Abstract
AIMS—To determine if patients with giant cell arteritis (GCA) treated with corticosteroids develop delayed visual loss or drug related ocular complications. METHODS—In a multicentre prospective study patients with GCA (using precise diagnostic criteria) had ophthalmic evaluations at predetermined intervals up to 1 year. The dose of corticosteroid was determined by treating physicians, often outside the study, with the daily dose reduced to the equivalent of 30-40 mg of prednisone within 5 weeks. Subsequently, treatment guidelines suggested that the dose be reduced as tolerated or the patient was withdrawn from steroids in a period not less than 6 months. RESULTS—At presentation, of the 22 patients enrolled, seven patients had nine eyes with ischaemic injury. Four eyes had improved visual acuity by two lines or more within 1 month of starting corticosteroids. No patients developed late visual loss as the steroid dose was reduced. At 1 year the visual acuity, contrast sensitivity, colour vision, and threshold perimetry were not significantly different from the 4-5 week determinations. At 1 year, there were no significant cataractous or glaucomatous changes. At 2 months, there was no difference in systemic complications between patients who received conventional dose (60-80 mg per day) or very high doses (200-1000 mg per day) of corticosteroids at the start or early in the course. CONCLUSIONS—Patients with GCA related visual loss can improve with treatment. Corticosteroids with starting doses of 60-1000 mg per day, with reduction to daily doses of 40-50 mg per day given for 4-6 weeks, and gradual dose reduction thereafter, as clinically permitted, did not result in delayed visual loss. There were no significant drug related ophthalmic complications.
Full Text
The Full Text of this article is available as a PDF (120.1 KB).
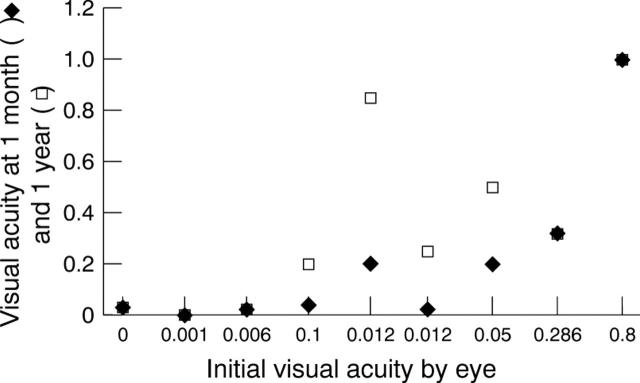
Figure 1 .
Changes in visual acuity expressed by eye as a decimal value. Recall three eyes in two patients had better pre-entry acuity which deteriorated within 5 days on oral prednisone.
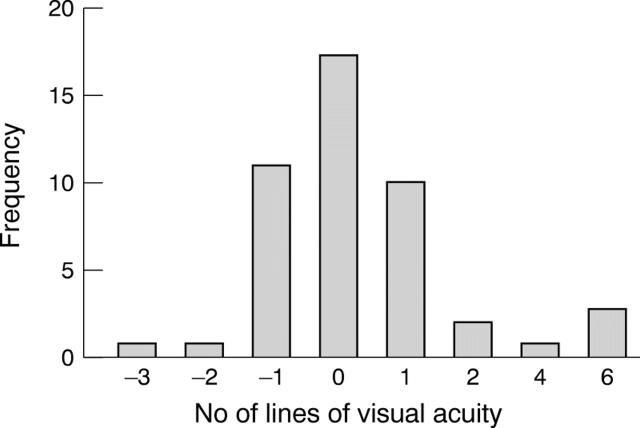
Figure 2 .
Changes in visual acuity at 1 year. Positive numbers indicate improvement and negative numbers, worsening. Frequency is expressed as number of eyes.
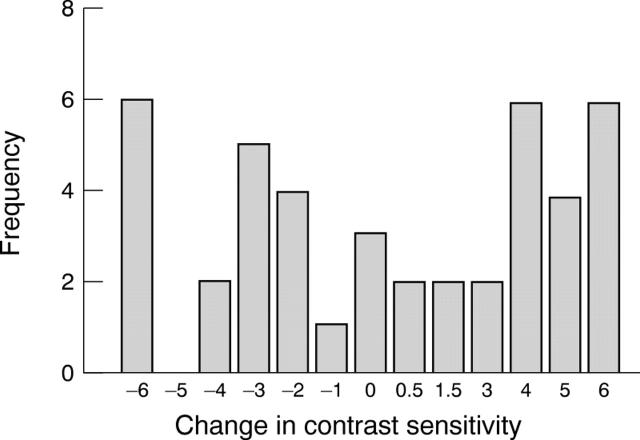
Figure 3 .
Change in contrast at 1 year from baseline expressed in log units ×10−1. Positive numbers indicate improvement and negative numbers, worsening. Frequency is expressed as number of eyes.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adhikary H. P., Sells R. A., Basu P. K. Ocular complications of systemic steroid after renal transplantation and their association with HLA. Br J Ophthalmol. 1982 May;66(5):290–291. doi: 10.1136/bjo.66.5.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiello P. D., Trautmann J. C., McPhee T. J., Kunselman A. R., Hunder G. G. Visual prognosis in giant cell arteritis. Ophthalmology. 1993 Apr;100(4):550–555. doi: 10.1016/s0161-6420(93)31608-8. [DOI] [PubMed] [Google Scholar]
- Beevers D. G., Harpur J. E., Turk K. A. Giant cell arteritis--the need for prolonged treatment. J Chronic Dis. 1973 Sep;26(9):571–584. doi: 10.1016/0021-9681(73)90062-3. [DOI] [PubMed] [Google Scholar]
- Blumberg S., Giansiracusa D. F., Docken W. P., Kantrowitz F. G. Recurrence of temporal arteritis. Clinical recurrence nine years after initial illness. JAMA. 1980 Oct 10;244(15):1713–1713. [PubMed] [Google Scholar]
- Chylack L. T., Jr, Leske M. C., Sperduto R., Khu P., McCarthy D. Lens Opacities Classification System. Arch Ophthalmol. 1988 Mar;106(3):330–334. doi: 10.1001/archopht.1988.01060130356020. [DOI] [PubMed] [Google Scholar]
- Cullen J. F. Temporal arteritis. Occurrence of ocular complications 7 years after diagnosis. Br J Ophthalmol. 1972 Aug;56(8):584–588. doi: 10.1136/bjo.56.8.584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cumming R. G., Mitchell P., Leeder S. R. Use of inhaled corticosteroids and the risk of cataracts. N Engl J Med. 1997 Jul 3;337(1):8–14. doi: 10.1056/NEJM199707033370102. [DOI] [PubMed] [Google Scholar]
- Delecoeuillerie G., Joly P., Cohen de Lara A., Paolaggi J. B. Polymyalgia rheumatica and temporal arteritis: a retrospective analysis of prognostic features and different corticosteroid regimens (11 year survey of 210 patients). Ann Rheum Dis. 1988 Sep;47(9):733–739. doi: 10.1136/ard.47.9.733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faarvang K. L., Pontoppidan Thyssen E. Giant cell arteritis: loss of vision during corticosteroid therapy. J Intern Med. 1989 Mar;225(3):215–216. doi: 10.1111/j.1365-2796.1989.tb00066.x. [DOI] [PubMed] [Google Scholar]
- Godel V., Feiler-Ofry V., Stein R. Systemic steroids and ocular fluid dynamics. I. Analysis of the sample as a whole. Influence of dosage and duration of therapy. Acta Ophthalmol (Copenh) 1972;50(5):655–663. doi: 10.1111/j.1755-3768.1972.tb06606.x. [DOI] [PubMed] [Google Scholar]
- Godel V., Feiler-Ofry V., Stein R. Systemic steroids and ocular fluid dynamics. II. Systemic versus topical steroids. Acta Ophthalmol (Copenh) 1972;50(5):664–676. doi: 10.1111/j.1755-3768.1972.tb06607.x. [DOI] [PubMed] [Google Scholar]
- Graham E., Holland A., Avery A., Russell R. W. Prognosis in giant-cell arteritis. Br Med J (Clin Res Ed) 1981 Jan 24;282(6260):269–271. doi: 10.1136/bmj.282.6260.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HOLLENHORST R. W., BROWN J. R., WAGENER H. P., SHICK R. M. Neurologic aspects of temporal arteritis. Neurology. 1960 May;10:490–498. doi: 10.1212/wnl.10.5.490. [DOI] [PubMed] [Google Scholar]
- Hamilton C. R., Jr, Shelley W. M., Tumulty P. A. Giant cell arteritis: including temporal arteritis and polymyalgia rheumatica. Medicine (Baltimore) 1971 Jan;50(1):1–27. [PubMed] [Google Scholar]
- Healey L. A., Wilske K. R. Manifestations of giant cell arteritis. Med Clin North Am. 1977 Mar;61(2):261–270. doi: 10.1016/s0025-7125(16)31331-1. [DOI] [PubMed] [Google Scholar]
- Henkind P., Charles N. C., Pearson J. Histopathology of ischemic optic neuropathy. Am J Ophthalmol. 1970 Jan;69(1):78–90. doi: 10.1016/0002-9394(70)91859-3. [DOI] [PubMed] [Google Scholar]
- Hunder G. G., Bloch D. A., Michel B. A., Stevens M. B., Arend W. P., Calabrese L. H., Edworthy S. M., Fauci A. S., Leavitt R. Y., Lie J. T. The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis Rheum. 1990 Aug;33(8):1122–1128. doi: 10.1002/art.1780330810. [DOI] [PubMed] [Google Scholar]
- Huston K. A., Hunder G. G., Lie J. T., Kennedy R. H., Elveback L. R. Temporal arteritis: a 25-year epidemiologic, clinical, and pathologic study. Ann Intern Med. 1978 Feb;88(2):162–167. doi: 10.7326/0003-4819-88-2-162. [DOI] [PubMed] [Google Scholar]
- Kyle V., Hazleman B. L. Treatment of polymyalgia rheumatica and giant cell arteritis. I. Steroid regimens in the first two months. Ann Rheum Dis. 1989 Aug;48(8):658–661. doi: 10.1136/ard.48.8.658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leske M. C., Chylack L. T., Jr, Sperduto R., Khu P., Wu S. Y., McCarthy D. Evaluation of a Lens Opacities Classification System. Arch Ophthalmol. 1988 Mar;106(3):327–329. doi: 10.1001/archopht.1988.01060130353019. [DOI] [PubMed] [Google Scholar]
- Liu G. T., Glaser J. S., Schatz N. J., Smith J. L. Visual morbidity in giant cell arteritis. Clinical characteristics and prognosis for vision. Ophthalmology. 1994 Nov;101(11):1779–1785. doi: 10.1016/s0161-6420(94)31102-x. [DOI] [PubMed] [Google Scholar]
- Meli B., Landau K., Gloor B. P. Die Tücken der Riesenzellarteriitis aus ophthalmologischer Sicht. Schweiz Med Wochenschr. 1996 Oct 26;126(43):1821–1828. [PubMed] [Google Scholar]
- Myles A. B., Perera T., Ridley M. G. Prevention of blindness in giant cell arteritis by corticosteroid treatment. Br J Rheumatol. 1992 Feb;31(2):103–105. doi: 10.1093/rheumatology/31.2.103. [DOI] [PubMed] [Google Scholar]
- Rosenfeld S. I., Kosmorsky G. S., Klingele T. G., Burde R. M., Cohn E. M. Treatment of temporal arteritis with ocular involvement. Am J Med. 1986 Jan;80(1):143–145. doi: 10.1016/0002-9343(86)90066-5. [DOI] [PubMed] [Google Scholar]
- Sorensen P. S., Lorenzen I. Kaempecellearteritis. Arteritis temporalis og polymyalgia rheumatica. Ugeskr Laeger. 1975 May 19;137(21):1135–1141. [PubMed] [Google Scholar]
- Thystrup J., Knudsen G. M., Mogensen A. M., Fledelius H. C. Atypical visual loss in giant cell arteritis. Acta Ophthalmol (Copenh) 1994 Dec;72(6):759–764. doi: 10.1111/j.1755-3768.1994.tb04696.x. [DOI] [PubMed] [Google Scholar]
- Urban R. C., Jr, Cotlier E. Corticosteroid-induced cataracts. Surv Ophthalmol. 1986 Sep-Oct;31(2):102–110. doi: 10.1016/0039-6257(86)90077-9. [DOI] [PubMed] [Google Scholar]
- WAGENER H. P., HOLLENHORST R. W. The ocular lesions of temporal arteritis. Am J Ophthalmol. 1958 May;45(5):617–630. [PubMed] [Google Scholar]
- Wilkinson I. M., Russell R. W. Arteries of the head and neck in giant cell arteritis. A pathological study to show the pattern of arterial involvement. Arch Neurol. 1972 Nov;27(5):378–391. doi: 10.1001/archneur.1972.00490170010003. [DOI] [PubMed] [Google Scholar]
- van der Veen M. J., Dinant H. J., van Booma-Frankfort C., van Albada-Kuipers G. A., Bijlsma J. W. Can methotrexate be used as a steroid sparing agent in the treatment of polymyalgia rheumatica and giant cell arteritis? Ann Rheum Dis. 1996 Apr;55(4):218–223. doi: 10.1136/ard.55.4.218. [DOI] [PMC free article] [PubMed] [Google Scholar]