Abstract
AIM—To classify ocular adnexal lymphomas according to the Revised European and American Lymphoma (REAL) classification and to determine any correlation between clinical features or histomorphological variables with the patients' outcome. METHODS—Conventional and immunohistology were performed on representative sections of 53 specimens of 46 patients with ocular adnexal lymphoma. The antibodies used were CD20, BCL-2, CD21, CD23, CD43, CD3, CD5, p53, cyclin D1, pan-cytokeratin, kappa, lambda, IgD, and IgM. The growth fraction of the tumours was determined using the MIB-1 antibody directed against the Ki-67 antigen. Clinical follow up data regarding the outcome were obtained from the treating physicians and/or hospital files. The Student's t test and log rank test were used for statistical analysis. RESULTS—The patient collective consisted of 29 females and 17 males with an age range of 32-89.7 years (average 63 years). Almost all specimens represented B cell non-Hodgkin's lymphomas: extranodal marginal zone lymphoma (EMZL) (n=38), diffuse large cell B cell lymphoma (n=8), lymphoplasmocytic lymphoma/immunocytoma (n=2), mantle cell lymphoma (n=2), follicle centre lymphoma (n=1), and plasmacytoma (n=1). One case of a secondary anaplastic large cell lymphoma of T cell type (T-ALCL) was diagnosed. The majority of the patients had stage I disease. A variety of therapeutic regimens was administered, the main form of treatment being radiotherapy. The average follow up time was 85 months. Complete remission was achieved in 24 patients (10 after excision alone, eight after radiotherapy alone, three after combined excision and radiotherapy, one after chemotherapy alone, and two after combined radiotherapy and chemotherapy). 12 patients died of causes related to lymphoma; in one patient the cause of death was unknown. Six patients had persistent tumour at final follow up and two patients were lost to follow up. The stage at presentation, as well as the lymphoma malignancy category, had a significant correlation with the final course of the disease (p=0.0001 and p=0.03, respectively). A significant correlation was also noted between the final outcome (p<0.05) and tumour cell expression for Ki-67 antigen and p53 protein. CONCLUSION—67% of patients with ocular adnexal lymphoma had EMZL. The stage at presentation had a significant influence on the final outcome. MIB-1 and p53 expression by the tumour cells proved to be important immunohistochemical markers concerning the prognosis. It is suggested that, following thorough staging investigations, primary EMZL (stage I) (if accessible) should be treated with excisional biopsy and subsequent low dose radiotherapy. Primary diffuse large cell B cell lymphoma of the ocular adnexa requires at least similar therapeutic measures and regular intensive follow up.
Full Text
The Full Text of this article is available as a PDF (218.8 KB).
Figure 1 .
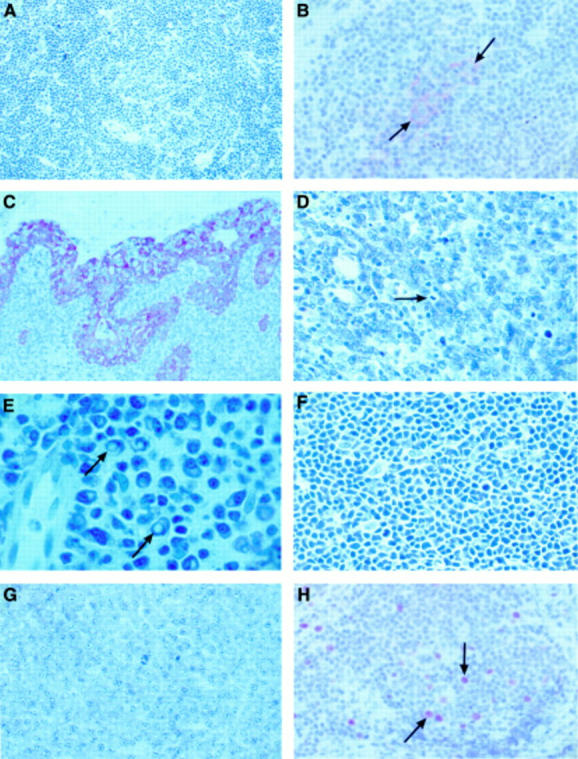
(A) Extranodal marginal zone lymphoma with a broadened marginal zone and infiltration of a reactive follicle with small centrocytoid tumour cells (Giemsa, ×200). (B) Remainders of a reactive follicle staining positively with CD23 (follicle dendritic cells, arrows), surrounded by infiltrating small centrocytoid lymphoma cells (×400). (C) Lymphoepithelial lesions, the epithelial cells stained positively with antibodies for pancytokeratin (×200). (D) Diffuse large cell B cell lymphoma showing a diffuse proliferation of lymphoblasts and a mitosis (arrow) (Giemsa, ×400). (E) Lymphoplasmacytic lymphoma/immunocytoma with Dutcher bodies (arrows) (Giemsa, ×1000). (F) Mantle cell lymphoma with tumour cells of intermediate size without blasts and with intermingled pale staining dendritic cells (Giemsa, ×400). (G) Localised plasmacytoma of the sclera (Giemsa, ×400). (H) Extranodal marginal zone lymphoma with a Ki-67 antigen positivity of 10% (×400, arrows: positive stained nuclei of lymphoma cells).
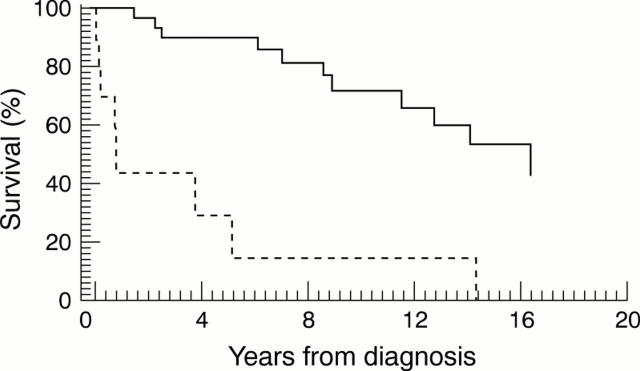
Figure 2 .
Kaplan-Meier curve. Stage of disease at time of presentation related to the survival (solid line, stage I; broken line, stage II-IV; log rank test: p=0.0001).
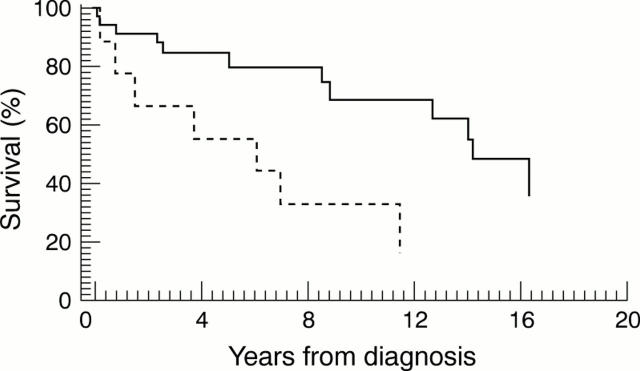
Figure 3 .
Kaplan-Meier curve. Lymphoma category of malignancy related to survival (solid line, low grade; broken line, high grade; log rank test: p=0.03).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baldini L., Blini M., Guffanti A., Fossati V., Colombi M., La Targia M. L., Bertoni F., Alietti A., Neri A., Bertoni G. Treatment and prognosis in a series of primary extranodal lymphomas of the ocular adnexa. Ann Oncol. 1998 Jul;9(7):779–781. doi: 10.1023/a:1008327301372. [DOI] [PubMed] [Google Scholar]
- Cahill M., Barnes C., Moriarty P., Daly P., Kennedy S. Ocular adnexal lymphoma-comparison of MALT lymphoma with other histological types. Br J Ophthalmol. 1999 Jun;83(6):742–747. doi: 10.1136/bjo.83.6.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cordell J. L., Falini B., Erber W. N., Ghosh A. K., Abdulaziz Z., MacDonald S., Pulford K. A., Stein H., Mason D. Y. Immunoenzymatic labeling of monoclonal antibodies using immune complexes of alkaline phosphatase and monoclonal anti-alkaline phosphatase (APAAP complexes). J Histochem Cytochem. 1984 Feb;32(2):219–229. doi: 10.1177/32.2.6198355. [DOI] [PubMed] [Google Scholar]
- Coupland S. E., Foss H. D., Assaf C., Auw-Haedrich C., Anastassiou G., Anagnostopoulos I., Hummel M., Karesh J. W., Lee W. R., Stein H. T-cell and T/natural killer-cell lymphomas involving ocular and ocular adnexal tissues: a clinicopathologic, immunohistochemical, and molecular study of seven cases. Ophthalmology. 1999 Nov;106(11):2109–2120. doi: 10.1016/S0161-6420(99)90492-X. [DOI] [PubMed] [Google Scholar]
- Coupland S. E., Krause L., Delecluse H. J., Anagnostopoulos I., Foss H. D., Hummel M., Bornfeld N., Lee W. R., Stein H. Lymphoproliferative lesions of the ocular adnexa. Analysis of 112 cases. Ophthalmology. 1998 Aug;105(8):1430–1441. doi: 10.1016/S0161-6420(98)98024-1. [DOI] [PubMed] [Google Scholar]
- Ellis J. H., Banks P. M., Campbell R. J., Liesegang T. J. Lymphoid tumors of the ocular adnexa. Clinical correlation with the working formulation classification and immunoperoxidase staining of paraffin sections. Ophthalmology. 1985 Oct;92(10):1311–1324. [PubMed] [Google Scholar]
- Ferry J. A., Yang W. I., Zukerberg L. R., Wotherspoon A. C., Arnold A., Harris N. L. CD5+ extranodal marginal zone B-cell (MALT) lymphoma. A low grade neoplasm with a propensity for bone marrow involvement and relapse. Am J Clin Pathol. 1996 Jan;105(1):31–37. doi: 10.1093/ajcp/105.1.31. [DOI] [PubMed] [Google Scholar]
- Isaacson P., Wright D. H. Extranodal malignant lymphoma arising from mucosa-associated lymphoid tissue. Cancer. 1984 Jun 1;53(11):2515–2524. doi: 10.1002/1097-0142(19840601)53:11<2515::aid-cncr2820531125>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- Jakobiec F. A., Knowles D. M. An overview of ocular adnexal lymphoid tumors. Trans Am Ophthalmol Soc. 1989;87:420–444. [PMC free article] [PubMed] [Google Scholar]
- Jakobiec F. A., McLean I., Font R. L. Clinicopathologic characteristics of orbital lymphoid hyperplasia. Ophthalmology. 1979 May;86(5):948–966. doi: 10.1016/s0161-6420(79)35438-0. [DOI] [PubMed] [Google Scholar]
- Knowles D. M., 2nd, Jakobiec F. A. Orbital lymphoid neoplasms: a clinicopathologic study of 60 patients. Cancer. 1980 Aug 1;46(3):576–589. doi: 10.1002/1097-0142(19800801)46:3<576::aid-cncr2820460326>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- Knowles D. M., Jakobiec F. A., McNally L., Burke J. S. Lymphoid hyperplasia and malignant lymphoma occurring in the ocular adnexa (orbit, conjunctiva, and eyelids): a prospective multiparametric analysis of 108 cases during 1977 to 1987. Hum Pathol. 1990 Sep;21(9):959–973. doi: 10.1016/0046-8177(90)90181-4. [DOI] [PubMed] [Google Scholar]
- Liesegang T. J. Ocular adnexal lymphoproliferative lesions. Mayo Clin Proc. 1993 Oct;68(10):1003–1010. doi: 10.1016/s0025-6196(12)62275-7. [DOI] [PubMed] [Google Scholar]
- Medeiros L. J., Harmon D. C., Linggood R. M., Harris N. L. Immunohistologic features predict clinical behavior of orbital and conjunctival lymphoid infiltrates. Blood. 1989 Nov 1;74(6):2121–2129. [PubMed] [Google Scholar]
- National Cancer Institute sponsored study of classifications of non-Hodgkin's lymphomas: summary and description of a working formulation for clinical usage. The Non-Hodgkin's Lymphoma Pathologic Classification Project. Cancer. 1982 May 15;49(10):2112–2135. doi: 10.1002/1097-0142(19820515)49:10<2112::aid-cncr2820491024>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- Norton A. J., Jordan S., Yeomans P. Brief, high-temperature heat denaturation (pressure cooking): a simple and effective method of antigen retrieval for routinely processed tissues. J Pathol. 1994 Aug;173(4):371–379. doi: 10.1002/path.1711730413. [DOI] [PubMed] [Google Scholar]
- Petrella T., Bron A., Foulet A., Arnould L., Chirpaz L., Michiels R. Report of a primary lymphoma of the conjunctiva. A lymphoma of MALT origin? Pathol Res Pract. 1991 Jan;187(1):78–84. doi: 10.1016/S0344-0338(11)81049-6. [DOI] [PubMed] [Google Scholar]
- Smithers D. W. Summary of papers delivered at the Conference on Staging in Hodgkin's Disease (Ann Arbor). Cancer Res. 1971 Nov;31(11):1869–1870. [PubMed] [Google Scholar]
- Vogiatzis K. V. Lymphoid tumors of the orbit and ocular adnexa: a long-term follow-up. Ann Ophthalmol. 1984 Nov;16(11):1046–1055. [PubMed] [Google Scholar]
- White W. L., Ferry J. A., Harris N. L., Grove A. S., Jr Ocular adnexal lymphoma. A clinicopathologic study with identification of lymphomas of mucosa-associated lymphoid tissue type. Ophthalmology. 1995 Dec;102(12):1994–2006. doi: 10.1016/s0161-6420(95)30764-6. [DOI] [PubMed] [Google Scholar]