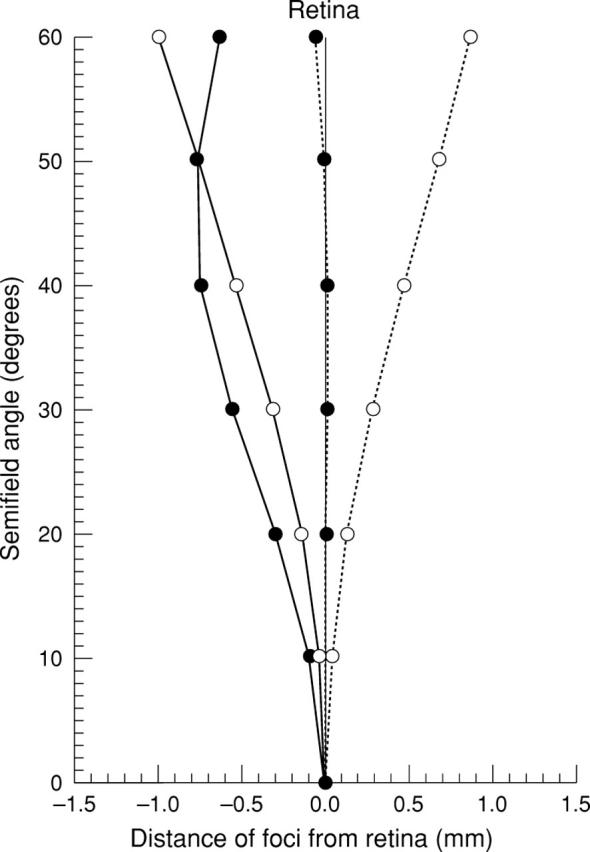
Figure 4 .
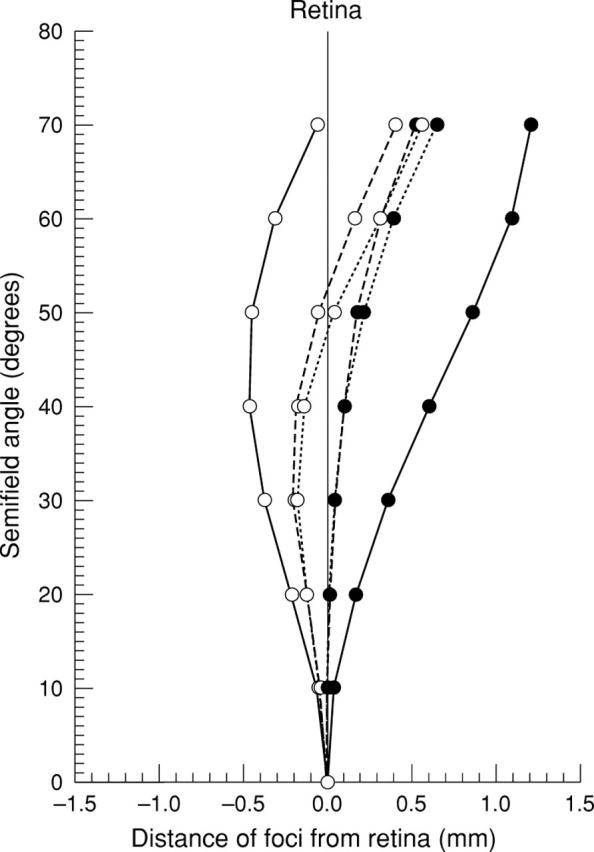
Sagittal (solid circles) and tangential (open circles) image surfaces plotted for the Gullstrand-Le Grand schematic eye (solid curves) and for the hypermetropic example eye corrected with both a single (broken curves) and double implant lenses (dotted curves). The disc of least confusion lies approximately mid way between the sagittal and tangential image surfaces.
Figure 5 .
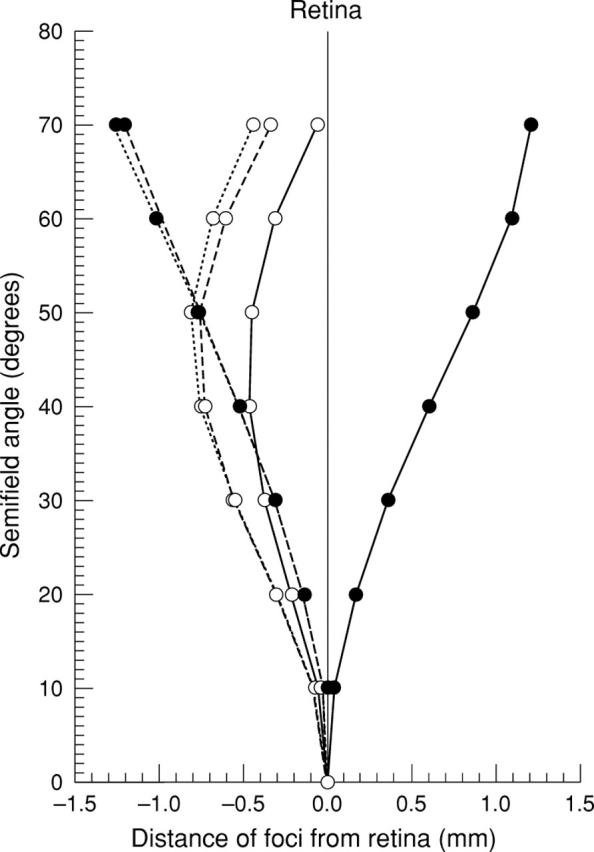
Sagittal (solid circles) and tangential (open circles) image surfaces plotted for the nanophthalmic example eye corrected with both a single (solid curves) and double implant lenses (dotted curves). The disc of least confusion lies approximately mid way between the sagittal and tangential image surfaces.
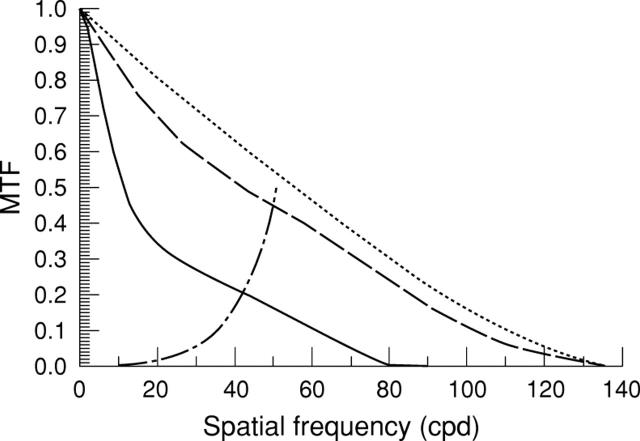
Figure 6 .
Axial modulation transfer function (MTF) curves for double implant lens shapes that reduce oblique astigmatism (solid line) and which maximise axial image quality (broken line) implanted in the nanophthalmic example eye described in the text. The dotted curve represents the diffraction limit for a 4 mm pupil size with Stiles-Crawford correction and for a wavelength of 587.6 nm.
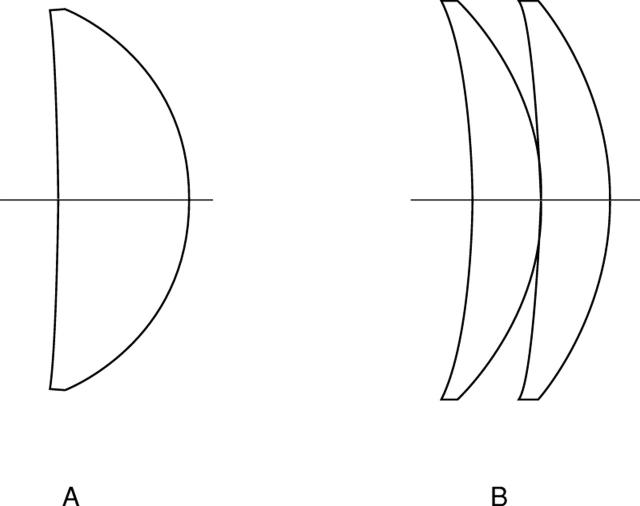
Figure 7 .
Single and double implant intraocular lens shapes that minimise oblique astigmatism. The lens shapes illustrated are for the hypermetropic eye described in the text. The intraocular lens shapes for the nanophthalmic eye are slightly more meniscus (see Table 3).
Figure 8 .
Sagittal (open circles) and tangential image surfaces (solid circles) plotted for the nanophthalmic example eye corrected with thin double implant lenses optimised to give zero oblique astigmatism (solid curves). Thickening the lenses increases the oblique astigmatism and moves the image surfaces behind the retina (broken curves).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Atchison D. A., Collins M. J., Wildsoet C. F., Christensen J., Waterworth M. D. Measurement of monochromatic ocular aberrations of human eyes as a function of accommodation by the Howland aberroscope technique. Vision Res. 1995 Feb;35(3):313–323. doi: 10.1016/0042-6989(94)00139-d. [DOI] [PubMed] [Google Scholar]
- Atchison D. A. Optical design of intraocular lenses. I. On-axis performance. Optom Vis Sci. 1989 Aug;66(8):492–506. doi: 10.1097/00006324-198908000-00002. [DOI] [PubMed] [Google Scholar]
- Atchison D. A. Optical design of intraocular lenses. II. Off-axis performance. Optom Vis Sci. 1989 Sep;66(9):579–590. doi: 10.1097/00006324-198909000-00003. [DOI] [PubMed] [Google Scholar]
- Campbell F. W., Green D. G. Optical and retinal factors affecting visual resolution. J Physiol. 1965 Dec;181(3):576–593. doi: 10.1113/jphysiol.1965.sp007784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douthwaite W. A., Sheridan M. The measurement of the corneal ellipse for the contact lens practitioner. Ophthalmic Physiol Opt. 1989 Jul;9(3):239–242. doi: 10.1111/j.1475-1313.1989.tb00900.x. [DOI] [PubMed] [Google Scholar]
- Eghbali F., Yeung K. K., Maloney R. K. Topographic determination of corneal asphericity and its lack of effect on the refractive outcome of radial keratotomy. Am J Ophthalmol. 1995 Mar;119(3):275–280. doi: 10.1016/s0002-9394(14)71167-5. [DOI] [PubMed] [Google Scholar]
- Gayton J. L., Sanders V. N. Implanting two posterior chamber intraocular lenses in a case of microphthalmos. J Cataract Refract Surg. 1993 Nov;19(6):776–777. doi: 10.1016/s0886-3350(13)80349-5. [DOI] [PubMed] [Google Scholar]
- Guillon M., Lydon D. P., Wilson C. Corneal topography: a clinical model. Ophthalmic Physiol Opt. 1986;6(1):47–56. [PubMed] [Google Scholar]
- Holladay J. T., Gills J. P., Leidlein J., Cherchio M. Achieving emmetropia in extremely short eyes with two piggyback posterior chamber intraocular lenses. Ophthalmology. 1996 Jul;103(7):1118–1123. doi: 10.1016/s0161-6420(96)30558-7. [DOI] [PubMed] [Google Scholar]
- Holladay J. T. Standardizing constants for ultrasonic biometry, keratometry, and intraocular lens power calculations. J Cataract Refract Surg. 1997 Nov;23(9):1356–1370. doi: 10.1016/s0886-3350(97)80115-0. [DOI] [PubMed] [Google Scholar]
- JENKINS T. C. ABERRATIONS OF THE EYE AND THEIR EFFECTS ON VISION: 1. SPHERICAL ABERRATION. Br J Physiol Opt. 1963 Apr-Jun;20:59–91. [PubMed] [Google Scholar]
- Lam A. K., Douthwaite W. A. Derivation of corneal flattening factor, p-value. Ophthalmic Physiol Opt. 1994 Oct;14(4):423–427. [PubMed] [Google Scholar]
- Millodot M., Sivak J. Contribution of the cornea and lens to the spherical aberration of the eye. Vision Res. 1979;19(6):685–687. doi: 10.1016/0042-6989(79)90244-x. [DOI] [PubMed] [Google Scholar]
- Sheridan M., Douthwaite W. A. Corneal asphericity and refractive error. Ophthalmic Physiol Opt. 1989 Jul;9(3):235–238. doi: 10.1111/j.1475-1313.1989.tb00899.x. [DOI] [PubMed] [Google Scholar]
- Shugar J. K., Lewis C., Lee A. Implantation of multiple foldable acrylic posterior chamber lenses in the capsular bag for high hyperopia. J Cataract Refract Surg. 1996;22 (Suppl 2):1368–1372. doi: 10.1016/s0886-3350(96)80100-3. [DOI] [PubMed] [Google Scholar]
- Sivak J. G., Kreuzer R. O. Spherical aberration of the crystalline lens. Vision Res. 1983;23(1):59–70. doi: 10.1016/0042-6989(83)90042-1. [DOI] [PubMed] [Google Scholar]
- Smith G., Pierscionek B. K., Atchison D. A. The optical modelling of the human lens. Ophthalmic Physiol Opt. 1991 Oct;11(4):359–369. [PubMed] [Google Scholar]
- el-Hage S. G., Berny F. Contribution of the crystalline lens to the spherical aberration of the eye. J Opt Soc Am. 1973 Feb;63(2):205–211. doi: 10.1364/josa.63.000205. [DOI] [PubMed] [Google Scholar]