Abstract
AIMS—To determine if postoperative visual outcome after successful macular hole surgery can be predicted with preoperative scanning laser ophthalmoscope (SLO) microperimetry. METHODS—A prospective non-comparative study of 16 eyes in 15 patients examined before the surgery. RESULTS—Visual outcome following macular hole surgery correlated with the "maximum parahole sensitivity", the highest intensity of stimulus to which the patient did not respond to any of the stimuli around the hole. Preoperative visual acuity, duration of the symptoms, size of the macular hole, and the "minimum parahole sensitivity", the lowest intensity to which the patient responded to all the stimuli around the hole, did not correlate significantly with postoperative visual acuity. CONCLUSION—Preoperative assessment of patients using SLO microperimetry is a good predictor of visual outcome after macular hole surgery.
Full Text
The Full Text of this article is available as a PDF (101.1 KB).
Figure 1 .
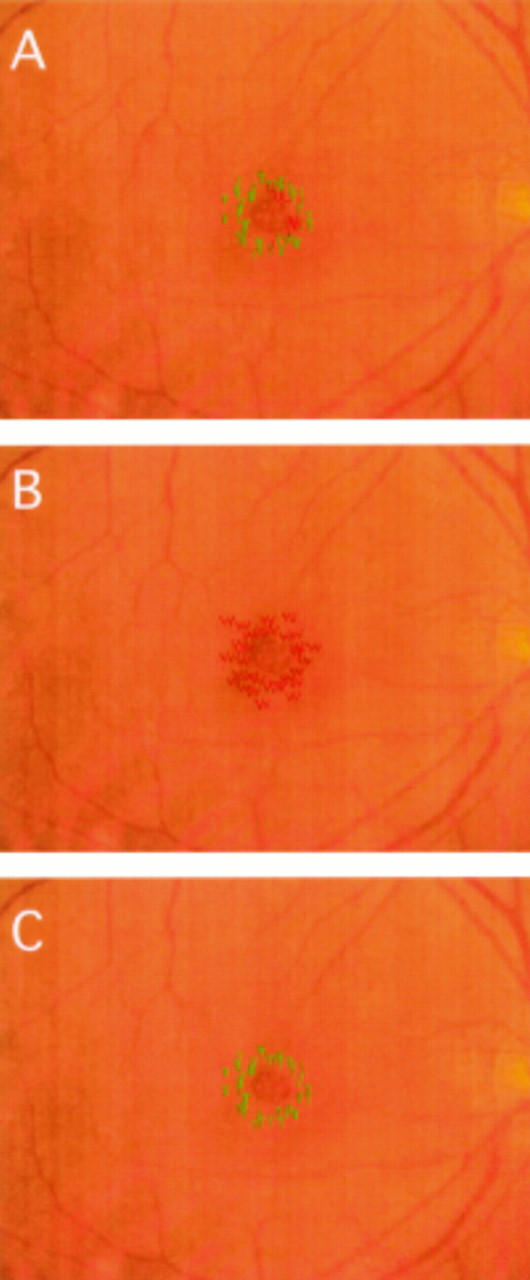
The actual procedure of SLO microperimetry to evaluate macular holes. (A) When the stimuli were presented at 20 dB, two different coloured spots that the patient recognised (green) and did not recognise (red) are shown. (B) The intensity was decreased until the patient did not recognise all stimuli around the macular hole, which was defined as the "maximum parahole sensitivity" (22 dB). (C) Thereafter, intensity was increased until the patient recognised all stimuli around the macular hole, which was defined as the "minimum parahole sensitivity" (17 dB).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Byhr E., Lindblom B. Preoperative measurements of macular hole with scanning laser ophthalmoscopy. Correlation with functional outcome. Acta Ophthalmol Scand. 1998 Oct;76(5):579–583. doi: 10.1034/j.1600-0420.1998.760513.x. [DOI] [PubMed] [Google Scholar]
- Freeman W. R., Azen S. P., Kim J. W., el-Haig W., Mishell D. R., 3rd, Bailey I. Vitrectomy for the treatment of full-thickness stage 3 or 4 macular holes. Results of a multicentered randomized clinical trial. The Vitrectomy for Treatment of Macular Hole Study Group. Arch Ophthalmol. 1997 Jan;115(1):11–21. doi: 10.1001/archopht.1997.01100150013002. [DOI] [PubMed] [Google Scholar]
- Funata M., Wendel R. T., de la Cruz Z., Green W. R. Clinicopathologic study of bilateral macular holes treated with pars plana vitrectomy and gas tamponade. Retina. 1992;12(4):289–298. doi: 10.1097/00006982-199212040-00001. [DOI] [PubMed] [Google Scholar]
- Glaser B. M., Michels R. G., Kuppermann B. D., Sjaarda R. N., Pena R. A. Transforming growth factor-beta 2 for the treatment of full-thickness macular holes. A prospective randomized study. Ophthalmology. 1992 Jul;99(7):1162–1173. doi: 10.1016/s0161-6420(92)31837-8. [DOI] [PubMed] [Google Scholar]
- Hee M. R., Puliafito C. A., Wong C., Duker J. S., Reichel E., Schuman J. S., Swanson E. A., Fujimoto J. G. Optical coherence tomography of macular holes. Ophthalmology. 1995 May;102(5):748–756. doi: 10.1016/s0161-6420(95)30959-1. [DOI] [PubMed] [Google Scholar]
- Kelly N. E., Wendel R. T. Vitreous surgery for idiopathic macular holes. Results of a pilot study. Arch Ophthalmol. 1991 May;109(5):654–659. doi: 10.1001/archopht.1991.01080050068031. [DOI] [PubMed] [Google Scholar]
- Lansing M. B., Glaser B. M., Liss H., Hanham A., Thompson J. T., Sjaarda R. N., Gordon A. J. The effect of pars plana vitrectomy and transforming growth factor-beta 2 without epiretinal membrane peeling on full-thickness macular holes. Ophthalmology. 1993 Jun;100(6):868–872. doi: 10.1016/s0161-6420(93)31561-7. [DOI] [PubMed] [Google Scholar]
- Madreperla S. A., Geiger G. L., Funata M., de la Cruz Z., Green W. R. Clinicopathologic correlation of a macular hole treated by cortical vitreous peeling and gas tamponade. Ophthalmology. 1994 Apr;101(4):682–686. doi: 10.1016/s0161-6420(94)31278-4. [DOI] [PubMed] [Google Scholar]
- Orellana J., Lieberman R. M. Stage III macular hole surgery. Br J Ophthalmol. 1993 Sep;77(9):555–558. doi: 10.1136/bjo.77.9.555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smiddy W. E., Thomley M. L., Knighton R. W., Feuer W. J. Use of the potential acuity meter and laser interferometer to predict visual acuity after macular hole surgery. Retina. 1994;14(4):305–309. doi: 10.1097/00006982-199414040-00003. [DOI] [PubMed] [Google Scholar]
- Weingeist T. A. Surgical management of idiopathic macular holes. Ophthalmology. 1993 Nov;100(11):1607–1608. doi: 10.1016/s0161-6420(93)31430-2. [DOI] [PubMed] [Google Scholar]


