Abstract
AIMS—To analyse the histopathology of "deep retinal vascular anomalous complex" or "chorioretinal anastomosis". METHODS—Six patients with a deep retinal vascular anomalous complex (age range 66-88 years) had fundus photography and fluorescein angiography not more than 14 days before foveal translocation surgery. Four patients were also documented with indocyanine green angiography. The surgical specimens were serially sectioned and stained in a stepped fashion with Masson trichrome, periodic acid Schiff, and phosphotungstic acid haematoxylin, a histochemical stain for fibrin. RESULTS—A subretinal fibrovascular membrane was surrounded by a rim consisting of diffuse drusen (basal laminar deposits), retinal pigment epithelium, and amorphous, fibrinous material interspersed with remains of outer segments in all specimens. In two specimens vascular structures were identified that left the specimen towards the retina. Amorphous material with the remains of outer segments was not found on the retinal side of the fibrovascular tissue itself but in four specimens a small neuroretinal portion (outer nuclear layer) was adherent to the complex. In three specimens a thin fibrocellular membrane was seen at the choroidal side of the diffuse drusen. CONCLUSION—Deep retinal vascular anomalous complex represents histologically neovascularisation growing out of the neuroretina, into the subretinal space, which mimics choroidal neovascularisation. The term therefore appears rightly chosen.
Full Text
The Full Text of this article is available as a PDF (209.7 KB).
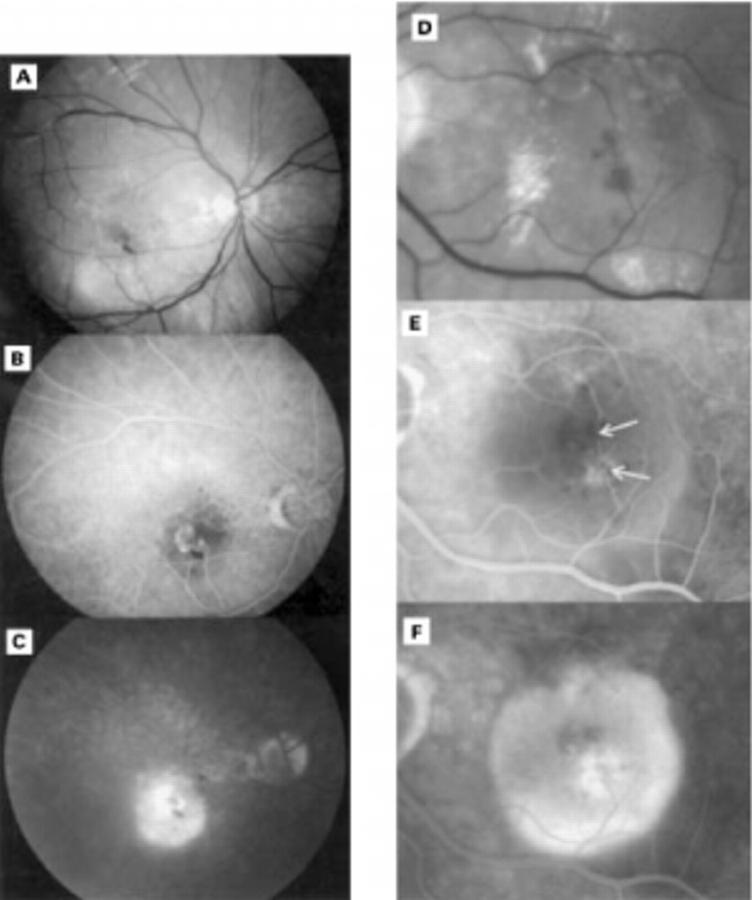
Figure 1 .
(A), (B), and (C) respectively red-free, venous, and late phase fluorescein angiography of a 71 year old patient. Intraretinal lipid exudates and haemorrhages are seen on the red-free photograph. A subretinal neovascular net is seen in the right eye which appears connected to at least two retinal vessels in the early phase. The hyperfluorescence of this deep retinal vascular anomalous complex persists in the late phase. The associated retinal pigment epithelial detachment appears hypofluorescent in the early phase but becomes hyperfluorescent in the late phase. (D), (E), and (F) respectively enlarged red-free, venous, and late phase fluorescein angiography of a 70 year old patient. Intraretinal lipid exudates and haemorrhages are seen, arrows indicate retinal vessels that appear to dip into the deep retinal vascular anomalous complex. The associated serous pigment epithelial detachment is clearly demonstrated in the late phase.
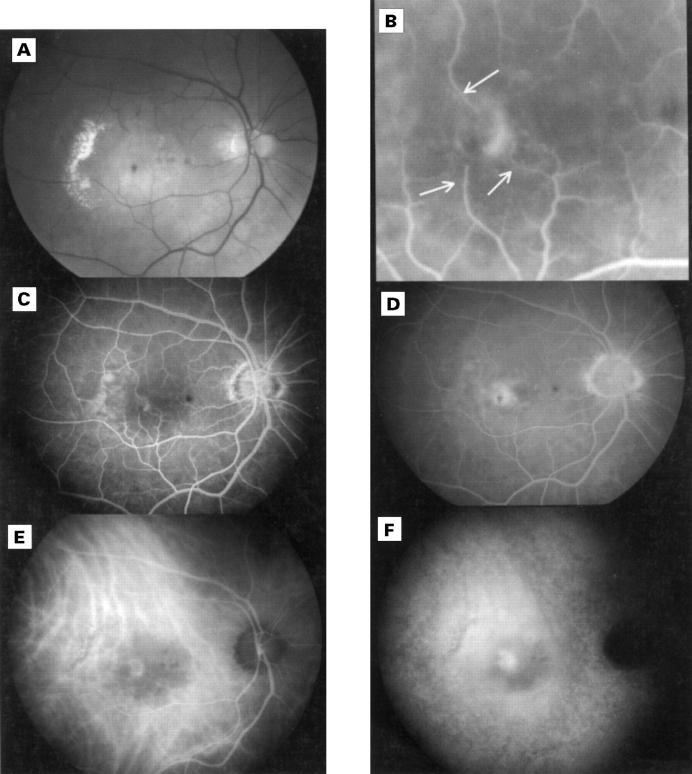
Figure 2 .
Red-free (A) fluorescein angiogram (B, C, and D) and indocyanine green angiogram of a 73 year old patient. On the red-free photograph, intraretinal lipid exudates, haemorrhages, and a drusenoid pigment epithelial detachment can be seen. Fluorescein angiography indicates a deep retinal vascular anomalous complex that appears to be connected to three retinal vessels (arrows). The venous (E) and late phase (F) indocyanine green angiogram identifies a vascular net. The lesion persists as a hot spot in the late phase, entirely within a hypofluorescent zone corresponding to the retinal pigment epithelial detachment.
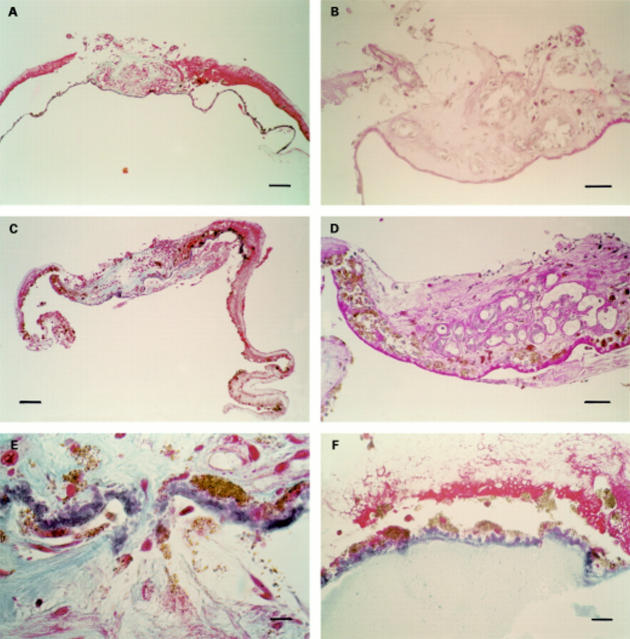
Figure 3 .
(A) MTC stain, bar = 100 µm, overview of specimen corresponding to Figure 2. A subretinal central fibrovascular nodule is seen surrounded by a rim composed of amorphous material, retinal pigment epithelium, and diffuse drusen. (B) PAS stain, bar = 50 µm, detail of same specimen as (A). The fibrovascular tissue immediately contacts the diffuse drusen. Some vessels leave the specimen towards the retina. (C) MTC stain, bar = 100 µm, overview of specimen corresponding to Figure 1A, B, C. A central fibrovascular nodule is seen, consisting both of a subretinal vascular component and an intra-Bruch's fibrocellular component, with surrounding rim. (D) PAS stain, bar = 50 µm, detail of same specimen as (C). A rich vasculature is demonstrated in the subretinal part of the specimen. (E) MTC stain, bar 10 µm, detail of same specimen as (C). An interruption of the diffuse drusen layer is seen with a fibrous tissue connecting the subretinal with the intra-Bruch's component. (F) MTC stain, bar 25 µm, detail of a third specimen, at the level of the rim. Pale staining, fine granular material is seen at the choroidal side of the diffuse drusen.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bellhorn R. W., Bellhorn M., Friedman A. H., Henkind P. Urethan-induced retinopathy in pigmented rats. Invest Ophthalmol. 1973 Jan;12(1):65–76. [PubMed] [Google Scholar]
- Bellhorn R. W., Burns M. S., Benjamin J. V. Retinal vessel abnormalities of phototoxic retinopathy in rats. Invest Ophthalmol Vis Sci. 1980 Jun;19(6):584–595. [PubMed] [Google Scholar]
- Berger A. S., McCuen B. W., 2nd, Brown G. C., Brownlow R. L., Jr Surgical removal of subfoveal neovascularization in idiopathic juxtafoveolar retinal telangiectasis. Retina. 1997;17(2):94–98. doi: 10.1097/00006982-199703000-00002. [DOI] [PubMed] [Google Scholar]
- Bird A. C., Bressler N. M., Bressler S. B., Chisholm I. H., Coscas G., Davis M. D., de Jong P. T., Klaver C. C., Klein B. E., Klein R. An international classification and grading system for age-related maculopathy and age-related macular degeneration. The International ARM Epidemiological Study Group. Surv Ophthalmol. 1995 Mar-Apr;39(5):367–374. doi: 10.1016/s0039-6257(05)80092-x. [DOI] [PubMed] [Google Scholar]
- Caldwell R. B. Blood-retinal barrier changes in the retinal pigment epithelium of RCS rats with inherited retinal degeneration. Prog Clin Biol Res. 1987;247:333–347. [PubMed] [Google Scholar]
- Eliassi-Rad B., Green W. R. Histopathologic study of presumed parafoveal telangiectasis. Retina. 1999;19(4):332–335. doi: 10.1097/00006982-199907000-00011. [DOI] [PubMed] [Google Scholar]
- Gass J. D., Blodi B. A. Idiopathic juxtafoveolar retinal telangiectasis. Update of classification and follow-up study. Ophthalmology. 1993 Oct;100(10):1536–1546. [PubMed] [Google Scholar]
- Green W. R., Enger C. Age-related macular degeneration histopathologic studies. The 1992 Lorenz E. Zimmerman Lecture. Ophthalmology. 1993 Oct;100(10):1519–1535. doi: 10.1016/s0161-6420(93)31466-1. [DOI] [PubMed] [Google Scholar]
- Green W. R., Gass J. D. Senile disciform degeneration of the macula. Retinal arterialization of the fibrous plaque demonstrated clinically and histopathologically. Arch Ophthalmol. 1971 Nov;86(5):487–494. doi: 10.1001/archopht.1971.01000010489001. [DOI] [PubMed] [Google Scholar]
- Grossniklaus H. E., Green W. R. Histopathologic and ultrastructural findings of surgically excised choroidal neovascularization. Submacular Surgery Trials Research Group. Arch Ophthalmol. 1998 Jun;116(6):745–749. doi: 10.1001/archopht.116.6.745. [DOI] [PubMed] [Google Scholar]
- Grossniklaus H. E., Hutchinson A. K., Capone A., Jr, Woolfson J., Lambert H. M. Clinicopathologic features of surgically excised choroidal neovascular membranes. Ophthalmology. 1994 Jun;101(6):1099–1111. doi: 10.1016/s0161-6420(13)31216-0. [DOI] [PubMed] [Google Scholar]
- Hartnett M. E., Weiter J. J., Garsd A., Jalkh A. E. Classification of retinal pigment epithelial detachments associated with drusen. Graefes Arch Clin Exp Ophthalmol. 1992;230(1):11–19. doi: 10.1007/BF00166756. [DOI] [PubMed] [Google Scholar]
- Hartnett M. E., Weiter J. J., Staurenghi G., Elsner A. E. Deep retinal vascular anomalous complexes in advanced age-related macular degeneration. Ophthalmology. 1996 Dec;103(12):2042–2053. doi: 10.1016/s0161-6420(96)30389-8. [DOI] [PubMed] [Google Scholar]
- Korte G. E., Bellhorn R. W., Burns M. S. Urethane-induced rat retinopathy. Plasticity of the blood-retinal barrier in disease. Invest Ophthalmol Vis Sci. 1984 Sep;25(9):1027–1034. [PubMed] [Google Scholar]
- Kuhn D., Meunier I., Soubrane G., Coscas G. Imaging of chorioretinal anastomoses in vascularized retinal pigment epithelium detachments. Arch Ophthalmol. 1995 Nov;113(11):1392–1398. doi: 10.1001/archopht.1995.01100110052025. [DOI] [PubMed] [Google Scholar]
- Lafaut B. A., Bartz-Schmidt K. U., Vanden Broecke C., Aisenbrey S., De Laey J. J., Heimann K. Clinicopathological correlation in exudative age related macular degeneration: histological differentiation between classic and occult choroidal neovascularisation. Br J Ophthalmol. 2000 Mar;84(3):239–243. doi: 10.1136/bjo.84.3.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee B. L. Bilateral subretinal neovascular membrane in idiopathic juxtafoveolar telangiectasis. Retina. 1996;16(4):344–346. doi: 10.1097/00006982-199616040-00014. [DOI] [PubMed] [Google Scholar]
- O'Shea J. G. Age-related macular degeneration. Postgrad Med J. 1998 Apr;74(870):203–207. doi: 10.1136/pgmj.74.870.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park D., Schatz H., McDonald H. R., Johnson R. N. Fibrovascular tissue in bilateral juxtafoveal telangiectasis. Arch Ophthalmol. 1996 Sep;114(9):1092–1096. doi: 10.1001/archopht.1996.01100140294006. [DOI] [PubMed] [Google Scholar]
- Sarks S. H. New vessel formation beneath the retinal pigment epithelium in senile eyes. Br J Ophthalmol. 1973 Dec;57(12):951–965. doi: 10.1136/bjo.57.12.951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinding T. Visual impairment of age-related macular degeneration. An epidemiological study of 1000 aged individuals. Acta Ophthalmol (Copenh) 1990 Apr;68(2):162–167. doi: 10.1111/j.1755-3768.1990.tb01898.x. [DOI] [PubMed] [Google Scholar]