Abstract
BACKGROUND/AIMS—Direct closure of eyelid defects gives excellent functional results but is usually restricted to defects measuring less than a quarter of the eyelid length for fear of distorting the palpebral aperture and compromising lid function. The authors have used direct closure in larger defects. The aim of this study was to establish the effects of direct closure of full thickness eyelid margin defects under tension on the palpebral aperture dimensions. METHODS—A consecutive series of patients who had undergone one eyelid, full thickness lid resection repaired by direct closure were identified and invited to have both eyes photographed. The palpebral apertures of both eyes were measured from the photographs by a masked observer. The amount of eyelid resected was recorded from the operation notes. The unoperated palpebral aperture was used as the control. The result were analysed using a paired samples t test. RESULTS—The photographs of 18 patients were included in the analysis. The mean width of excised full thickness lid tissue was 15 mm (range 7-26 mm). The mean vertical palpebral aperture height was 9.2 (SD 1.4) mm in the operated eye as opposed to 9.3 (SD 1.2) mm in the non-operated eye. The mean horizontal palpebral aperture width was 26.1 (SD 1.9) mm in the operated eye as opposed to 26.4 (SD 1.8) mm in the non-operated eye. There was no statistically significant difference between the operated and unoperated horizontal and vertical palpebral measurements. CONCLUSIONS—Direct closure of large full thickness eyelid defects is possible in selected patients with excellent functional and cosmetic results. Eyelid tissue expansion occurs spontaneously following direct eyelid defect closure under tension, restoring the palpebral aperture dimensions.
Full Text
The Full Text of this article is available as a PDF (145.4 KB).
Figure 1 .
These photographs are of a patient not included in the series. (A) The preoperative right lower lid basal cell carcinoma, which measured 11 mm in its horizontal diameter. (B) The 6 month postoperative result after 19 mm horizontal lid resection and direct closure. (C) Also taken at 6 months and allows comparison with the normal unoperated left eye.
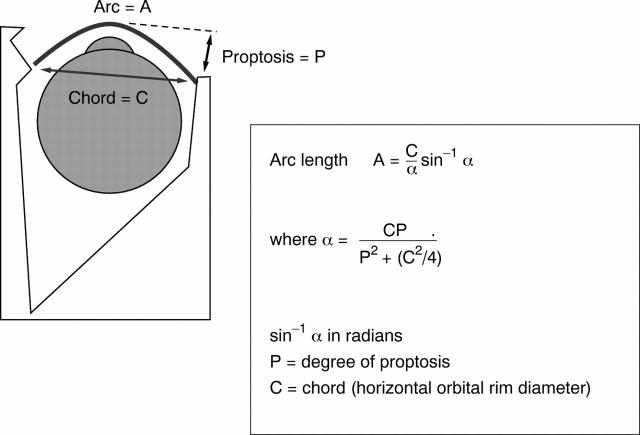
Figure 2 .
Straightening of the normal lid curvature (arc to chord conversion).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Austad E. D., Thomas S. B., Pasyk K. Tissue expansion: dividend or loan? Plast Reconstr Surg. 1986 Jul;78(1):63–67. doi: 10.1097/00006534-198607000-00009. [DOI] [PubMed] [Google Scholar]
- Bennett R. G., Hirt M. A history of tissue expansion. Concepts, controversies, and complications. J Dermatol Surg Oncol. 1993 Dec;19(12):1066–1073. doi: 10.1111/j.1524-4725.1993.tb01001.x. [DOI] [PubMed] [Google Scholar]
- FOX S. A., BEARD C. SPONTANEOUS LID REPAIR. Am J Ophthalmol. 1964 Dec;58:947–952. doi: 10.1016/0002-9394(64)90004-2. [DOI] [PubMed] [Google Scholar]
- Foster J. A., Scheiner A. J., Wulc A. E., Wallace I. B., Greenbaum S. S. Intraoperative tissue expansion in eyelid reconstruction. Ophthalmology. 1998 Jan;105(1):170–175. doi: 10.1016/s0161-6420(98)92009-7. [DOI] [PubMed] [Google Scholar]
- Gibson T., Kenedi R. M., Craik J. E. The mobile micro-architecture of dermal collagen: a bio-engineering study. Br J Surg. 1965 Oct;52(10):764–770. doi: 10.1002/bjs.1800521017. [DOI] [PubMed] [Google Scholar]
- Hawes M. J., Jamell G. A. Complications of tarsoconjunctival grafts. Ophthal Plast Reconstr Surg. 1996 Mar;12(1):45–50. doi: 10.1097/00002341-199603000-00007. [DOI] [PubMed] [Google Scholar]
- Johnson T. M., Brown M. D., Sullivan M. J., Swanson N. A. Immediate intraoperative tissue expansion. J Am Acad Dermatol. 1990 Feb;22(2 Pt 1):283–287. doi: 10.1016/0190-9622(90)70038-j. [DOI] [PubMed] [Google Scholar]
- Johnson T. M., Lowe L., Brown M. D., Sullivan M. J., Nelson B. R. Histology and physiology of tissue expansion. J Dermatol Surg Oncol. 1993 Dec;19(12):1074–1078. doi: 10.1111/j.1524-4725.1993.tb01002.x. [DOI] [PubMed] [Google Scholar]
- Mehta H. K. Spontaneous reformation of lower eyelid. Br J Ophthalmol. 1981 Mar;65(3):202–208. doi: 10.1136/bjo.65.3.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss A. L., Cooper M. A., Lendrum J., Hiles R. W. The sanctity of the upper lid in lower eyelid reconstruction questioned. A modification of a lid sharing procedure with a long-term follow-up. Br J Plast Surg. 1987 May;40(3):246–257. doi: 10.1016/0007-1226(87)90118-4. [DOI] [PubMed] [Google Scholar]
- NEUMANN C. G. The expansion of an area of skin by progressive distention of a subcutaneous balloon; use of the method for securing skin for subtotal reconstruction of the ear. Plast Reconstr Surg (1946) 1957 Feb;19(2):124–130. doi: 10.1097/00006534-195702000-00004. [DOI] [PubMed] [Google Scholar]
- Pietilä J. P., Nordström R. E., Virkkunen P. J., Voutilainen P. E., Rintala A. E. Accelerated tissue expansion with the "overfilling" technique. Plast Reconstr Surg. 1988 Feb;81(2):204–207. doi: 10.1097/00006534-198802000-00011. [DOI] [PubMed] [Google Scholar]
- Putterman A. M. Reconstruction of the eyelids following resection for carcinoma. Clin Plast Surg. 1985 Jul;12(3):393–410. [PubMed] [Google Scholar]
- Tse D. T., McCafferty L. R. Controlled tissue expansion in periocular reconstructive surgery. Ophthalmology. 1993 Feb;100(2):260–268. doi: 10.1016/s0161-6420(93)31661-1. [DOI] [PubMed] [Google Scholar]
- Wohlrab T. M., Rohrbach J. M., Thiel H. J. Leaving the eyelid to its own devices. Ger J Ophthalmol. 1996 Jul;5(4):246–249. [PubMed] [Google Scholar]