Abstract
AIM—To evaluate the accuracy of impression cytology employing a Biopore membrane device in the diagnosis of ocular surface squamous neoplasia (OSSN). METHODS—The histology of patients undergoing excision biopsy for the suspected diagnosis of OSSN over a 20 month period was compared with the reported cytology of impression cytology specimens obtained preoperatively using the Biopore membrane device. RESULTS—25 excision biopsies were performed for suspected OSSN. There was accurate correlation in 20 out of the 25 cases (80%). In three cases (12%), there was poor correlation in that only a few dysplastic cells and hyperkeratosis were noted on cytology, whereas histology showed keratinising dysplasia in two cases and a moderately differentiated keratinising squamous cell carcinoma in the third. There were two cases (8%) of non-correlation—one keratinising dysplasia on histology, but anucleate keratin, squamous metaplasia, and rare atypical cells on cytology, and another case with very mild focal dysplasia on histology but squamous metaplasia on cytology. Review of the cytology showed that dysplastic cells were either rare or absent from the cytology specimens in these two cases; it was felt that these represented sampling problems rather than true false negatives. There were no false positives on cytology. Final diagnosis on histology was squamous cell carcinoma in one; carcinoma in situ in two; keratinising dysplasia in 15, non-keratinising dysplasia in seven. CONCLUSION—Impression cytology employing the Biopore membrane accurately predicts the histological diagnosis of OSSN. The presence of hyperkeratosis, inflammatory cells with only a few dysplastic cells, may indicate high grade keratinising dysplasia or squamous cell carcinoma. The method is both rapid and easy to perform in routine clinical practice. These findings suggest that there may be a role for its use in the initial assessment and follow up of patients with suspected OSSN.
Full Text
The Full Text of this article is available as a PDF (161.1 KB).
Figure 1 .
Impression cytology sampling using the Biopore membrane device.
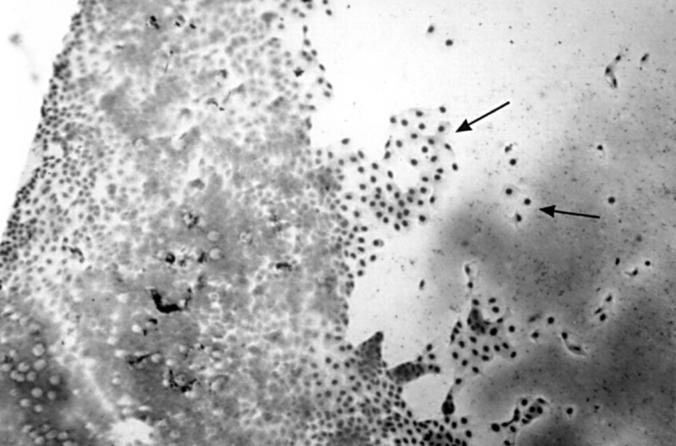
Figure 2 .
Normal ocular surface impression cytology including the limbus. To the left, there are sheets of conjunctival epithelial cells with goblet cells (clear spaces) which merge with the limbus centrally and on the right, corneal epithelial cells which are larger (arrows). Giemsa. Magnification ×200.
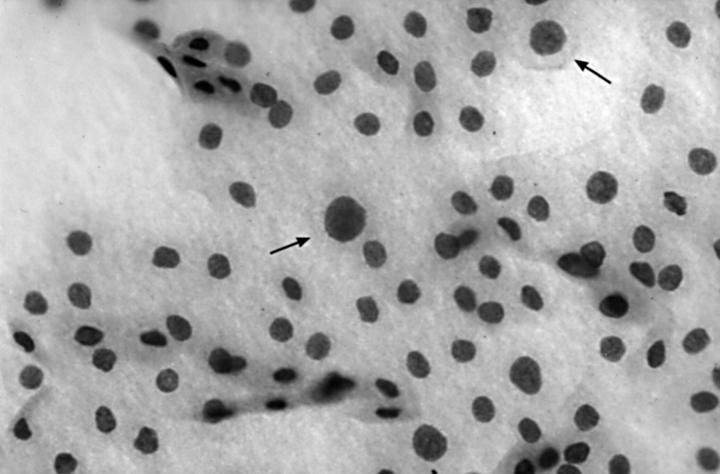
Figure 3 .
Occasional dysplastic cells (arrows) in a case of keratinising dysplasia (case 2). Giemsa. Magnification ×2000.
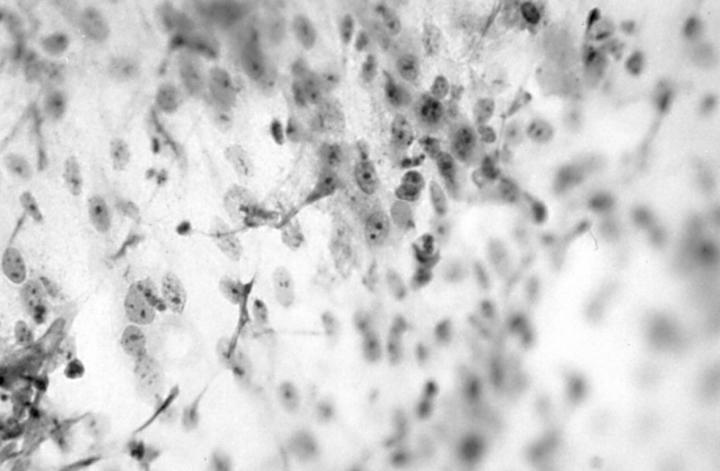
Figure 4 .
Numerous dysplastic cells with prominent nucleoli in severe non-keratinising dysplasia (case 23). Haematoxylin and eosin. Magnification ×2000.
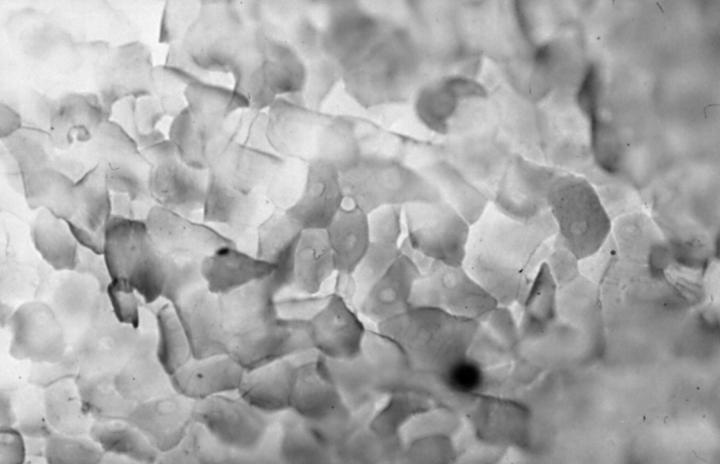
Figure 5 .
Anucleate keratotic debris on impression cytology in a case of keratinising dysplasia (case 2). Giemsa. Magnification ×2000.
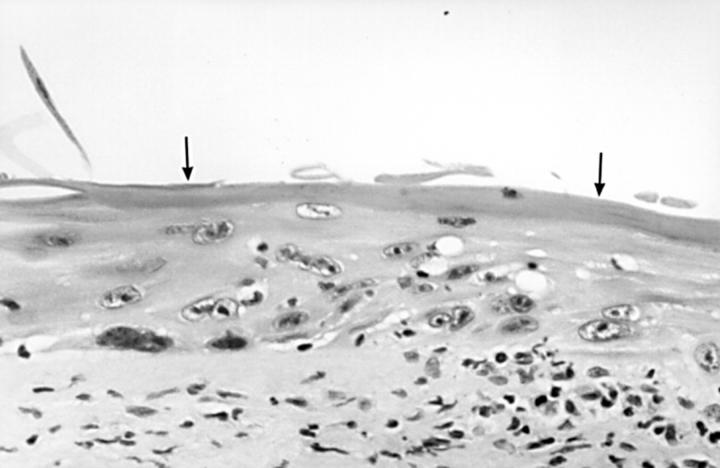
Figure 6 .
Histology of keratinising dysplasia showing thick surface layer of hyperkeratosis, indicated by arrows (case 2). Haematoxylin and eosin ×2000.
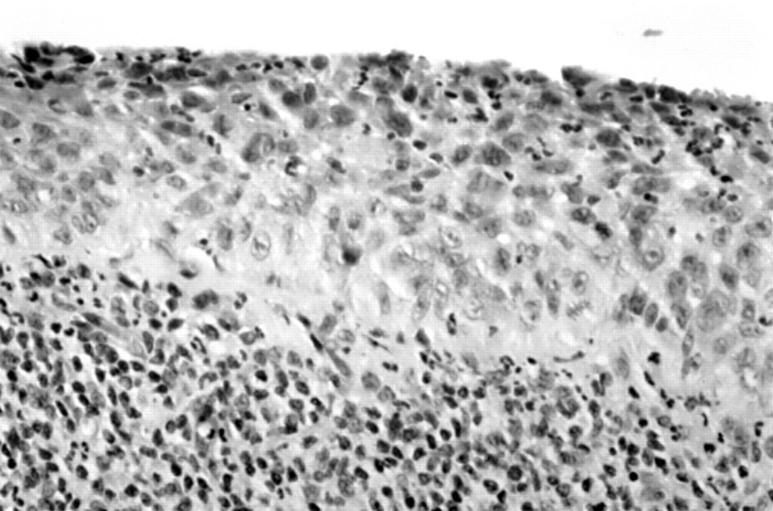
Figure 7 .
Histology of severe non-keratinising dysplasia with dense stromal inflammatory infiltrate and inflammation in the epithelium (case 23). Haematoxylin and eosin ×2000.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Egbert P. R., Lauber S., Maurice D. M. A simple conjunctival biopsy. Am J Ophthalmol. 1977 Dec;84(6):798–801. doi: 10.1016/0002-9394(77)90499-8. [DOI] [PubMed] [Google Scholar]
- Frucht-Pery J., Sugar J., Baum J., Sutphin J. E., Pe'er J., Savir H., Holland E. J., Meisler D. M., Foster J. A., Folberg R. Mitomycin C treatment for conjunctival-corneal intraepithelial neoplasia: a multicenter experience. Ophthalmology. 1997 Dec;104(12):2085–2093. doi: 10.1016/s0161-6420(97)30055-4. [DOI] [PubMed] [Google Scholar]
- Lee G. A., Hirst L. W. Retrospective study of ocular surface squamous neoplasia. Aust N Z J Ophthalmol. 1997 Nov;25(4):269–276. doi: 10.1111/j.1442-9071.1997.tb01514.x. [DOI] [PubMed] [Google Scholar]
- Natadisastra G., Wittpenn J. R., West K. P., Jr, Muhilal, Sommer A. Impression cytology for detection of vitamin A deficiency. Arch Ophthalmol. 1987 Sep;105(9):1224–1228. doi: 10.1001/archopht.1987.01060090082033. [DOI] [PubMed] [Google Scholar]
- Nelson J. D., Havener V. R., Cameron J. D. Cellulose acetate impressions of the ocular surface. Dry eye states. Arch Ophthalmol. 1983 Dec;101(12):1869–1872. doi: 10.1001/archopht.1983.01040020871007. [DOI] [PubMed] [Google Scholar]
- Nolan G. R., Hirst L. W., Bancroft B. J. Efficacy of a training programme designed to teach cervical smear screeners to identify ocular surface squamous neoplasia using conjunctival impression cytology. Cytopathology. 1997 Dec;8(6):388–396. doi: 10.1111/j.1365-2303.1997.tb00569.x. [DOI] [PubMed] [Google Scholar]
- Nolan G. R., Hirst L. W., Wright R. G., Bancroft B. J. Application of impression cytology to the diagnosis of conjunctival neoplasms. Diagn Cytopathol. 1994;11(3):246–249. doi: 10.1002/dc.2840110310. [DOI] [PubMed] [Google Scholar]
- Puangsricharern V., Tseng S. C. Cytologic evidence of corneal diseases with limbal stem cell deficiency. Ophthalmology. 1995 Oct;102(10):1476–1485. doi: 10.1016/s0161-6420(95)30842-1. [DOI] [PubMed] [Google Scholar]
- Salomão D. R., Mathers W. D., Sutphin J. E., Cuevas K., Folberg R. Cytologic changes in the conjunctiva mimicking malignancy after topical mitomycin C chemotherapy. Ophthalmology. 1999 Sep;106(9):1756–1761. doi: 10.1016/S0161-6420(99)90355-X. [DOI] [PubMed] [Google Scholar]
- Thiel M. A., Bossart W., Bernauer W. Improved impression cytology techniques for the immunopathological diagnosis of superficial viral infections. Br J Ophthalmol. 1997 Nov;81(11):984–988. doi: 10.1136/bjo.81.11.984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tseng S. C. Staging of conjunctival squamous metaplasia by impression cytology. Ophthalmology. 1985 Jun;92(6):728–733. doi: 10.1016/s0161-6420(85)33967-2. [DOI] [PubMed] [Google Scholar]