Abstract
BACKGROUND/AIMS—Previous studies reported the predictive value of the short wavelength sensitive (SWS) cone mediated sensitivity for visual outcome in age related macular degeneration. In this study SWS sensitivity was measured by commercially available blue on yellow perimetry in patients with non-exudative age related maculopathy (ARM) and compared with the presence of morphological risk factors and the status of the fellow eye. METHODS—In a prospective cross sectional study, 126 patients (57 males, 69 females, mean age 71 (SD 6) years) with ARM (visual acuity >20/50) were tested. Central visual fields (blue on yellow) were obtained with a conventional perimeter. Fundus slides were graded by two independent observers for soft drusen and presence of focal hyperpigmentation. RESULTS—Mean sensitivity and standard deviation of all patients exhibited a significant reduction with age. Patients with soft drusen had significantly lower sensitivity than those without, whereas there were no differences in visual acuity (log MAR). Sensitivity was also reduced in those eyes with fellow eyes having a sight threatening complication of age related macular degeneration (AMD). Eyes with focal hyperpigmentation compared with those without had no loss of sensitivity, but did have a significant decrease in the central part of the field compared with the more eccentric. CONCLUSION—SWS sensitivity loss is associated with common risk factors for progression to AMD. Short wavelength automated perimetry is moderately rapid and readily available. It may serve as a tool in future ARM trials.
Full Text
The Full Text of this article is available as a PDF (157.3 KB).
Figure 1 .
Perimetry results (in dB) for all 68 stimulus locations superimposed on the matching fundus photograph. A 68 year old male patient with normal visual acuity and soft drusen.
Figure 2 .
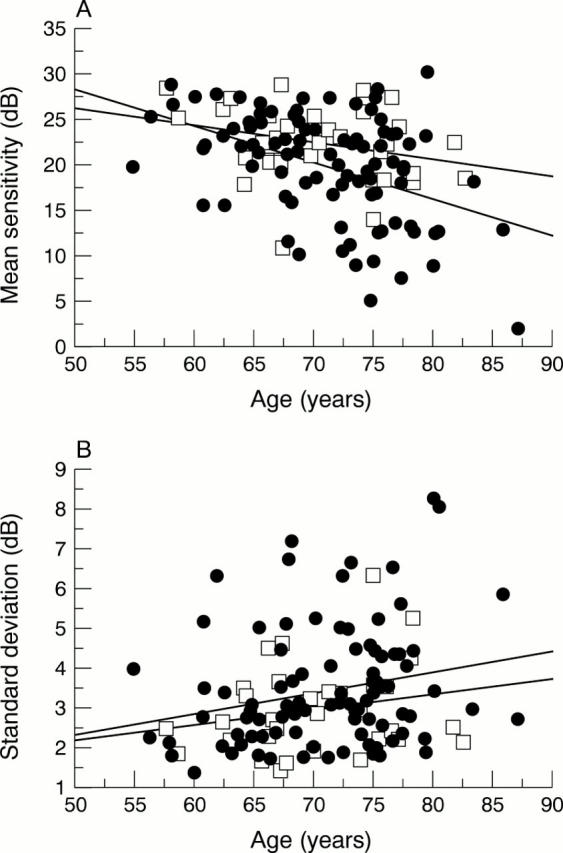
(A) Mean sensitivity of the included patients as a function of age (mean sensitivity = 45.77-0.357 * age; r = −0.41); closed circles: eyes with soft drusen (mean sensitivity = 48.41-0.403 * age; r = −0.45), open squares: eyes without soft drusen (mean sensitivity = 35.67 −0.190 * age; r = −0.29). (B) Standard deviation (SD) over the full 10 deg field of the included patients as a function of age (SD = −0.283 + 0.051 * age; r =0.23); closed circles: eyes with soft drusen (SD = −0.335 + 0.053 * age; r = 0.23), open squares: eyes without soft drusen (SD = 0.273 + 0.039 * age; r = 0.22).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bressler N. M., Bressler S. B., Seddon J. M., Gragoudas E. S., Jacobson L. P. Drusen characteristics in patients with exudative versus non-exudative age-related macular degeneration. Retina. 1988;8(2):109–114. doi: 10.1097/00006982-198808020-00005. [DOI] [PubMed] [Google Scholar]
- Brown B., Adams A. J., Coletta N. J., Haegerstrom-Portnoy G. Dark adaptation in age-related maculopathy. Ophthalmic Physiol Opt. 1986;6(1):81–84. [PubMed] [Google Scholar]
- Eisner A., Fleming S. A., Klein M. L., Mauldin W. M. Sensitivities in older eyes with good acuity: eyes whose fellow eye has exudative AMD. Invest Ophthalmol Vis Sci. 1987 Nov;28(11):1832–1837. [PubMed] [Google Scholar]
- Eisner A., Klein M. L., Zilis J. D., Watkins M. D. Visual function and the subsequent development of exudative age-related macular degeneration. Invest Ophthalmol Vis Sci. 1992 Oct;33(11):3091–3102. [PubMed] [Google Scholar]
- Eisner A., Stoumbos V. D., Klein M. L., Fleming S. A. Relations between fundus appearance and function. Eyes whose fellow eye has exudative age-related macular degeneration. Invest Ophthalmol Vis Sci. 1991 Jan;32(1):8–20. [PubMed] [Google Scholar]
- Greenstein V. C., Hood D. C., Ritch R., Steinberger D., Carr R. E. S (blue) cone pathway vulnerability in retinitis pigmentosa, diabetes and glaucoma. Invest Ophthalmol Vis Sci. 1989 Aug;30(8):1732–1737. [PubMed] [Google Scholar]
- Holz F. G., Gross-Jendroska M., Eckstein A., Hogg C. R., Arden G. B., Bird A. C. Colour contrast sensitivity in patients with age-related Bruch's membrane changes. Ger J Ophthalmol. 1995 Nov;4(6):336–341. [PubMed] [Google Scholar]
- Hudson C., Flanagan J. G., Turner G. S., Chen H. C., Young L. B., McLeod D. Short-wavelength sensitive visual field loss in patients with clinically significant diabetic macular oedema. Diabetologia. 1998 Aug;41(8):918–928. doi: 10.1007/s001250051008. [DOI] [PubMed] [Google Scholar]
- Johnson C. A., Adams A. J., Casson E. J., Brandt J. D. Blue-on-yellow perimetry can predict the development of glaucomatous visual field loss. Arch Ophthalmol. 1993 May;111(5):645–650. doi: 10.1001/archopht.1993.01090050079034. [DOI] [PubMed] [Google Scholar]
- Johnson C. A., Adams A. J., Casson E. J., Brandt J. D. Progression of early glaucomatous visual field loss as detected by blue-on-yellow and standard white-on-white automated perimetry. Arch Ophthalmol. 1993 May;111(5):651–656. doi: 10.1001/archopht.1993.01090050085035. [DOI] [PubMed] [Google Scholar]
- Johnson C. A., Adams A. J., Twelker J. D., Quigg J. M. Age-related changes in the central visual field for short-wavelength-sensitive pathways. J Opt Soc Am A. 1988 Dec;5(12):2131–2139. doi: 10.1364/josaa.5.002131. [DOI] [PubMed] [Google Scholar]
- Johnson C. A., Brandt J. D., Khong A. M., Adams A. J. Short-wavelength automated perimetry in low-, medium-, and high-risk ocular hypertensive eyes. Initial baseline results. Arch Ophthalmol. 1995 Jan;113(1):70–76. doi: 10.1001/archopht.1995.01100010072023. [DOI] [PubMed] [Google Scholar]
- Klein R., Davis M. D., Magli Y. L., Segal P., Klein B. E., Hubbard L. The Wisconsin age-related maculopathy grading system. Ophthalmology. 1991 Jul;98(7):1128–1134. doi: 10.1016/s0161-6420(91)32186-9. [DOI] [PubMed] [Google Scholar]
- Klein R., Klein B. E., Jensen S. C. The relation of cardiovascular disease and its risk factors to the 5-year incidence of age-related maculopathy: the Beaver Dam Eye Study. Ophthalmology. 1997 Nov;104(11):1804–1812. doi: 10.1016/s0161-6420(97)30023-2. [DOI] [PubMed] [Google Scholar]
- Krumpaszky H. G., Klauss V. Epidemiology of blindness and eye disease. Ophthalmologica. 1996;210(1):1–84. doi: 10.1159/000310663. [DOI] [PubMed] [Google Scholar]
- Laatikainen L., Hirvelä H. Prevalence and visual consequences of macular changes in a population aged 70 years and older. Acta Ophthalmol Scand. 1995 Apr;73(2):105–110. doi: 10.1111/j.1600-0420.1995.tb00647.x. [DOI] [PubMed] [Google Scholar]
- Leibowitz H. M., Krueger D. E., Maunder L. R., Milton R. C., Kini M. M., Kahn H. A., Nickerson R. J., Pool J., Colton T. L., Ganley J. P. The Framingham Eye Study monograph: An ophthalmological and epidemiological study of cataract, glaucoma, diabetic retinopathy, macular degeneration, and visual acuity in a general population of 2631 adults, 1973-1975. Surv Ophthalmol. 1980 May-Jun;24(Suppl):335–610. [PubMed] [Google Scholar]
- Midena E., Degli Angeli C., Blarzino M. C., Valenti M., Segato T. Macular function impairment in eyes with early age-related macular degeneration. Invest Ophthalmol Vis Sci. 1997 Feb;38(2):469–477. [PubMed] [Google Scholar]
- Mills R. P., Hopp R. H., Drance S. M. Comparison of quantitative testing with the Octopus, Humphrey, and Tübingen perimeters. Am J Ophthalmol. 1986 Oct 15;102(4):496–504. doi: 10.1016/0002-9394(86)90080-2. [DOI] [PubMed] [Google Scholar]
- Pauleikhoff D., Harper C. A., Marshall J., Bird A. C. Aging changes in Bruch's membrane. A histochemical and morphologic study. Ophthalmology. 1990 Feb;97(2):171–178. [PubMed] [Google Scholar]
- Remky A., Arend O., Hendricks S. Short-wavelength automated perimetry and capillary density in early diabetic maculopathy. Invest Ophthalmol Vis Sci. 2000 Jan;41(1):274–281. [PubMed] [Google Scholar]
- Remky A., Elsner A. E., Morandi A. J., Beausencourt E., Trempe C. L. Blue-on-yellow perimetry with a scanning laser ophthalmoscope: small alterations in the central macula with aging. J Opt Soc Am A Opt Image Sci Vis. 2001 Jul;18(7):1425–1436. doi: 10.1364/josaa.18.001425. [DOI] [PubMed] [Google Scholar]
- Rezai K. A., Kohen L., Wiedemann P., Heimann K. Iris pigment epithelium transplantation. Graefes Arch Clin Exp Ophthalmol. 1997 Sep;235(9):558–562. doi: 10.1007/BF00947084. [DOI] [PubMed] [Google Scholar]
- Sample P. A., Martinez G. A., Weinreb R. N. Short-wavelength automated perimetry without lens density testing. Am J Ophthalmol. 1994 Nov 15;118(5):632–641. doi: 10.1016/s0002-9394(14)76578-x. [DOI] [PubMed] [Google Scholar]
- Sarks S. H. Council Lecture. Drusen and their relationship to senile macular degeneration. Aust J Ophthalmol. 1980 May;8(2):117–130. doi: 10.1111/j.1442-9071.1980.tb01670.x. [DOI] [PubMed] [Google Scholar]
- Smiddy W. E., Fine S. L. Prognosis of patients with bilateral macular drusen. Ophthalmology. 1984 Mar;91(3):271–277. doi: 10.1016/s0161-6420(84)34309-3. [DOI] [PubMed] [Google Scholar]
- Spraul C. W., Grossniklaus H. E. Characteristics of Drusen and Bruch's membrane in postmortem eyes with age-related macular degeneration. Arch Ophthalmol. 1997 Feb;115(2):267–273. doi: 10.1001/archopht.1997.01100150269022. [DOI] [PubMed] [Google Scholar]
- Vinding T., Appleyard M., Nyboe J., Jensen G. Risk factor analysis for atrophic and exudative age-related macular degeneration. An epidemiological study of 1000 aged individuals. Acta Ophthalmol (Copenh) 1992 Feb;70(1):66–72. doi: 10.1111/j.1755-3768.1992.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Vingerling J. R., Dielemans I., Hofman A., Grobbee D. E., Hijmering M., Kramer C. F., de Jong P. T. The prevalence of age-related maculopathy in the Rotterdam Study. Ophthalmology. 1995 Feb;102(2):205–210. doi: 10.1016/s0161-6420(95)31034-2. [DOI] [PubMed] [Google Scholar]
- Wolf S., Lappas A., Weinberger A. W., Kirchhof B. Macular translocation for surgical management of subfoveal choroidal neovascularizations in patients with AMD: first results. Graefes Arch Clin Exp Ophthalmol. 1999 Jan;237(1):51–57. doi: 10.1007/s004170050194. [DOI] [PubMed] [Google Scholar]
- Young R. W. Pathophysiology of age-related macular degeneration. Surv Ophthalmol. 1987 Mar-Apr;31(5):291–306. doi: 10.1016/0039-6257(87)90115-9. [DOI] [PubMed] [Google Scholar]



