Abstract
AIMS—To investigate if the amniotic membrane (AM) promotes epithelial migration while inhibiting stromal remodelling associated with corneal haze after excimer laser keratectomy. METHODS—A wound 150 µm in depth and 6.0 mm in diameter was produced in 40 rabbits using an excimer laser. One eye was randomly chosen to be covered by the AM while the other eye served as a control. Epithelial wound healing was evaluated, together with any morphological changes of the anterior stroma connected with corneal haze. These morphological changes were histopathologically analysed using dichlortriazinyl aminofluorescein (DTAF), Masson trichrome staining, and an image analyser. RESULTS—The AM group had a short latent phase followed by fast epithelial healing (p<0.001) during the early wound healing period and a significant decrease in the inflammatory response, together with a smaller change in the number of keratocytes than the control group. The mean thickness of the regenerated stroma was significantly thinner in the AM group than in the control group at 8 weeks (p<0.0001). The AM group had a more regular architecture of regenerated stromal lamella at 8 weeks and significantly less haze after 4 weeks than the control group (p<0.05). CONCLUSION—Use of the AM as a dressing on a corneal wound created by excimer laser surgery, in which severe haze is expected, may induce rapid epithelial healing with less inflammatory response. The AM may inhibit the irregular synthesis of stromal collagen that is associated with corneal haze.
Full Text
The Full Text of this article is available as a PDF (179.8 KB).
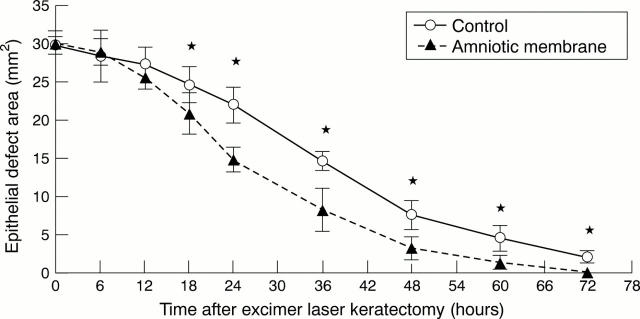
Figure 1 .
Changes in epithelial defect area after excimer laser keratectomy compared with control group. Values are mean (SD). *p<0.01.
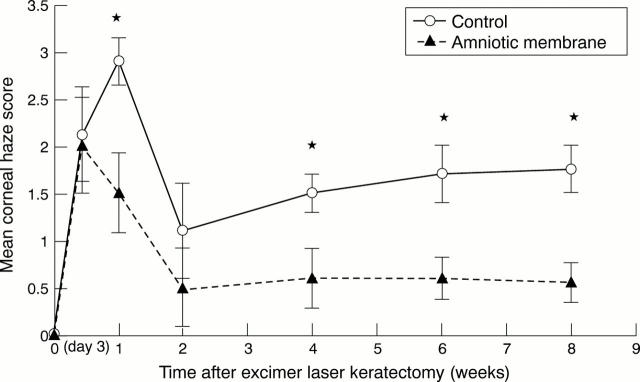
Figure 2 .
Mean (SD) corneal haze scores after excimer laser keratectomy compared with control group. *p<0.05.
Figure 3 .
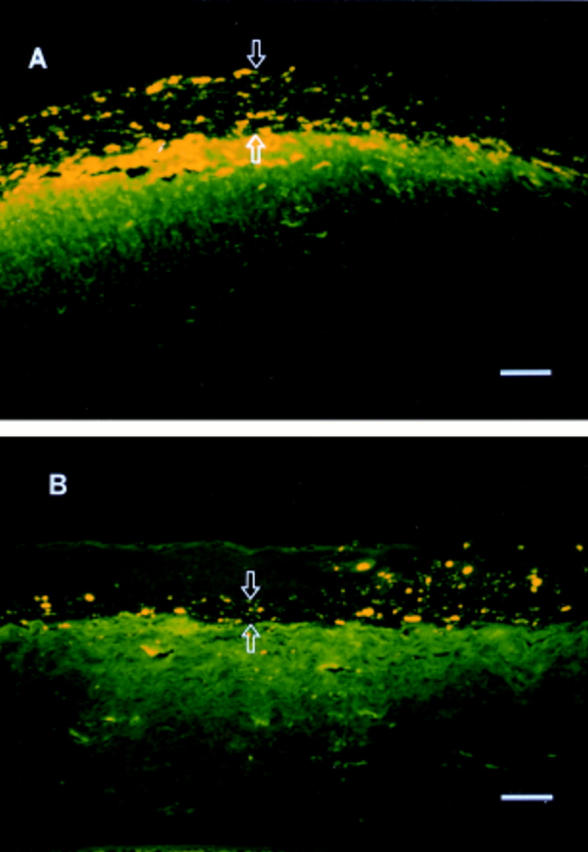
Fluorescence photomicrographs of rabbit corneas at 8 weeks after excimer laser keratectomy (DTAF stain). A significant amount of regenerated collagen (between arrows) dispersed with DTAF dye between the epithelium (upper arrow) and the brightly fluorescent original stromal bed (lower arrow) is present in the control cornea (A) but there is a little unstained collagen (between arrows) in the AM covered cornea (B). Bar = 50 µm.
Figure 4 .
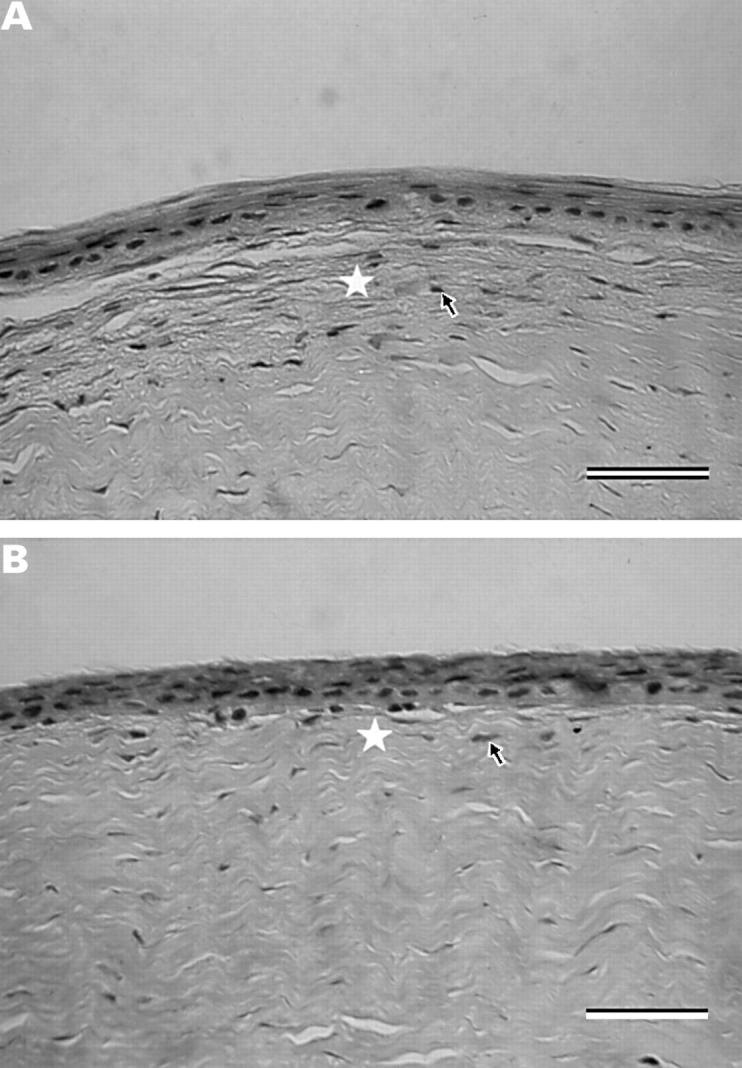
Light micrographs of rabbit corneas at 4 weeks after excimer laser keratectomy (Masson's trichrome stain). The newly formed collagen in the anterior stroma (*) has a more regular architecture in the AM covered cornea (B) than in the control cornea (A). The keratocytes (arrows) beneath the epithelium show less hyperplasia in the AM covered cornea (B) than in the control cornea (A). Bar = 50 µm.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Azuara-Blanco A., Pillai C. T., Dua H. S. Amniotic membrane transplantation for ocular surface reconstruction. Br J Ophthalmol. 1999 Apr;83(4):399–402. doi: 10.1136/bjo.83.4.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Böhnke M., Thaer A., Schipper I. Confocal microscopy reveals persisting stromal changes after myopic photorefractive keratectomy in zero haze corneas. Br J Ophthalmol. 1998 Dec;82(12):1393–1400. doi: 10.1136/bjo.82.12.1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi Y. S., Kim J. Y., Wee W. R., Lee J. H. Effect of the application of human amniotic membrane on rabbit corneal wound healing after excimer laser photorefractive keratectomy. Cornea. 1998 Jul;17(4):389–395. doi: 10.1097/00003226-199807000-00009. [DOI] [PubMed] [Google Scholar]
- Corbett M. C., Prydal J. I., Verma S., Oliver K. M., Pande M., Marshall J. An in vivo investigation of the structures responsible for corneal haze after photorefractive keratectomy and their effect on visual function. Ophthalmology. 1996 Sep;103(9):1366–1380. doi: 10.1016/s0161-6420(96)30495-8. [DOI] [PubMed] [Google Scholar]
- Crosson C. E., Klyce S. D., Beuerman R. W. Epithelial wound closure in the rabbit cornea. A biphasic process. Invest Ophthalmol Vis Sci. 1986 Apr;27(4):464–473. [PubMed] [Google Scholar]
- Davison P. F., Galbavy E. J. Connective tissue remodeling in corneal and scleral wounds. Invest Ophthalmol Vis Sci. 1986 Oct;27(10):1478–1484. [PubMed] [Google Scholar]
- Davison P. F., Galbavy E. J. Fluorescent dyes demonstrate the uniform expansion of the growing rabbit cornea. Invest Ophthalmol Vis Sci. 1985 Sep;26(9):1202–1209. [PubMed] [Google Scholar]
- Fantes F. E., Hanna K. D., Waring G. O., 3rd, Pouliquen Y., Thompson K. P., Savoldelli M. Wound healing after excimer laser keratomileusis (photorefractive keratectomy) in monkeys. Arch Ophthalmol. 1990 May;108(5):665–675. doi: 10.1001/archopht.1990.01070070051034. [DOI] [PubMed] [Google Scholar]
- Gartry D. S., Muir M. G., Lohmann C. P., Marshall J. The effect of topical corticosteroids on refractive outcome and corneal haze after photorefractive keratectomy. A prospective, randomized, double-blind trial. Arch Ophthalmol. 1992 Jul;110(7):944–952. doi: 10.1001/archopht.1992.01080190050028. [DOI] [PubMed] [Google Scholar]
- Gartry D., Kerr Muir M., Marshall J. Excimer laser treatment of corneal surface pathology: a laboratory and clinical study. Br J Ophthalmol. 1991 May;75(5):258–269. doi: 10.1136/bjo.75.5.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J. C., Tseng S. C. Transplantation of preserved human amniotic membrane for surface reconstruction in severely damaged rabbit corneas. Cornea. 1995 Sep;14(5):473–484. [PubMed] [Google Scholar]
- Koizumi N. J., Inatomi T. J., Sotozono C. J., Fullwood N. J., Quantock A. J., Kinoshita S. Growth factor mRNA and protein in preserved human amniotic membrane. Curr Eye Res. 2000 Mar;20(3):173–177. [PubMed] [Google Scholar]
- Larkin D. F., Alexander R. A., Cree I. A. Infiltrating inflammatory cell phenotypes and apoptosis in rejected human corneal allografts. Eye (Lond) 1997;11(Pt 1):68–74. doi: 10.1038/eye.1997.13. [DOI] [PubMed] [Google Scholar]
- Latvala T., Tervo K., Mustonen R., Tervo T. Expression of cellular fibronectin and tenascin in the rabbit cornea after excimer laser photorefractive keratectomy: a 12 month study. Br J Ophthalmol. 1995 Jan;79(1):65–69. doi: 10.1136/bjo.79.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall J., Trokel S., Rothery S., Krueger R. R. A comparative study of corneal incisions induced by diamond and steel knives and two ultraviolet radiations from an excimer laser. Br J Ophthalmol. 1986 Jul;70(7):482–501. doi: 10.1136/bjo.70.7.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Møller-Pedersen T., Li H. F., Petroll W. M., Cavanagh H. D., Jester J. V. Confocal microscopic characterization of wound repair after photorefractive keratectomy. Invest Ophthalmol Vis Sci. 1998 Mar;39(3):487–501. [PubMed] [Google Scholar]
- O'Brart D. P., Lohmann C. P., Klonos G., Corbett M. C., Pollock W. S., Kerr-Muir M. G., Marshall J. The effects of topical corticosteroids and plasmin inhibitors on refractive outcome, haze, and visual performance after photorefractive keratectomy. A prospective, randomized, observer-masked study. Ophthalmology. 1994 Sep;101(9):1565–1574. doi: 10.1016/s0161-6420(94)38032-8. [DOI] [PubMed] [Google Scholar]
- Park C. K., Kim J. H. Comparison of wound healing after photorefractive keratectomy and laser in situ keratomileusis in rabbits. J Cataract Refract Surg. 1999 Jun;25(6):842–850. doi: 10.1016/s0886-3350(99)00047-4. [DOI] [PubMed] [Google Scholar]
- Schworm H. D., Eithoff S., Schaumberger M., Boergen K. P. Investigations on subjective and objective cyclorotatory changes after inferior oblique muscle recession. Invest Ophthalmol Vis Sci. 1997 Feb;38(2):405–412. [PubMed] [Google Scholar]
- Seiler T., McDonnell P. J. Excimer laser photorefractive keratectomy. Surv Ophthalmol. 1995 Sep-Oct;40(2):89–118. doi: 10.1016/s0039-6257(95)80001-8. [DOI] [PubMed] [Google Scholar]
- Siganos D. S., Katsanevaki V. J., Pallikaris I. G. Correlation of subepithelial haze and refractive regression 1 month after photorefractive keratectomy for myopia. J Refract Surg. 1999 May-Jun;15(3):338–342. doi: 10.3928/1081-597X-19990501-10. [DOI] [PubMed] [Google Scholar]
- SundarRaj N., Geiss M. J., 3rd, Fantes F., Hanna K., Anderson S. C., Thompson K. P., Thoft R. A., Waring G. O., 3rd Healing of excimer laser ablated monkey corneas. An immunohistochemical evaluation. Arch Ophthalmol. 1990 Nov;108(11):1604–1610. doi: 10.1001/archopht.1990.01070130106039. [DOI] [PubMed] [Google Scholar]
- Szerenyi K. D., Wang X., Gabrielian K., McDonnell P. J. Keratocyte loss and repopulation of anterior corneal stroma after de-epithelialization. Arch Ophthalmol. 1994 Jul;112(7):973–976. doi: 10.1001/archopht.1994.01090190121031. [DOI] [PubMed] [Google Scholar]
- Tseng S. C., Li D. Q., Ma X. Suppression of transforming growth factor-beta isoforms, TGF-beta receptor type II, and myofibroblast differentiation in cultured human corneal and limbal fibroblasts by amniotic membrane matrix. J Cell Physiol. 1999 Jun;179(3):325–335. doi: 10.1002/(SICI)1097-4652(199906)179:3<325::AID-JCP10>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- Tseng S. C., Prabhasawat P., Barton K., Gray T., Meller D. Amniotic membrane transplantation with or without limbal allografts for corneal surface reconstruction in patients with limbal stem cell deficiency. Arch Ophthalmol. 1998 Apr;116(4):431–441. doi: 10.1001/archopht.116.4.431. [DOI] [PubMed] [Google Scholar]
- Tuft S. J., Zabel R. W., Marshall J. Corneal repair following keratectomy. A comparison between conventional surgery and laser photoablation. Invest Ophthalmol Vis Sci. 1989 Aug;30(8):1769–1777. [PubMed] [Google Scholar]
- Wilson C. A., Berkowitz B. A., Srebro R. Perfluorinated organic liquid as an intraocular oxygen reservoir for the ischemic retina. Invest Ophthalmol Vis Sci. 1995 Jan;36(1):131–141. [PubMed] [Google Scholar]
- Wilson S. E. Molecular cell biology for the refractive corneal surgeon: programmed cell death and wound healing. J Refract Surg. 1997 Mar-Apr;13(2):171–175. doi: 10.3928/1081-597X-19970301-15. [DOI] [PubMed] [Google Scholar]
- Wu W. C., Stark W. J., Green W. R. Corneal wound healing after 193-nm excimer laser keratectomy. Arch Ophthalmol. 1991 Oct;109(10):1426–1432. doi: 10.1001/archopht.1991.01080100106053. [DOI] [PubMed] [Google Scholar]