Abstract
BACKGROUND—Congenital nasolacrimal obstruction is usually the result of failure of canalisation of the distal end of the nasolacrimal duct. The most common outcome is spontaneous resolution, but some children do require surgical treatment by probing. Probing is a blind procedure with a recognised failure rate. METHODS—In 52 lacrimal systems of 40 children nasal endoscopy was combined with a "stepwise" systematic probing in an attempt to improve the outcome and reduce the number of repeat procedures. RESULTS—Combined nasal endoscopy and probing improved the understanding of outflow obstruction in young children. The success of the procedure depended upon the level of the obstruction within the outflow system. Formation of a false passage was seen in six cases (15%). The probe was rerouted under direct visualisation in these cases to form a functioning passage. Reasons for failure were identified in those who did not have a successful outcome and only one repeat procedure was required. CONCLUSION—Using nasal endoscopy the area of lacrimal outflow obstruction at the lower end of the nasolacrimal duct can be observed directly and it is possible to guide the progress of probing under direct vision. This gives better information about the nature of the obstruction, minimises the formation of false passages, and allows a wider range of treatment options under a single anaesthetic.
Full Text
The Full Text of this article is available as a PDF (117.6 KB).
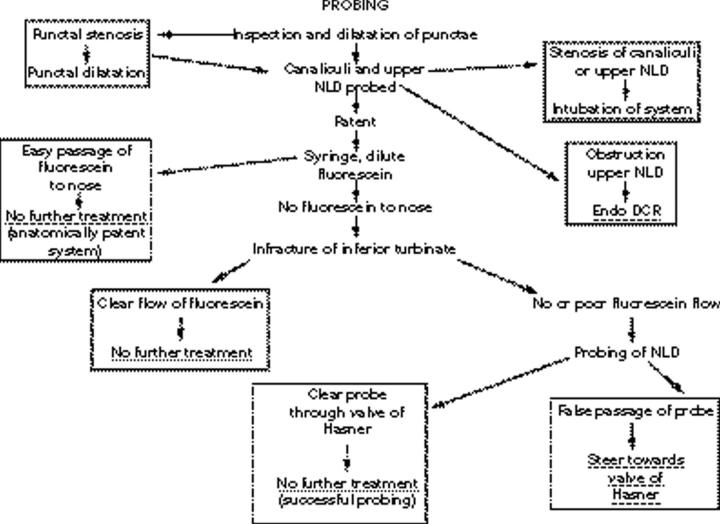
Figure 1 .
Flow diagram indicating the steps taken in probing.
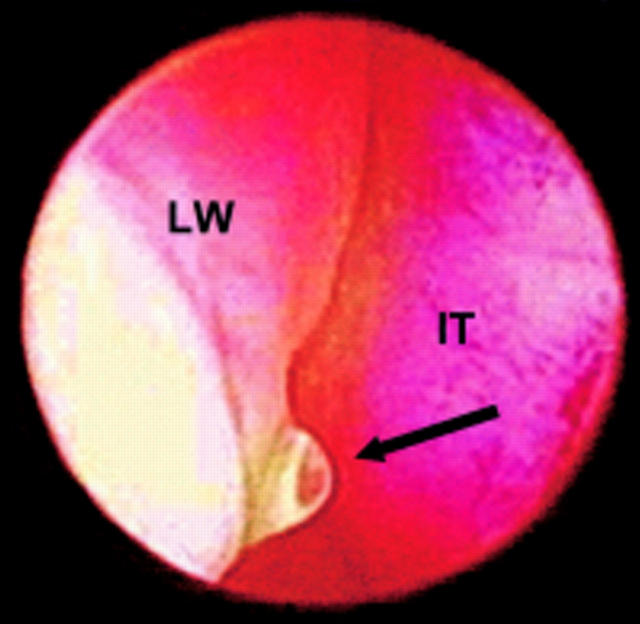
Figure 2 .
A bubble of fluorescein seen entering the nose in an intermittent manner in a case of stenosis of the distal end of the nasolacrimal. Arrow points to stenosed punctum. IT= inferior turbinate; LW = lateral wall.
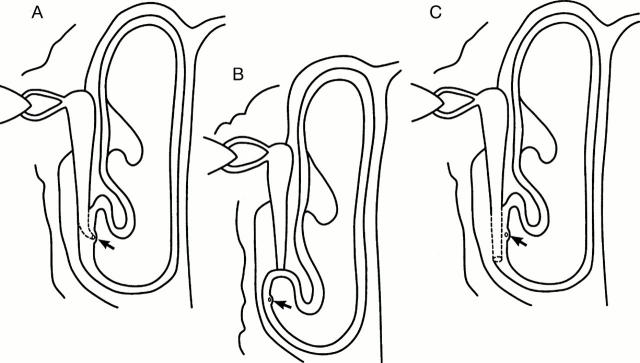
Figure 3 .
Diagrammatic representation of the possible methods that the nasolacrimal duct (NLD) may enter the nose. (A) Normal relation between osseous NLD and the mucosal exit. (B) The osseous NLD is shorter, with exit of the probe at the apex of the inferior meatus. (C) The osseous NLD is longer and the probe enters the submucosal space and passes to the floor of the nose, without entering the nose.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- CASSADY J. V. Developmental anatomy of nasolacrimal duct. AMA Arch Ophthalmol. 1952 Feb;47(2):141–158. doi: 10.1001/archopht.1952.01700030146003. [DOI] [PubMed] [Google Scholar]
- Ffooks O. O. DACRYOCYSTITIS IN INFANCY. Br J Ophthalmol. 1962 Jul;46(7):422–434. doi: 10.1136/bjo.46.7.422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossmann T., Putz R. Uber die angeborene Tränengangstenose der neugeborenen, ihre Anatomie, ihre Folgen und Behandlung. Klin Monbl Augenheilkd. 1972 May;160(5):563–572. [PubMed] [Google Scholar]
- Ingels K., Kestelyn P., Meire F., Ingels G., Van Weissenbruch R. The endoscopic approach for congenital nasolacrimal duct obstruction. Clin Otolaryngol Allied Sci. 1997 Apr;22(2):96–99. doi: 10.1046/j.1365-2273.1997.00846.x. [DOI] [PubMed] [Google Scholar]
- KENDIG E. L., Jr, GUERRY D., 3rd The incidence of congenital impotency of the nasolacrimal duct. J Pediatr. 1950 Feb;36(2):212–212. doi: 10.1016/s0022-3476(50)80206-8. [DOI] [PubMed] [Google Scholar]
- Katowitz J. A., Welsh M. G. Timing of initial probing and irrigation in congenital nasolacrimal duct obstruction. Ophthalmology. 1987 Jun;94(6):698–705. doi: 10.1016/s0161-6420(87)33392-5. [DOI] [PubMed] [Google Scholar]
- MacEwen C. J., Young J. D. Epiphora during the first year of life. Eye (Lond) 1991;5(Pt 5):596–600. doi: 10.1038/eye.1991.103. [DOI] [PubMed] [Google Scholar]
- MacEwen C. J., Young J. D. The fluorescein disappearance test (FDT): an evaluation of its use in infants. J Pediatr Ophthalmol Strabismus. 1991 Nov-Dec;28(6):302–305. doi: 10.3928/0191-3913-19911101-04. [DOI] [PubMed] [Google Scholar]
- Maini R., MacEwen C. J., Young J. D. The natural history of epiphora in childhood. Eye (Lond) 1998;12(Pt 4):669–671. doi: 10.1038/eye.1998.166. [DOI] [PubMed] [Google Scholar]
- Nelson L. R., Calhoun J. H., Menduke H. Medical management of congenital nasolacrimal duct obstruction. Ophthalmology. 1985 Sep;92(9):1187–1190. doi: 10.1016/s0161-6420(85)33878-2. [DOI] [PubMed] [Google Scholar]
- Noda S., Hayasaka S., Setogawa T. Congenital nasolacrimal duct obstruction in Japanese infants: its incidence and treatment with massage. J Pediatr Ophthalmol Strabismus. 1991 Jan-Feb;28(1):20–22. [PubMed] [Google Scholar]
- Nucci P., Capoferri C., Alfarano R., Brancato R. Conservative management of congenital nasolacrimal duct obstruction. J Pediatr Ophthalmol Strabismus. 1989 Jan-Feb;26(1):39–43. doi: 10.3928/0191-3913-19890101-10. [DOI] [PubMed] [Google Scholar]
- Paul T. O. Medical management of congenital nasolacrimal duct obstruction. J Pediatr Ophthalmol Strabismus. 1985 Mar-Apr;22(2):68–70. doi: 10.3928/0191-3913-19850301-09. [DOI] [PubMed] [Google Scholar]
- Paul T. O., Shepherd R. Congenital nasolacrimal duct obstruction: natural history and the timing of optimal intervention. J Pediatr Ophthalmol Strabismus. 1994 Nov-Dec;31(6):362–367. doi: 10.3928/0191-3913-19941101-04. [DOI] [PubMed] [Google Scholar]
- Petersen R. A., Robb R. M. The natural course of congenital obstruction of the nasolacrimal duct. J Pediatr Ophthalmol Strabismus. 1978 Jul-Aug;15(4):246–250. doi: 10.3928/0191-3913-19780701-14. [DOI] [PubMed] [Google Scholar]
- Ram B., Barras C. W., White P. S., MacEwen C. J., Young J. D. The technique of nasendoscopy in the evaluation of nasolacrimal duct obstruction in children. Rhinology. 2000 Jun;38(2):83–86. [PubMed] [Google Scholar]
- Robb R. M. Success rates of nasolacrimal duct probing at time intervals after 1 year of age. Ophthalmology. 1998 Jul;105(7):1307–1310. doi: 10.1016/S0161-6420(98)97038-5. [DOI] [PubMed] [Google Scholar]
- Sturrock S. M., MacEwen C. J., Young J. D. Long-term results after probing for congenital nasolacrimal duct obstruction. Br J Ophthalmol. 1994 Dec;78(12):892–894. doi: 10.1136/bjo.78.12.892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesley R. E. Inferior turbinate fracture in the treatment of congenital nasolacrimal duct obstruction and congenital nasolacrimal duct anomaly. Ophthalmic Surg. 1985 Jun;16(6):368–371. [PubMed] [Google Scholar]
- Young J. D., MacEwen C. J., Ogston S. A. Congenital nasolacrimal duct obstruction in the second year of life: a multicentre trial of management. Eye (Lond) 1996;10(Pt 4):485–491. doi: 10.1038/eye.1996.107. [DOI] [PubMed] [Google Scholar]
- el-Mansoury J., Calhoun J. H., Nelson L. B., Harley R. D. Results of late probing for congenital nasolacrimal duct obstruction. Ophthalmology. 1986 Aug;93(8):1052–1054. doi: 10.1016/s0161-6420(86)33621-2. [DOI] [PubMed] [Google Scholar]