Abstract
BACKGROUND/AIM—The pathogenesis of visual field loss associated with macular hole surgery is uncertain but a number of explanations have been proposed, the most convincing of which is the effect of peeling of the posterior hyaloid, causing either direct damage to the nerve fibre layer or to its blood supply at the optic nerve head. The purpose of this preliminary prospective study was to determine the incidence of visual field defects following macular hole surgery in cases in which peeling of the posterior hyaloid was confined only to the area of the macula. METHODS—102 consecutive eyes that had macular hole surgery had preoperative and postoperative visual field examination using a Humphrey's perimeter. A comparison was made between two groups: I, those treated with vitrectomy with complete posterior cortical vitreous peeling; and II, those treated with a vitrectomy with peeling of the posterior hyaloid in the area of the macula but without attempting a complete posterior vitreous detachment. Specifically, no attempt was made to separate the posterior hyaloid from the optic nerve head. Eyes with stage II or III macular holes were operated. Autologous platelet concentrate and non-expansile gas tamponade was used. Patients were postured prone for 1 week. RESULTS—In group I, 22% of patients were found to have visual field defects. In group II, it was possible to separate the posterior hyaloid from the macula without stripping it from the optic nerve head and in these eyes no pattern of postoperative visual field loss emerged. There were no significant vision threatening complications in this group. The difference in the incidence of visual field loss between group I and group II was significant (p=0.02). The anatomical and visual success rates were comparable between both groups. CONCLUSION—The results from this preliminary study suggest that the complication of visual field loss after macular surgery may be reduced if peeling of the posterior hyaloid is confined to the area of the macula so that the hyaloid remains attached at the optic nerve head. The postoperative clinical course does not appear to differ from eyes in which a complete posterior vitreous detachment has been effected during surgery.
Full Text
The Full Text of this article is available as a PDF (131.5 KB).
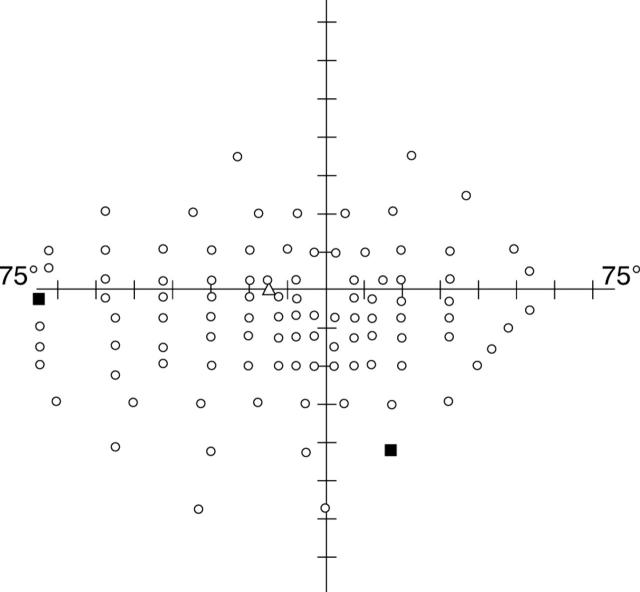
Figure 1 .
An example of a postoperative monocular Humphrey Esterman visual field perimetry from a patient in group II, where the posterior hyaloid remains attached at the optic nerve head.
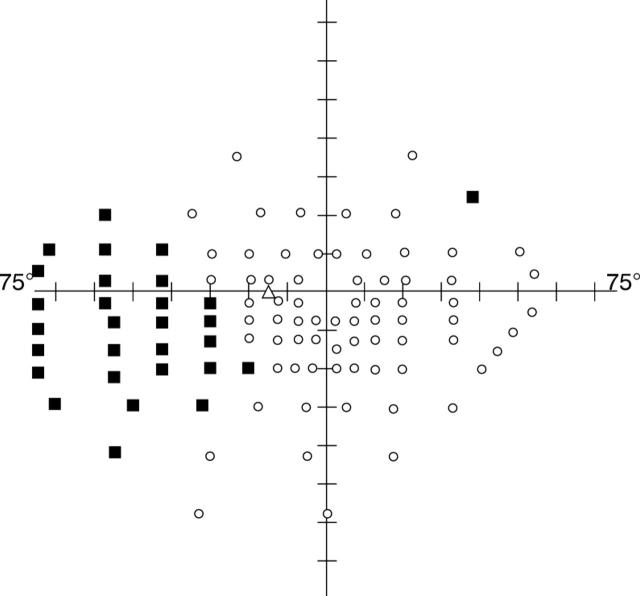
Figure 2 .
Monocular Humphrey Esterman visual field from a patient in group I, following macular hole surgery where the posterior hyaloid was stripped from the optic nerve head. This illustrates the typical inferotemporal quadrant defect found in this group.
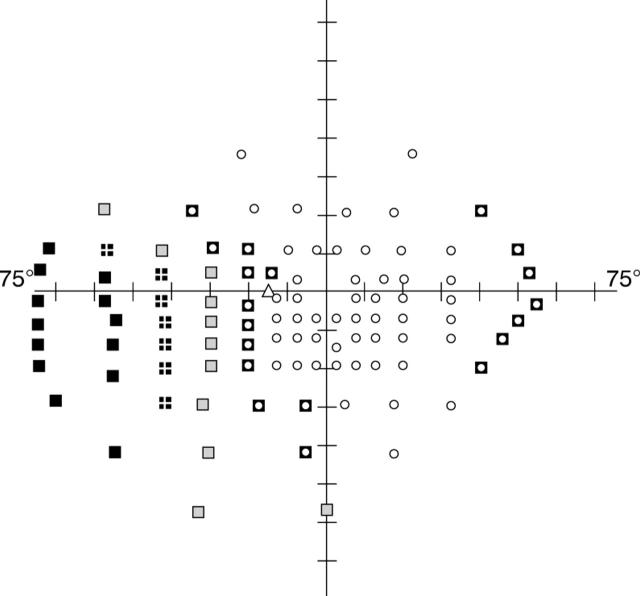
Figure 3 .
Composite pattern of overlapping visual field loss from all 18 patients in whom visual field defects occurred in group I. Black boxes indicate the common points missed by all 18 patients (100%) with field loss. Crossed boxes show points missed in >75% (14-17) of these eyes. Hatched boxes correspond to points missed in >50% (9-13), and centre circle boxes represent the points not seen in < 50% of eyes (<9).
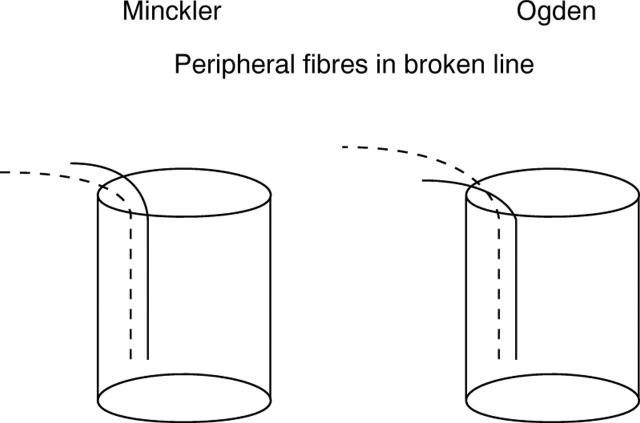
Figure 4 .
A schematic diagram illustrating the proposed theories of vertical topographical organisation of the peripheral retinal nerve fibres at the optic nerve head.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Banker A. S., Freeman W. R., Kim J. W., Munguia D., Azen S. P. Vision-threatening complications of surgery for full-thickness macular holes. Vitrectomy for Macular Hole Study Group. Ophthalmology. 1997 Sep;104(9):1442–1453. doi: 10.1016/s0161-6420(97)30118-3. [DOI] [PubMed] [Google Scholar]
- Berger A. S., Conway M., Del Priore L. V., Walker R. S., Pollack J. S., Kaplan H. J. Submacular surgery for subfoveal choroidal neovascular membranes in patients with presumed ocular histoplasmosis. Arch Ophthalmol. 1997 Aug;115(8):991–996. doi: 10.1001/archopht.1997.01100160161004. [DOI] [PubMed] [Google Scholar]
- Boldt H. C., Munden P. M., Folk J. C., Mehaffey M. G. Visual field defects after macular hole surgery. Am J Ophthalmol. 1996 Sep;122(3):371–381. doi: 10.1016/s0002-9394(14)72064-1. [DOI] [PubMed] [Google Scholar]
- Bopp S., Lucke K., Hille U. Peripheral visual field loss after vitreous surgery for macular holes. Graefes Arch Clin Exp Ophthalmol. 1997 Jun;235(6):362–371. doi: 10.1007/BF00937285. [DOI] [PubMed] [Google Scholar]
- Bouzas E. A., Donati G., Pournaras C. J. Distribution and regulation of the optic nerve head tissue PO2. Surv Ophthalmol. 1997 Nov;42 (Suppl 1):S27–S34. doi: 10.1016/s0039-6257(97)80025-2. [DOI] [PubMed] [Google Scholar]
- Cioffi G. A., Van Buskirk E. M. Microvasculature of the anterior optic nerve. Surv Ophthalmol. 1994 May;38 (Suppl):S107–S117. doi: 10.1016/0039-6257(94)90054-x. [DOI] [PubMed] [Google Scholar]
- Ezra E., Arden G. B., Riordan-Eva P., Aylward G. W., Gregor Z. J. Visual field loss following vitrectomy for stage 2 and 3 macular holes. Br J Ophthalmol. 1996 Jun;80(6):519–525. doi: 10.1136/bjo.80.6.519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foos R. Y. Posterior vitreous detachment. Trans Am Acad Ophthalmol Otolaryngol. 1972 Mar-Apr;76(2):480–497. [PubMed] [Google Scholar]
- Foos R. Y., Roth A. M. Surface structure of the optic nerve head. 2. Vitreopapillary attachments and posterior vitreous detachment. Am J Ophthalmol. 1973 Nov;76(5):662–671. doi: 10.1016/0002-9394(73)90560-6. [DOI] [PubMed] [Google Scholar]
- Gass J. D. Idiopathic senile macular hole. Its early stages and pathogenesis. Arch Ophthalmol. 1988 May;106(5):629–639. doi: 10.1001/archopht.1988.01060130683026. [DOI] [PubMed] [Google Scholar]
- Gass J. D. Reappraisal of biomicroscopic classification of stages of development of a macular hole. Am J Ophthalmol. 1995 Jun;119(6):752–759. doi: 10.1016/s0002-9394(14)72781-3. [DOI] [PubMed] [Google Scholar]
- Gaudric A., Massin P., Paques M., Santiago P. Y., Guez J. E., Le Gargasson J. F., Mundler O., Drouet L. Autologous platelet concentrate for the treatment of full-thickness macular holes. Graefes Arch Clin Exp Ophthalmol. 1995 Sep;233(9):549–554. doi: 10.1007/BF00404704. [DOI] [PubMed] [Google Scholar]
- Groenewald C. P., Wong D., Pearce I., Hiscott P., Grierson I. Nasal epipapillary membrane causing visual field loss following macular hole surgery: does it throw fresh light on the retinotopic arrangement of the nerve fibre layer? Eye (Lond) 1998;12(Pt 2):328–330. doi: 10.1038/eye.1998.80. [DOI] [PubMed] [Google Scholar]
- Hayreh S. S. In vivo choroidal circulation and its watershed zones. Eye (Lond) 1990;4(Pt 2):273–289. doi: 10.1038/eye.1990.39. [DOI] [PubMed] [Google Scholar]
- Hutchins R. K. Complications of macular hole surgery. Ophthalmology. 1998 May;105(5):762–762. doi: 10.1016/S0161-6420(98)95009-6. [DOI] [PubMed] [Google Scholar]
- Hutton W. L., Fuller D. G., Snyder W. B., Fellman R. L., Swanson W. H. Visual field defects after macular hole surgery. A new finding. Ophthalmology. 1996 Dec;103(12):2152–2159. doi: 10.1016/s0161-6420(96)30376-x. [DOI] [PubMed] [Google Scholar]
- Katz B., Hoyt W. F. Intrapapillary and peripapillary hemorrhage in young patients with incomplete posterior vitreous detachment. Signs of vitreopapillary traction. Ophthalmology. 1995 Feb;102(2):349–354. doi: 10.1016/s0161-6420(95)31018-4. [DOI] [PubMed] [Google Scholar]
- Kelly N. E., Wendel R. T. Vitreous surgery for idiopathic macular holes. Results of a pilot study. Arch Ophthalmol. 1991 May;109(5):654–659. doi: 10.1001/archopht.1991.01080050068031. [DOI] [PubMed] [Google Scholar]
- Kerrison J. B., Haller J. A., Elman M., Miller N. R. Visual field loss following vitreous surgery. Arch Ophthalmol. 1996 May;114(5):564–569. doi: 10.1001/archopht.1996.01100130556010. [DOI] [PubMed] [Google Scholar]
- Melberg N. S., Thomas M. A. Visual field loss after pars plana vitrectomy with air/fluid exchange. Am J Ophthalmol. 1995 Sep;120(3):386–388. doi: 10.1016/s0002-9394(14)72169-5. [DOI] [PubMed] [Google Scholar]
- Minckler D. S. The organization of nerve fiber bundles in the primate optic nerve head. Arch Ophthalmol. 1980 Sep;98(9):1630–1636. doi: 10.1001/archopht.1980.01020040482019. [DOI] [PubMed] [Google Scholar]
- Minihan M., Goggin M., Cleary P. E. Surgical management of macular holes: results using gas tamponade alone, or in combination with autologous platelet concentrate, or transforming growth factor beta 2. Br J Ophthalmol. 1997 Dec;81(12):1073–1079. doi: 10.1136/bjo.81.12.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden T. E. Nerve fiber layer of the macaque retina: retinotopic organization. Invest Ophthalmol Vis Sci. 1983 Jan;24(1):85–98. [PubMed] [Google Scholar]
- Paques M., Massin P., Santiago P. Y., Spielmann A. C., Gaudric A. Visual field loss after vitrectomy for full-thickness macular holes. Am J Ophthalmol. 1997 Jul;124(1):88–94. doi: 10.1016/s0002-9394(14)71648-4. [DOI] [PubMed] [Google Scholar]
- Park S. S., Marcus D. M., Duker J. S., Pesavento R. D., Topping T. M., Frederick A. R., Jr, D'Amico D. J. Posterior segment complications after vitrectomy for macular hole. Ophthalmology. 1995 May;102(5):775–781. doi: 10.1016/s0161-6420(95)30956-6. [DOI] [PubMed] [Google Scholar]
- Pendergast S. D., McCuen B. W., 2nd Visual field loss after macular hole surgery. Ophthalmology. 1996 Jul;103(7):1069–1077. doi: 10.1016/s0161-6420(96)30565-4. [DOI] [PubMed] [Google Scholar]
- Roth A. M., Foos R. Y. Surface structure of the optic nerve head. 1. Epipapillary membranes. Am J Ophthalmol. 1972 Nov;74(5):977–985. doi: 10.1016/0002-9394(72)91221-4. [DOI] [PubMed] [Google Scholar]
- Welch J. C. Dehydration injury as a possible cause of visual field defect after pars plana vitrectomy for macular hole. Am J Ophthalmol. 1997 Nov;124(5):698–699. doi: 10.1016/s0002-9394(14)70915-8. [DOI] [PubMed] [Google Scholar]