Abstract
BACKGROUND—The study of corneal endothelium, by specular microscopy, in patients with anterior uveitis has largely been restricted to observations on the endothelial cells. In this prospective study "keratic precipitates" (KP) in different types of uveitis were examined in different stages of the disease process and the endothelial changes occurring in the vicinity of the KP were evaluated in comparison with the endothelium of the uninvolved eye. METHODS—13 patients with active unilateral uveitis were recruited. The mean age was 42.9 years (range 20-76 years). A Tomey-1100 contact wide field specular (×10) microscope was used to capture endothelial images and KP until the resolution of uveitis. Data regarding type of uveitis, number, size, and nature of KP were recorded. Automated morphometric analysis was done for cell size, cell density and coefficient of variation, and statistical comparisons of cell size and cell density were made (Student's t test) between the endothelium in the vicinity of fresh and resolving KP, fresh KP and normal endothelium, and resolving KP and normal endothelium. RESULTS—On specular microscopy, fresh KP were seen as dense, white glistening deposits occupying 5-10 endothelial cells in diameter and fine KP were widely distributed and were one or two endothelial cells in diameter. The KP in Posner-Schlossman syndrome had a distinct and different morphology. With clinical remission of uveitis, the KP were observed to undergo characteristic morphological changes and old KP demonstrated a large, dark halo surrounding a central white deposit and occasionally a dark shadow or a "lacuna" replaced the site of the original KP. Endothelial blebs were noted as dark shadows or defects in the endothelial mosaic in patients with recurrent uveitis. There was significant statistical difference in the mean cell size and cell density of endothelial cells in the vicinity of fresh KP compared with normal endothelium of the opposite eye. CONCLUSION—This study elucidated the different specular microscopic features of KP in anterior uveitis. Distinct morphological features of large and fine KP were noted. These features underwent dramatic changes on resolution of uveitis. The endothelium was abnormal in the vicinity of KP, which returned to near normal values on resolution of uveitis.
Full Text
The Full Text of this article is available as a PDF (157.5 KB).
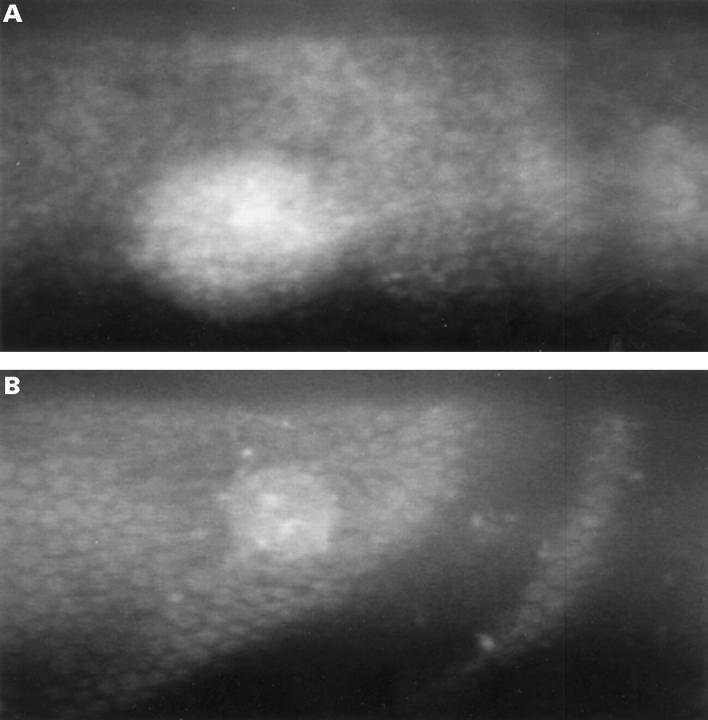
Figure 1 .
(A) and (B) Large fresh KP appearing as dense white deposits on endothelium.
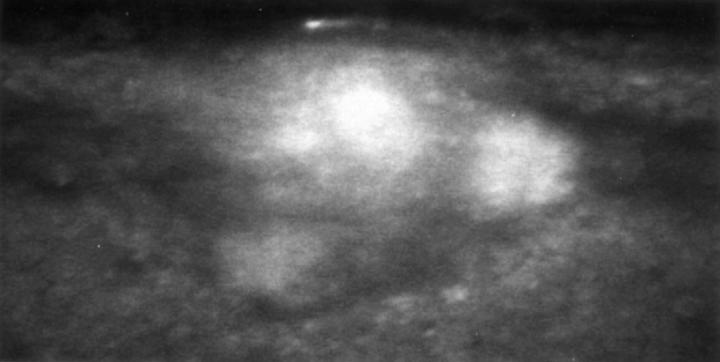
Figure 2 .
The solitary KP in Posner-Schlossman syndrome. Note the conglomeration of three individual KP connected by slender pseudopodia and the margin of the conglomerate distinct from the surrounding endothelium.
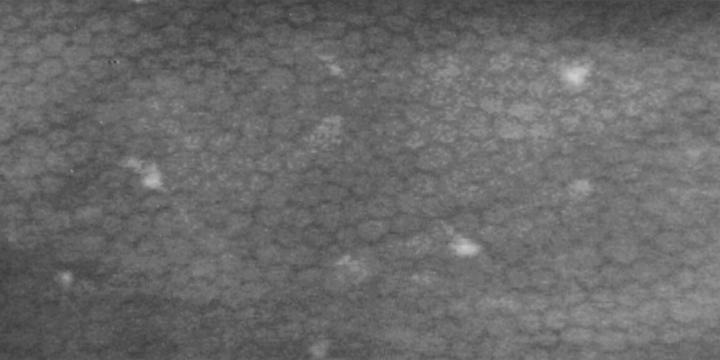
Figure 3 .
Fine KPs scattered on endothelium.
Figure 4 .
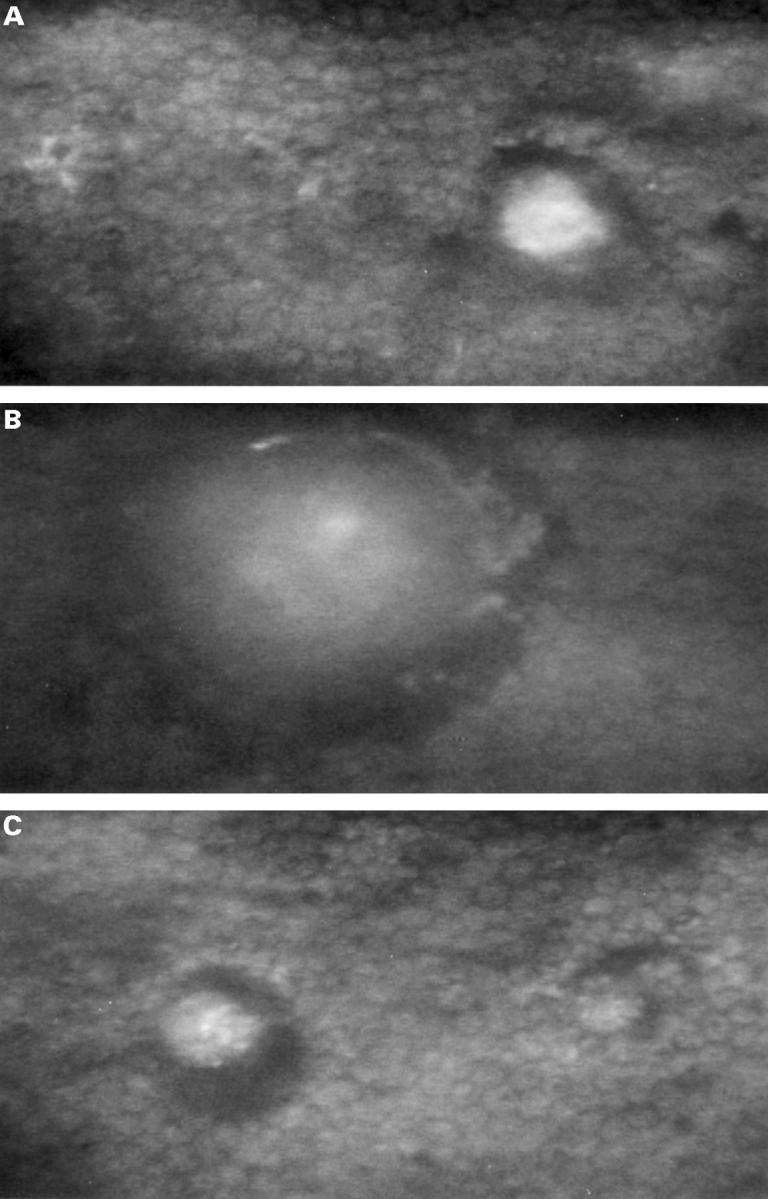
(A) and (B) Resolving KP. Note the appearance of a dark halo surrounding the glistening dense white centre and the gradual increase in the dark shadow in the periphery with the shrinkage of the central white deposit. (C) Old KP. Dark halo surrounding the central white deposit with indistinct cellular margins on resolution of uveitis.
Figure 5 .
Old KP. Note the dark halo completely replacing the original site of KP.
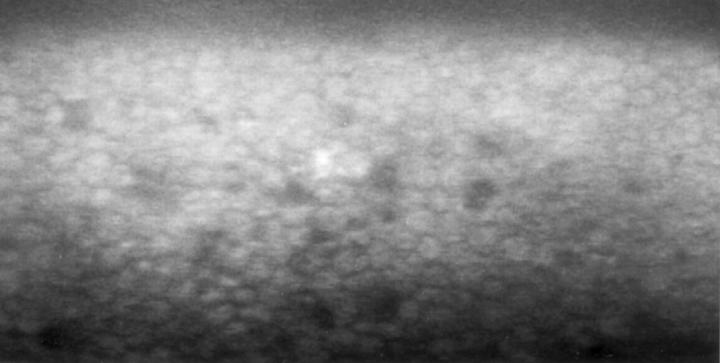
Figure 6 .
Endothelial blebs observed as dark shadows or defects in endothelium in recurrent uveitis.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brooks A. M., Grant G., Gillies W. E. Differentiation and assessment of corneal endothelial changes associated with diseases of the anterior segment of the eye. Aust N Z J Ophthalmol. 1987 Feb;15(1):65–70. doi: 10.1111/j.1442-9071.1987.tb00306.x. [DOI] [PubMed] [Google Scholar]
- Brooks A. M., Grant G., Gillies W. E. The use of specular microscopy to investigate unusual findings in the corneal endothelium and its adjacent structures. Aust N Z J Ophthalmol. 1988 Aug;16(3):235–243. doi: 10.1111/j.1442-9071.1988.tb01215.x. [DOI] [PubMed] [Google Scholar]
- Hartmann C., Köditz W. Automated morphometric endothelial analysis combined with video specular microscopy. Cornea. 1984;3(3):155–167. [PubMed] [Google Scholar]
- Hartmann C., Köditz W. Automated morphometric endothelial analysis combined with video specular microscopy. Cornea. 1984;3(3):155–167. [PubMed] [Google Scholar]
- Inomata H., Smelser G. K. Fine structural alterations of corneal endothelim during experimental uveitis. Invest Ophthalmol. 1970 Apr;9(4):272–285. [PubMed] [Google Scholar]
- Koester C. J., Roberts C. W., Donn A., Hoefle F. B. Wide field specular microscopy. Clinical and research applications. Ophthalmology. 1980 Sep;87(9):849–860. doi: 10.1016/s0161-6420(80)35150-6. [DOI] [PubMed] [Google Scholar]
- Lester J. M., McFarland J. L., Bursell S. E., Laing R. A., Brenner J. F. Automated morphometric analysis of corneal endothelial cells. Invest Ophthalmol Vis Sci. 1981 Mar;20(3):407–410. [PubMed] [Google Scholar]
- Olsen T. Changes in the corneal endothelium after acute anterior uveitis as seen with the specular microscope. Acta Ophthalmol (Copenh) 1980 Apr;58(2):250–256. doi: 10.1111/j.1755-3768.1980.tb05718.x. [DOI] [PubMed] [Google Scholar]
- Olsen T. Transient changes in specular appearance of the corneal endothelium and in corneal thickness during anterior uveitis. Acta Ophthalmol (Copenh) 1981 Feb;59(1):100–109. doi: 10.1111/j.1755-3768.1981.tb06717.x. [DOI] [PubMed] [Google Scholar]
- Price N. C., Cheng H. Contact and noncontact specular microscopy. Br J Ophthalmol. 1981 Aug;65(8):568–574. doi: 10.1136/bjo.65.8.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao G. N., Stevens R. E., Mandelberg A. I., Aquavella J. V. Morphologic variations in graft endothelium. Arch Ophthalmol. 1980 Aug;98(8):1403–1406. doi: 10.1001/archopht.1980.01020040255008. [DOI] [PubMed] [Google Scholar]
- Sherrard E. S., Buckley R. J. The relief mode. New application of the corneal specular microscope. Arch Ophthalmol. 1982 Feb;100(2):296–300. doi: 10.1001/archopht.1982.01030030298014. [DOI] [PubMed] [Google Scholar]
- Sugar A. Clinical specular microscopy. Surv Ophthalmol. 1979 Jul-Aug;24(1):21–32. doi: 10.1016/0039-6257(79)90144-9. [DOI] [PubMed] [Google Scholar]
- Walter K. A., Coulter V. L., Palay D. A., Taravella M. J., Grossniklaus H. E., Edelhauser H F. Corneal endothelial deposits in patients with cytomegalovirus retinitis. Am J Ophthalmol. 1996 Apr;121(4):391–396. doi: 10.1016/s0002-9394(14)70435-0. [DOI] [PubMed] [Google Scholar]