Full Text
The Full Text of this article is available as a PDF (235.1 KB).
Figure 1 .
Grade 1 ocular surface burn. Large corneal burn following accidental exposure to ammonia. There is no limbal or conjunctival involvement. Fluorescein stained diffuse view of the cornea.
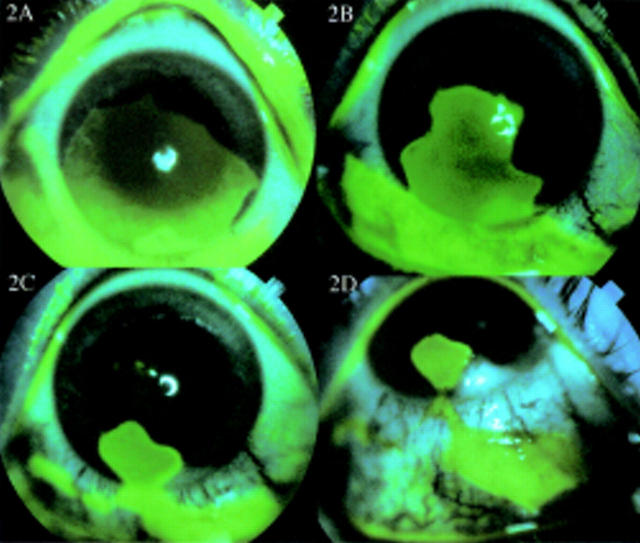
Figure 2 .
(A) Grade 3 (4.5/30%) ocular surface burn. Four and a half clock hours of limbus involvement with 30% conjunctival involvement following ocular surface burn with a domestic cleansing (alkali) injury. (B) and (C) the surviving limbal epithelium demonstrates circumferential migration of tongue-shaped projections affording limbal epithelial cover to denuded limbus. (D) The entire limbus has healed with limbal epithelium and the corneal surface too is almost completely healed with corneal (limbal derived) epithelium. The conjunctival defect is closing with conjunctival epithelium. Fluorescein stained diffuse view of the cornea.
Figure 3 .

Grade 3 (5/35%) ocular surface burn following an accident involving an industrial alkaline chemical. Five clock hours of the limbus and 35% of the conjunctiva were involved. (A) Diffuse view with patient looking straight illustrating the extent of limbal involvement. (B) Diffuse view with patient looking up and out and (C) looking up and in to show the extent of conjunctival involvement. (With the Roper Hall grading (III) this would carry a guarded prognosis. This patient made a complete recovery.)
Figure 4 .

Grade 4 (7/50%) ocular surface burn following an acid burn. Seven clock hours of the limbus and 50% of the conjunctiva were involved. (A) An autolimbal transplant was first carried out in the inferior nasal quadrant (arrows). (B) One year after a full thickness corneal transplant that succeeded the autolimbal transplant by 4 months. Arrows show the limits of the autologous conjunctiva attached to the peripheral corneal strip that constituted the "autolimbal graft." The patient has been followed for 2.5 years and retains a clear graft. (With the Roper Hall grading (IV) this would carry a poor prognosis.)
Figure 5 .

Grade 5 (9.5/60%) ocular surface burn following alkali injury. Nine and a half clock hours of the limbus and 60% of the conjunctiva were involved. (A) Diffuse view of the cornea showing extensive conjunctivalisation and a fibrovascular pannus. (B) The eye 13 months after ocular surface reconstruction with autolimbal transplantation. (With the Roper Hall grading (IV) this would carry a poor prognosis.)
Figure 6 .

Grade 6 (12/100%) ocular surface burn with a "fish pond cleaning liquid" following an assault. The entire limbus and the entire conjunctiva were involved. (A) Diffuse view showing involvement of the entire upper and (B) lower bulbar conjunctiva. (C) The entire corneal surface and 12 clock hours of the limbus are involved. This patient carries a very poor prognosis.
Figure 7 .
Grade 6 (12/100%) ocular surface burn following injury with cement powder. The entire limbus and conjunctiva were involved. This picture was taken 7 months after the injury. The eye is becoming pthysical with extensive symblepharon. This illustrates the very poor prognosis of a grade 6 burn. (With the Roper Hall grading Figs 4, 5, 6, and 7 would all be grouped under grade IV with a poor prognosis.)
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Azuara-Blanco A., Pillai C. T., Dua H. S. Amniotic membrane transplantation for ocular surface reconstruction. Br J Ophthalmol. 1999 Apr;83(4):399–402. doi: 10.1136/bjo.83.4.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodovsky S. C., McCarty C. A., Snibson G., Loughnan M., Sullivan L., Daniell M., Taylor H. R. Management of alkali burns : an 11-year retrospective review. Ophthalmology. 2000 Oct;107(10):1829–1835. doi: 10.1016/s0161-6420(00)00289-x. [DOI] [PubMed] [Google Scholar]
- Chen J. J., Tseng S. C. Abnormal corneal epithelial wound healing in partial-thickness removal of limbal epithelium. Invest Ophthalmol Vis Sci. 1991 Jul;32(8):2219–2233. [PubMed] [Google Scholar]
- Chen J. J., Tseng S. C. Corneal epithelial wound healing in partial limbal deficiency. Invest Ophthalmol Vis Sci. 1990 Jul;31(7):1301–1314. [PubMed] [Google Scholar]
- Davanger M., Evensen A. Role of the pericorneal papillary structure in renewal of corneal epithelium. Nature. 1971 Feb 19;229(5286):560–561. doi: 10.1038/229560a0. [DOI] [PubMed] [Google Scholar]
- Dua H. S., Azuara-Blanco A. Allo-limbal transplantation in patients with limbal stem cell deficiency. Br J Ophthalmol. 1999 Apr;83(4):414–419. doi: 10.1136/bjo.83.4.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dua H. S., Azuara-Blanco A. Autologous limbal transplantation in patients with unilateral corneal stem cell deficiency. Br J Ophthalmol. 2000 Mar;84(3):273–278. doi: 10.1136/bjo.84.3.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dua H. S., Azuara-Blanco A. Limbal stem cells of the corneal epithelium. Surv Ophthalmol. 2000 Mar-Apr;44(5):415–425. doi: 10.1016/s0039-6257(00)00109-0. [DOI] [PubMed] [Google Scholar]
- Dua H. S., Forrester J. V. Clinical patterns of corneal epithelial wound healing. Am J Ophthalmol. 1987 Nov 15;104(5):481–489. doi: 10.1016/s0002-9394(14)74105-4. [DOI] [PubMed] [Google Scholar]
- Dua H. S., Forrester J. V. The corneoscleral limbus in human corneal epithelial wound healing. Am J Ophthalmol. 1990 Dec 15;110(6):646–656. doi: 10.1016/s0002-9394(14)77062-x. [DOI] [PubMed] [Google Scholar]
- Dua H. S. Stem cells of the ocular surface: scientific principles and clinical applications. Br J Ophthalmol. 1995 Nov;79(11):968–969. doi: 10.1136/bjo.79.11.968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dua H. S. The conjunctiva in corneal epithelial wound healing. Br J Ophthalmol. 1998 Dec;82(12):1407–1411. doi: 10.1136/bjo.82.12.1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang A. J., Tseng S. C. Corneal epithelial wound healing in the absence of limbal epithelium. Invest Ophthalmol Vis Sci. 1991 Jan;32(1):96–105. [PubMed] [Google Scholar]
- Kenyon K. R., Tseng S. C. Limbal autograft transplantation for ocular surface disorders. Ophthalmology. 1989 May;96(5):709–723. doi: 10.1016/s0161-6420(89)32833-8. [DOI] [PubMed] [Google Scholar]
- Kinoshita S., Kiorpes T. C., Friend J., Thoft R. A. Limbal epithelium in ocular surface wound healing. Invest Ophthalmol Vis Sci. 1982 Jul;23(1):73–80. [PubMed] [Google Scholar]
- Kruse F. E. Stem cells and corneal epithelial regeneration. Eye (Lond) 1994;8(Pt 2):170–183. doi: 10.1038/eye.1994.42. [DOI] [PubMed] [Google Scholar]
- Meller D., Pires R. T., Mack R. J., Figueiredo F., Heiligenhaus A., Park W. C., Prabhasawat P., John T., McLeod S. D., Steuhl K. P. Amniotic membrane transplantation for acute chemical or thermal burns. Ophthalmology. 2000 May;107(5):980–990. doi: 10.1016/s0161-6420(00)00024-5. [DOI] [PubMed] [Google Scholar]
- Morgan S., Murray A. Limbal autotransplantation in the acute and chronic phases of severe chemical injuries. Eye (Lond) 1996;10(Pt 3):349–354. doi: 10.1038/eye.1996.72. [DOI] [PubMed] [Google Scholar]
- Pfister R. R. Chemical injuries of the eye. Ophthalmology. 1983 Oct;90(10):1246–1253. [PubMed] [Google Scholar]
- Roper-Hall M. J. Thermal and chemical burns. Trans Ophthalmol Soc U K. 1965;85:631–653. [PubMed] [Google Scholar]
- Shimazaki J., Yang H. Y., Tsubota K. Amniotic membrane transplantation for ocular surface reconstruction in patients with chemical and thermal burns. Ophthalmology. 1997 Dec;104(12):2068–2076. doi: 10.1016/s0161-6420(97)30057-8. [DOI] [PubMed] [Google Scholar]
- Sridhar M. S., Bansal A. K., Sangwan V. S., Rao G. N. Amniotic membrane transplantation in acute chemical and thermal injury. Am J Ophthalmol. 2000 Jul;130(1):134–137. doi: 10.1016/s0002-9394(00)00500-6. [DOI] [PubMed] [Google Scholar]
- Townsend W. M. The limbal palisades of Vogt. Trans Am Ophthalmol Soc. 1991;89:721–756. [PMC free article] [PubMed] [Google Scholar]
- Tsai R. J., Li L. M., Chen J. K. Reconstruction of damaged corneas by transplantation of autologous limbal epithelial cells. N Engl J Med. 2000 Jul 13;343(2):86–93. doi: 10.1056/NEJM200007133430202. [DOI] [PubMed] [Google Scholar]
- Tsai R. J., Tseng S. C. Human allograft limbal transplantation for corneal surface reconstruction. Cornea. 1994 Sep;13(5):389–400. doi: 10.1097/00003226-199409000-00003. [DOI] [PubMed] [Google Scholar]
- Tseng S. C., Prabhasawat P., Barton K., Gray T., Meller D. Amniotic membrane transplantation with or without limbal allografts for corneal surface reconstruction in patients with limbal stem cell deficiency. Arch Ophthalmol. 1998 Apr;116(4):431–441. doi: 10.1001/archopht.116.4.431. [DOI] [PubMed] [Google Scholar]
- Tseng S. C., Prabhasawat P., Lee S. H. Amniotic membrane transplantation for conjunctival surface reconstruction. Am J Ophthalmol. 1997 Dec;124(6):765–774. doi: 10.1016/s0002-9394(14)71693-9. [DOI] [PubMed] [Google Scholar]
- Tsubota K., Toda I., Saito H., Shinozaki N., Shimazaki J. Reconstruction of the corneal epithelium by limbal allograft transplantation for severe ocular surface disorders. Ophthalmology. 1995 Oct;102(10):1486–1496. doi: 10.1016/s0161-6420(95)30841-x. [DOI] [PubMed] [Google Scholar]
- Wei Z. G., Wu R. L., Lavker R. M., Sun T. T. In vitro growth and differentiation of rabbit bulbar, fornix, and palpebral conjunctival epithelia. Implications on conjunctival epithelial transdifferentiation and stem cells. Invest Ophthalmol Vis Sci. 1993 Apr;34(5):1814–1828. [PubMed] [Google Scholar]