Abstract
AIMS—To evaluate the clinical course and the characteristics of transient refractive error occurring during intensive glycaemic control of severe hyperglycaemia. METHODS—28 eyes of patients with persistent diabetes were included in this prospective study. During the observation period, patients underwent general ophthalmological examination and A-mode scan ultrasonography was performed at each examination—at days 1, 3, and 7, and then once every week or every other week until recovery of hyperopia. RESULTS—A transient hyperopic change occurred in all patients receiving improved control after hyperglycaemia. Hyperopic change developed a mean of 3.4 (SD 2.0) days after the onset of treatment, and reached a peak at 10.3 (6.1) days, where the maximum hyperopic change in an eye was 1.47 (0.87) D (range 0.50-3.75 D). Recovery of the previous refraction occurred between 14 and 84 days after the initial assessment. There was a positive correlation between the magnitude of the maximum hyperopic change and (1) the plasma glucose concentration on admission (p<0.01), (2) the HbA1c level on admission (p<0.005), (3) the daily rate of plasma glucose reduction over the first 7 days of treatment (p<0.001), (4) the number of days required for hyperopia to reach its peak (p<0.001), and (5) the number of days required for the development and resolution of hyperopic changes (p<0.0001). There was a negative correlation between the maximum hyperopic change of an eye and baseline value of refraction (p<0.01). During transient hyperopia, no significant changes were observed in the radius of the anterior corneal curvature, axial length, lens thickness, or depth of anterior chamber. CONCLUSIONS—The degree of transient hyperopia associated with rapid correction of hyperglycaemia is highly dependent on the rate of reduction of the plasma glucose level. A reduction of refractive index in intraocular tissues, especially in lens, appears to be responsible for this hyperopic change.
Full Text
The Full Text of this article is available as a PDF (119.3 KB).
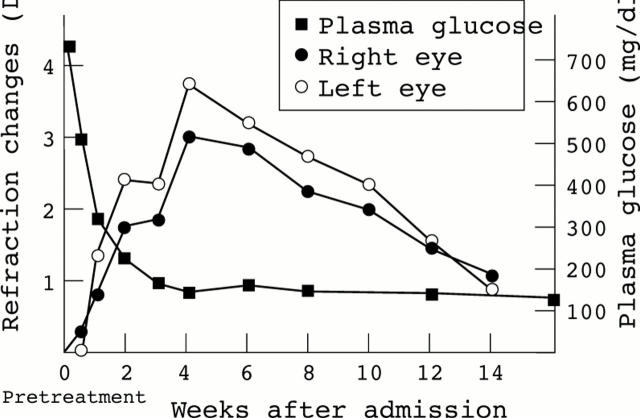
Figure 1 .
Change of refraction and of plasma glucose concentration in a diabetic patient (case 4) over a period of 16 weeks after starting intensive glycaemic control on day 0. The change of refraction in an eye at a given time point represents the difference between the refractive error on that day and the refractive error at the time of admission. Transient bilateral hyperopic change was similar in both eyes, and appeared in response to a rapid reduction in plasma glucose.
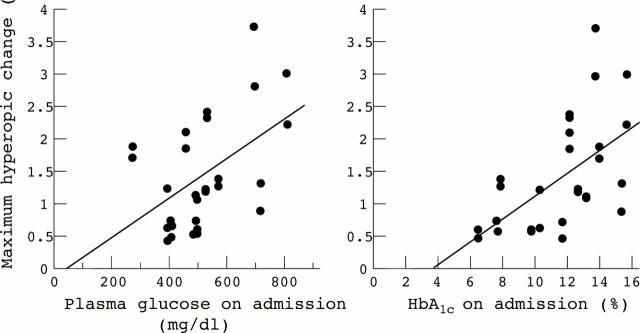
Figure 2 .
Relation between maximum hyperopic change of an eye (dioptres) and the plasma glucose concentration (mg/dl) on admission (left). There was a significant positive correlation between them (r=0.49, p<0.01). Relation between maximum hyperopic change of an eye (dioptres) and HbA1c (%) on admission (right). There was a significant positive correlation between them (r=0.57, p<0.005).
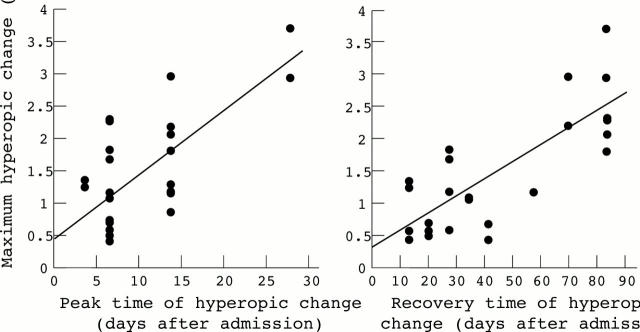
Figure 3 .
Relation between maximum hyperopic change of an eye (dioptres) and the day on which the maximum hyperopic change was attained (left). There was a significant positive correlation between them (r=0.68, p<0.001). Relation between maximum hyperopic change of an eye (dioptres) and the day on which the patient recovered from hyperopia (right). There was a significant positive correlation between them (r=0.78, p<0.0001).
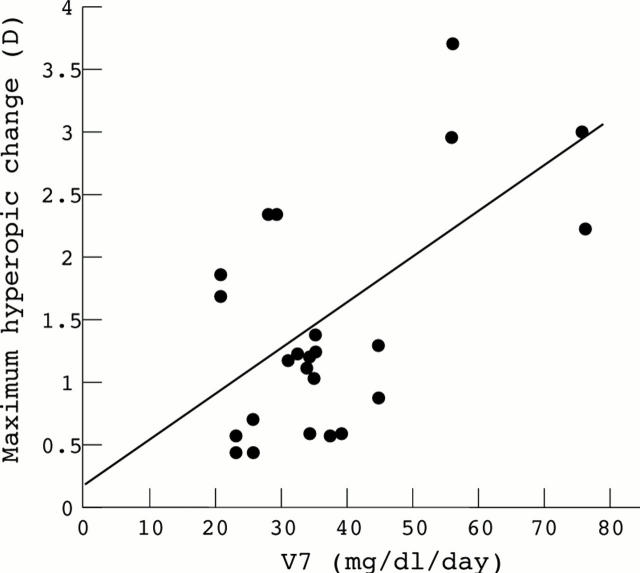
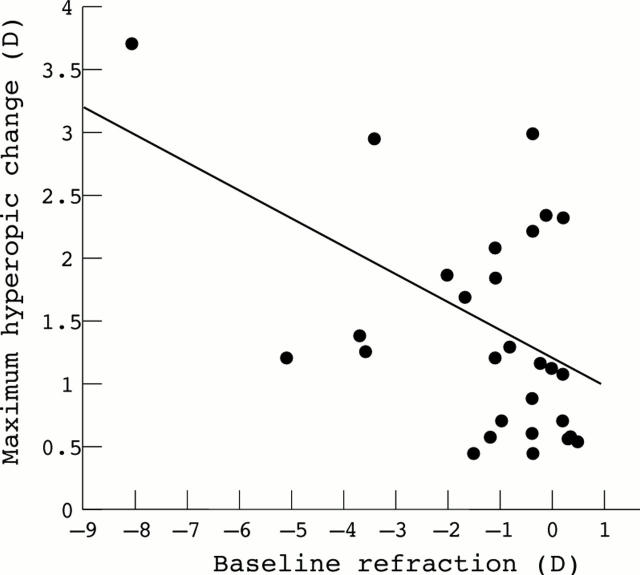
Figure 4 .
Relation between maximum hyperopic change of an eye and the daily rate of plasma glucose reduction over the first 7 days of treatment. There is a positive correlation between them (r=0.59, p<0.001).
Figure 5 .
Relation between maximum hyperopic change of an eye and baseline refraction of the eye. There is a negative correlation between them (r=−0.48, p<0.01).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Butler P. A. Reversible cataracts in diabetes mellitus. J Am Optom Assoc. 1994 Aug;65(8):559–563. [PubMed] [Google Scholar]
- Dickey J. B., Daily M. J. Transient posterior subcapsular lens opacities in diabetes mellitus. Am J Ophthalmol. 1993 Feb 15;115(2):234–238. doi: 10.1016/s0002-9394(14)73929-7. [DOI] [PubMed] [Google Scholar]
- Duke-Elder W. S. CHANGES IN REFRACTION IN DIABETES MELLITUS. Br J Ophthalmol. 1925 Apr;9(4):167–187. doi: 10.1136/bjo.9.4.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eva P. R., Pascoe P. T., Vaughan D. G. Refractive change in hyperglycaemia: hyperopia, not myopia. Br J Ophthalmol. 1982 Aug;66(8):500–505. doi: 10.1136/bjo.66.8.500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fledelius H. C. Refractive change in diabetes mellitus around onset or when poorly controlled. A clinical study. Acta Ophthalmol (Copenh) 1987 Feb;65(1):53–57. doi: 10.1111/j.1755-3768.1987.tb08491.x. [DOI] [PubMed] [Google Scholar]
- Friberg T. R., Grove A. S., Jr Choroidal folds and refractive errors associated with orbital tumors. An analysis. Arch Ophthalmol. 1983 Apr;101(4):598–603. doi: 10.1001/archopht.1983.01040010598014. [DOI] [PubMed] [Google Scholar]
- Gabbay K. H. The sorbitol pathway and the complications of diabetes. N Engl J Med. 1973 Apr 19;288(16):831–836. doi: 10.1056/NEJM197304192881609. [DOI] [PubMed] [Google Scholar]
- Gelvin J. B., Thonn V. A. The formation and reversal of acute cataracts in diabetes mellitus. J Am Optom Assoc. 1993 Jul;64(7):471–474. [PubMed] [Google Scholar]
- Gwinup G., Villarreal A. Relationship of serum glucose concentration to changes in refraction. Diabetes. 1976 Jan;25(1):29–31. doi: 10.2337/diab.25.1.29. [DOI] [PubMed] [Google Scholar]
- HUGGERT A. The appearance of the crystalline lens during different stages of transitory changes of refraction. II. Acta Ophthalmol (Copenh) 1954;32(4):375–389. doi: 10.1111/j.1755-3768.1954.tb05057.x. [DOI] [PubMed] [Google Scholar]
- Hemenger R. P., Garner L. F., Ooi C. S. Change with age of the refractive index gradient of the human ocular lens. Invest Ophthalmol Vis Sci. 1995 Mar;36(3):703–707. [PubMed] [Google Scholar]
- KINOSHITA J. H., MEROLA L. O., SATOH K., DIKMAK E. Osmotic changes caused by the accumulation of dulcitol in the lenses of rats fed with galactose. Nature. 1962 Jun 16;194:1085–1087. doi: 10.1038/1941085a0. [DOI] [PubMed] [Google Scholar]
- Keller J. T. Letter: Hyperopia in diabetes. Arch Ophthalmol. 1973 Dec;90(6):511–512. doi: 10.1001/archopht.1973.01000050511024. [DOI] [PubMed] [Google Scholar]
- Marmor M. F. Transient accommodative paralysis and hyperopia in diabetes. Arch Ophthalmol. 1973 May;89(5):419–421. doi: 10.1001/archopht.1973.01000040421014. [DOI] [PubMed] [Google Scholar]
- Perkins E. S. Cataract: refractive error, diabetes, and morphology. Br J Ophthalmol. 1984 May;68(5):293–297. doi: 10.1136/bjo.68.5.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Planten J. T. Changes of refraction in the adult eye due to changing refractive indices of the layers of the lens. Ophthalmologica. 1981;183(2):86–90. doi: 10.1159/000309145. [DOI] [PubMed] [Google Scholar]
- Saito Y., Ohmi G., Kinoshita S., Nakamura Y., Ogawa K., Harino S., Okada M. Transient hyperopia with lens swelling at initial therapy in diabetes. Br J Ophthalmol. 1993 Mar;77(3):145–148. doi: 10.1136/bjo.77.3.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santa Cruz C. S., Culotta T., Cohen E. J., Rapuano C. J. Chalazion-induced hyperopia as a cause of decreased vision. Ophthalmic Surg Lasers. 1997 Aug;28(8):683–684. [PubMed] [Google Scholar]
- Smith G., Atchison D. A., Pierscionek B. K. Modeling the power of the aging human eye. J Opt Soc Am A. 1992 Dec;9(12):2111–2117. doi: 10.1364/josaa.9.002111. [DOI] [PubMed] [Google Scholar]
- Willi M. J. Hyperopia and hyperglycemia. Surv Ophthalmol. 1996 Sep-Oct;41(2):187–187. doi: 10.1016/s0039-6257(96)80019-1. [DOI] [PubMed] [Google Scholar]