Abstract
AIM—To indicate that congenital idiopathic nystagmus (CIN) and sensory defect nystagmus (SDN) can be vertical or asymmetric in some children. METHODS—Of 276 children presenting with nystagmus for electrophysiological testing, 14 were identified as having CIN or SDN, yet had a nystagmus which was either vertical (n=11) or horizontal asymmetric (n=3). Flash electroretinograms and flash and pattern visual evoked potentials (VEPs) were recorded in all patients. Eye movement assessment, including horizontal optokinetic nystagmus (OKN) testing, was carried out in 11/14 patients. RESULTS—Eight patients (seven with vertical, one with asymmetric horizontal nystagmus) had congenital cone dysfunction. One patient with vertical and another with asymmetric nystagmus had cone-rod dystrophy. One patient with vertical upbeat had congenital stationary night blindness. Two patients (one downbeat, one upbeat nystagmus) had normal electrophysiological, clinical, and brain magnetic resonance imaging findings and were classified as having CIN. One patient with asymmetric nystagmus showed electrophysiological and clinical findings associated with albinism. Horizontal OKN was present in 80% of patients tested, including the three cases with horizontal asymmetric nystagmus. This is atypical in both CIN and SDN, where the OKN is usually absent. CONCLUSIONS—Vertical and asymmetric nystagmus are most commonly associated with serious intracranial pathology and its presence is an indication for neuroimaging studies. However, such nystagmus can occur in children with retinal disease, albinism, and in cases with CIN. These findings stress the importance of non-invasive VEP/ERG testing in all cases of typical and also atypical nystagmus.
Full Text
The Full Text of this article is available as a PDF (156.0 KB).
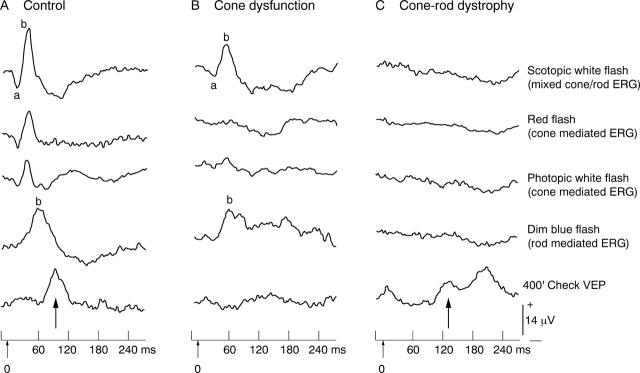
Figure 1 .
Flash ERGs to scotopic bright white (mixed cone and rod mediated response), red, bright white photopic (both cone mediated responses) and dim blue flash (rod mediated response) from a control subject (A), patient no 2 with cone dysfunction (B) and patient no 10 with cone-rod dystrophy (C). Note the prolonged b wave latency of the scotopic white flash ERG in the patient with cone dysfunction (B) relative to control (A) indicating that it is predominantly rod generated, whereas the cone mediated red and photopic white ERGs are absent. The ERGs under all stimulus conditions are not discernible in the patient with cone-rod dystrophy (C). The bottom traces show the occipital pattern VEPs to 400' checks. The arrows show the major positive component (P100). The cone-rod dystrophy patient (C) shows a degraded and prolonged response (up arrow), reflecting poor macular function, whereas the response is barely discernible for the cone dysfunction patient (B).
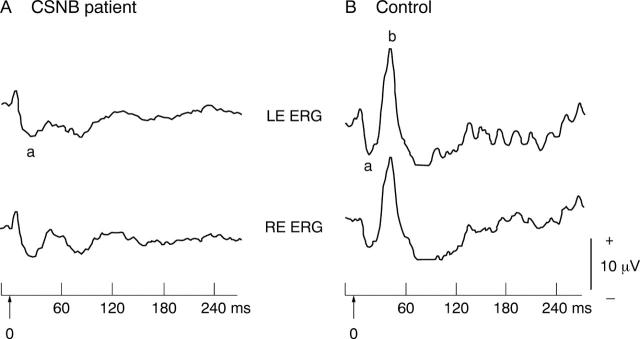
Figure 2 .
Scotopic bright white flash ERGs from patient no 12 with X linked congenital stationary night blindness (CSNB) (A) and age matched control (B). Note the broadened a wave and absent b wave giving the characteristic "negative" ERG configuration in the patient.
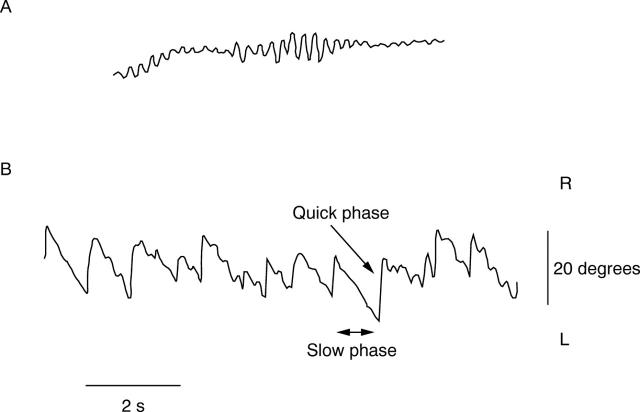
Figure 3 .
Horizontal eye movement waveforms recorded by bitemporal electro-oculography from patient no 10 with cone-rod dystrophy (aged 7 months) who has high frequency, moderately low amplitude horizontal asymmetric nystagmus (A) and preserved horizontal optokinetic response (B). The optokinetic response to full field leftward curtain rotation can be seen with the pendular nystagmus superimposed upon the slow phases. The ERG and VEP results of this patient are shown in Figure 1C.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Abadi R. V., Dickinson C. M. The influence of preexisting oscillations on the binocular optokinetic response. Ann Neurol. 1985 Jun;17(6):578–586. doi: 10.1002/ana.410170609. [DOI] [PubMed] [Google Scholar]
- Baloh R. W., Yee R. D. Spontaneous vertical nystagmus. Rev Neurol (Paris) 1989;145(8-9):527–532. [PubMed] [Google Scholar]
- Berson E. L., Sandberg M. A., Rosner B., Sullivan P. L. Color plates to help identify patients with blue cone monochromatism. Am J Ophthalmol. 1983 Jun;95(6):741–747. doi: 10.1016/0002-9394(83)90058-2. [DOI] [PubMed] [Google Scholar]
- Bixenman W. W. Congenital hereditary downbeat nystagmus. Can J Ophthalmol. 1983 Dec;18(7):344–348. [PubMed] [Google Scholar]
- Casteels I., Harris C. M., Shawkat F., Taylor D. Nystagmus in infancy. Br J Ophthalmol. 1992 Jul;76(7):434–437. doi: 10.1136/bjo.76.7.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FORSYTHE W. I. Congenital hereditary vertical nystagmus. J Neurol Neurosurg Psychiatry. 1955 Aug;18(3):196–198. doi: 10.1136/jnnp.18.3.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fielder A. R., Evans N. M. Is the geniculostriate system a prerequisite for nystagmus? Eye (Lond) 1988;2(Pt 6):628–635. doi: 10.1038/eye.1988.116. [DOI] [PubMed] [Google Scholar]
- Funahashi K., Kuwata T., Yabumoto M., Nakai M., Komai N., Ohmi E. Congenital vertical pendular nystagmus in sisters. Ophthalmologica. 1988;196(3):137–142. doi: 10.1159/000309890. [DOI] [PubMed] [Google Scholar]
- Goldblum T. A., Effron L. A. Upbeat nystagmus associated with tonic downward deviation in healthy neonates. J Pediatr Ophthalmol Strabismus. 1994 Sep-Oct;31(5):334–335. doi: 10.3928/0191-3913-19940901-16. [DOI] [PubMed] [Google Scholar]
- Gottlob I. Eye movement abnormalities in carriers of blue-cone monochromatism. Invest Ophthalmol Vis Sci. 1994 Aug;35(9):3556–3560. [PubMed] [Google Scholar]
- Gottlob I., Reinecke R. D. Eye and head movements in patients with achromatopsia. Graefes Arch Clin Exp Ophthalmol. 1994 Jul;232(7):392–401. doi: 10.1007/BF00186579. [DOI] [PubMed] [Google Scholar]
- Gottlob I., Wizov S. S., Reinecke R. D. Quantitative eye and head movement recordings of retinal disease mimicking spasmus nutans. Am J Ophthalmol. 1995 Mar;119(3):374–376. doi: 10.1016/s0002-9394(14)71188-2. [DOI] [PubMed] [Google Scholar]
- Gottlob I., Zubcov A., Catalano R. A., Reinecke R. D., Koller H. P., Calhoun J. H., Manley D. R. Signs distinguishing spasmus nutans (with and without central nervous system lesions) from infantile nystagmus. Ophthalmology. 1990 Sep;97(9):1166–1175. doi: 10.1016/s0161-6420(90)32440-5. [DOI] [PubMed] [Google Scholar]
- Haegerstrom-Portnoy G., Schneck M. E., Verdon W. A., Hewlett S. E. Clinical vision characteristics of the congenital achromatopsias. II. Color vision. Optom Vis Sci. 1996 Jul;73(7):457–465. doi: 10.1097/00006324-199607000-00002. [DOI] [PubMed] [Google Scholar]
- Harris C. M., Kriss A., Shawkat F., Taylor D. The use of video in assessing and illustrating abnormal eye movements in young children. J Audiov Media Med. 1992 Jul;15(3):113–116. doi: 10.3109/17453059209018364. [DOI] [PubMed] [Google Scholar]
- Hoyt C. S., Gelbart S. S. Vertical nystagmus in infants with congenital ocular abnormalities. Ophthalmic Paediatr Genet. 1984 Dec;4(3):155–161. doi: 10.3109/13816818409006115. [DOI] [PubMed] [Google Scholar]
- Jacobs M., Harris C., Shawkat F., Taylor D. The objective assessment of abnormal eye movements in infants and young children. Aust N Z J Ophthalmol. 1992 Aug;20(3):185–195. doi: 10.1111/j.1442-9071.1992.tb00938.x. [DOI] [PubMed] [Google Scholar]
- Jay W. M., Marcus R. W., Jay M. S. Primary position upbeat nystagmus with organophosphate poisoning. J Pediatr Ophthalmol Strabismus. 1982 Nov-Dec;19(6):318–319. doi: 10.3928/0191-3913-19821101-09. [DOI] [PubMed] [Google Scholar]
- Kattah J. C., Kolsky M. P., Guy J., O'Doherty D. Primary position vertical nystagmus and cerebellar ataxia. Arch Neurol. 1983 May;40(5):310–314. doi: 10.1001/archneur.1983.04050050078012. [DOI] [PubMed] [Google Scholar]
- Kriss A., Russell-Eggitt I. Electrophysiological assessment of visual pathway function in infants. Eye (Lond) 1992;6(Pt 2):145–153. doi: 10.1038/eye.1992.30. [DOI] [PubMed] [Google Scholar]
- Kriss A. Skin ERGs: their effectiveness in paediatric visual assessment, confounding factors, and comparison with ERGs recorded using various types of corneal electrode. Int J Psychophysiol. 1994 May;16(2-3):137–146. doi: 10.1016/0167-8760(89)90040-8. [DOI] [PubMed] [Google Scholar]
- Lambert S. R., Newman N. J. Retinal disease masquerading as spasmus nutans. Neurology. 1993 Aug;43(8):1607–1609. doi: 10.1212/wnl.43.8.1607. [DOI] [PubMed] [Google Scholar]
- Phadke J. G., Hern J. E., Blaiklock C. T. Downbeat nystagmus--a false localising sign due to communicating hydrocephalus. J Neurol Neurosurg Psychiatry. 1981 May;44(5):459–459. doi: 10.1136/jnnp.44.5.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell-Eggitt I., Kriss A., Taylor D. S. Albinism in childhood: a flash VEP and ERG study. Br J Ophthalmol. 1990 Mar;74(3):136–140. doi: 10.1136/bjo.74.3.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SOGG R. L., HOYT W. F. Intermittent vertical nystagmus in a father and son. Arch Ophthalmol. 1962 Oct;68:515–517. doi: 10.1001/archopht.1962.00960030519015. [DOI] [PubMed] [Google Scholar]
- Traccis S., Rosati G., Aiello I., Monaco M. F., Loffredo P., Puliga M. V., Pirastru M. I., Agnetti V. Upbeat nystagmus as an early sign of cerebellar astrocytoma. J Neurol. 1989 Sep;236(6):359–360. doi: 10.1007/BF00314382. [DOI] [PubMed] [Google Scholar]
- Yee R. D. Downbeat nystagmus: characteristics and localization of lesions. Trans Am Ophthalmol Soc. 1989;87:984–1032. [PMC free article] [PubMed] [Google Scholar]
- Yee R. D., Farley M. K., Bateman J. B., Martin D. A. Eye movement abnormalities in rod monochromatism and blue-cone monochromatism. Graefes Arch Clin Exp Ophthalmol. 1985;223(2):55–59. doi: 10.1007/BF02150944. [DOI] [PubMed] [Google Scholar]