Abstract
AIM—This study was designed to test the ability of a portable computer driven, head mounted visual field testing system to perform automated perimetry on patients at their bedside and to compare these results with the "gold standard" for bedside examinations, confrontation visual fields. METHODS—The Kasha visual field system is a portable automated perimeter which utilises a virtual reality headset. 37 neurosurgery patients were examined at their bedside with a central 24 degree suprathreshold testing strategy after confrontation visual field testing. The patterns of visual field defects were categorised and compared with the results of confrontation testing. RESULTS—A total of 42 field examinations were completed on 37 patients, and the average testing time for both eyes was 4.8 minutes with the perimetry system. Each of the 11 fields (100%) classified with defects on confrontation testing was similarly categorised on head mounted perimetry. 26 out of 31 (84%) visual fields were normal on both confrontation and perimetry testing, while five out of the 31 fields (16%) which were full on confrontation had visual field defects identified by head mounted perimetry. CONCLUSION—The head mounted, automated perimetry system proved easily portable and convenient for examining neurosurgical patients at their bedside in the perioperative period. The device demonstrated equal sensitivity to confrontation visual field testing methods in detecting field defects and offers the advantage of standardised, quantifiable testing with graphic results for follow up examinations.
Full Text
The Full Text of this article is available as a PDF (186.3 KB).
Figure 1 .
Head mounted perimetry test in progress with perimetrist monitoring examination on the computer screen.
Figure 2 .
Head mounted perimetry field of a 58 year old man 4 days after a transsphenoid resection of a pituitary adenoma, with a classic bitemporal field defect consistent with chiasmal dysfunction.
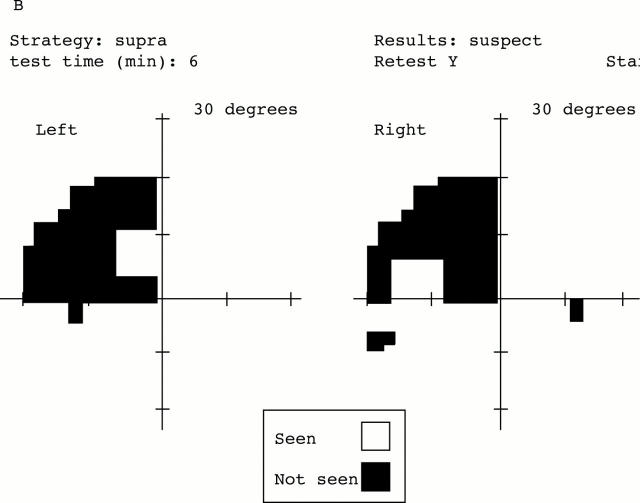
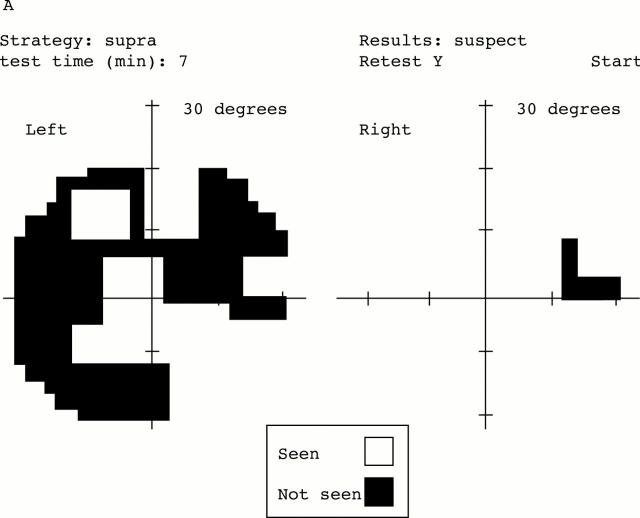
Figure 3 .
Head mounted perimetry fields of a 37 year old man taken preoperatively (A) and 2 days following a right temporal lobe resection for an anaplastic astrocytoma (B). The left superior homonomous quadrant defect is consistent with the right temporal lobe resection.
Figure 4 .

Head mounted perimetry field of a 34 year old woman 3 days following a craniotomy for central nervous system sarcoid (A). The three quadrant defect in the left eye (B) and enlarged blind spot in the right eye correlated well with the results of a Humphrey field examination performed 3 months earlier (C).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bickler-Bluth M., Trick G. L., Kolker A. E., Cooper D. G. Assessing the utility of reliability indices for automated visual fields. Testing ocular hypertensives. Ophthalmology. 1989 May;96(5):616–619. doi: 10.1016/s0161-6420(89)32840-5. [DOI] [PubMed] [Google Scholar]
- Katz J., Sommer A. Reliability indexes of automated perimetric tests. Arch Ophthalmol. 1988 Sep;106(9):1252–1254. doi: 10.1001/archopht.1988.01060140412043. [DOI] [PubMed] [Google Scholar]
- Katz J., Sommer A., Witt K. Reliability of visual field results over repeated testing. Ophthalmology. 1991 Jan;98(1):70–75. doi: 10.1016/s0161-6420(91)32339-x. [DOI] [PubMed] [Google Scholar]
- Keltner J. L., Johnson C. A. Screening for visual field abnormalities with automated perimetry. Surv Ophthalmol. 1983 Nov-Dec;28(3):175–183. doi: 10.1016/0039-6257(83)90094-2. [DOI] [PubMed] [Google Scholar]
- Keltner J. L., Johnson C. A., Spurr J. O., Beck R. W. Baseline visual field profile of optic neuritis. The experience of the optic neuritis treatment trial. Optic Neuritis Study Group. Arch Ophthalmol. 1993 Feb;111(2):231–234. doi: 10.1001/archopht.1993.01090020085029. [DOI] [PubMed] [Google Scholar]
- Keltner J. L., Johnson C. A., Spurr J. O., Beck R. W. Visual field profile of optic neuritis. One-year follow-up in the Optic Neuritis Treatment Trial. Arch Ophthalmol. 1994 Jul;112(7):946–953. doi: 10.1001/archopht.1994.01090190094027. [DOI] [PubMed] [Google Scholar]
- Reitner A., Tittl M., Ergun E., Baradaran-Dilmaghani R. The efficient use of perimetry for neuro-ophthalmic diagnosis. Br J Ophthalmol. 1996 Oct;80(10):903–905. doi: 10.1136/bjo.80.10.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siatkowski R. M., Lam B. L., Anderson D. R., Feuer W. J., Halikman A. M. Automated suprathreshold static perimetry screening for detecting neuro-ophthalmologic disease. Ophthalmology. 1996 Jun;103(6):907–917. doi: 10.1016/s0161-6420(96)30588-5. [DOI] [PubMed] [Google Scholar]
- Trobe J. D., Acosta P. C., Krischer J. P., Trick G. L. Confrontation visual field techniques in the detection of anterior visual pathway lesions. Ann Neurol. 1981 Jul;10(1):28–34. doi: 10.1002/ana.410100105. [DOI] [PubMed] [Google Scholar]
- Younge B. R. Computer-assisted perimetry in visual pathway disease: neuro-ophthalmic applications. Trans Am Ophthalmol Soc. 1984;82:899–942. [PMC free article] [PubMed] [Google Scholar]