Abstract
BACKGROUND/AIMS—Tuberous sclerosis complex (TSC) has retinal and non-retinal ophthalmic manifestations. This study was designed to determine the prevalence of the ophthalmic manifestations and of refractive errors in a population of patients with TSC. METHODS—179 patients identified were in a prevalence study of TSC in the south of England and 107 of these agreed to full ophthalmic examination which was successful in 100. Ophthalmic examination included examination of the eyelids, cover test, examination of the irides, dilation funduscopy using both direct and indirect ophthalmoscopy, and refraction using retinoscopy. Myopia was defined as a spherical equivalent <−0.5D and hyperopia as a spherical equivalent >+0.5D. RESULTS—Retinal hamartomas were seen in 44 of the 100 patients. The commonest morphological type of hamartoma seen was the flat, translucent lesion in 31 of the 44 patients (70%). The multinodular "mulberry" lesion was seen in 24 of the 44 patients (55%) and the transitional type lesion was seen in four of the 44 patients (9%). Punched out areas of retinal depigmentation were seen in 39 of the 100 patients but only six of 100 controls. 27% of eyes were myopic, 22% were hyperopic, and 27% had astigmatism >0.75D. Of the non-retinal findings, 39 patients had angiofibromas of the eyelids, five had non-paralytic strabismus, and three had colobomas. CONCLUSION—Apart from the higher prevalence of flat retinal hamartomas, the findings of this study compare closely with previous large clinic based series of TSC patients. Refractive findings were similar to previous studies of a similarly aged non-TSC population. This is the first series to document the statistically significant association of punched out chorioretinal depigmentation with TSC and the authors believe that it should be looked for as an aid to diagnosis.
Full Text
The Full Text of this article is available as a PDF (126.0 KB).
Figure 1 .
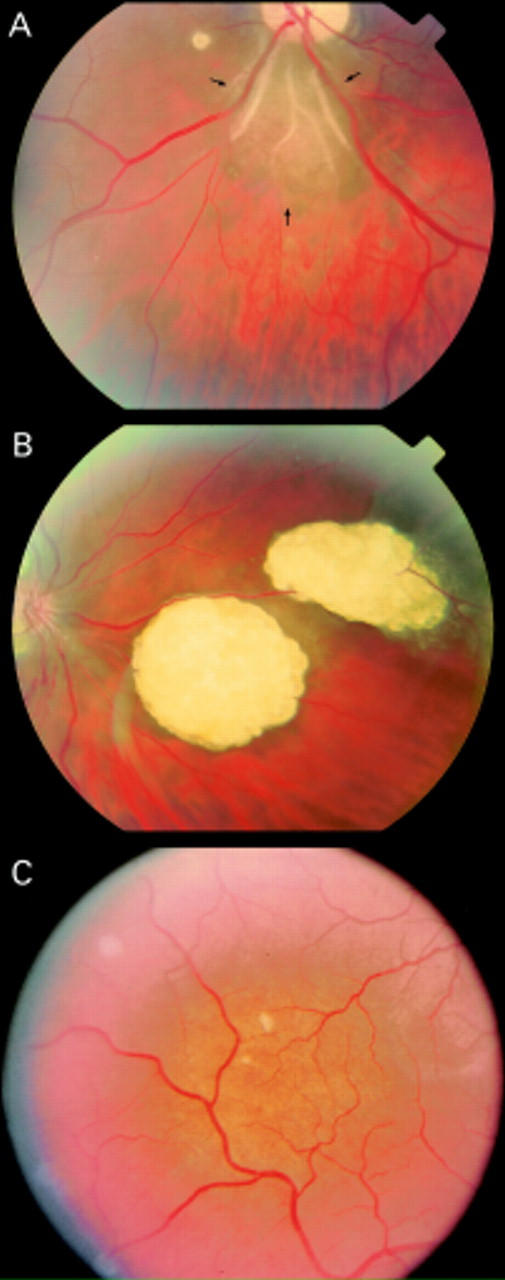
(A) Smooth non-calcified retinal hamartoma (arrowed). (B) Calcified, multinodular retinal hamartomas ("mulberry tumours"). (C) "Punched out" areas of chorioretinal depigmentation.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aine E. Refractive errors in a Finnish rural population. Acta Ophthalmol (Copenh) 1984 Dec;62(6):944–954. doi: 10.1111/j.1755-3768.1984.tb08447.x. [DOI] [PubMed] [Google Scholar]
- Attebo K., Ivers R. Q., Mitchell P. Refractive errors in an older population: the Blue Mountains Eye Study. Ophthalmology. 1999 Jun;106(6):1066–1072. doi: 10.1016/S0161-6420(99)90251-8. [DOI] [PubMed] [Google Scholar]
- Fledelius H. C. Prevalences of astigmatism and anisometropia in adult danes. With reference to presbyopes' possible use of supermarket standard glasses. Acta Ophthalmol (Copenh) 1984 Jun;62(3):391–400. doi: 10.1111/j.1755-3768.1984.tb08419.x. [DOI] [PubMed] [Google Scholar]
- Kiribuchi K., Uchida Y., Fukuyama Y., Maruyama H. High incidence of fundus hamartomas and clinical significance of a fundus score in tuberous sclerosis. Brain Dev. 1986;8(5):509–517. doi: 10.1016/s0387-7604(86)80096-1. [DOI] [PubMed] [Google Scholar]
- Lucchese N. J., Goldberg M. F. Iris and fundus pigmentary changes in tuberous sclerosis. J Pediatr Ophthalmol Strabismus. 1981 Nov-Dec;18(6):45–46. doi: 10.3928/0191-3913-19811101-12. [DOI] [PubMed] [Google Scholar]
- Nyboer J. H., Robertson D. M., Gomez M. R. Retinal lesions in tuberous sclerosis. Arch Ophthalmol. 1976 Aug;94(8):1277–1280. doi: 10.1001/archopht.1976.03910040149003. [DOI] [PubMed] [Google Scholar]
- O'Callaghan F. J., Osborne J. P. Advances in the understanding of tuberous sclerosis. Arch Dis Child. 2000 Aug;83(2):140–142. doi: 10.1136/adc.83.2.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roach E. S., Gomez M. R., Northrup H. Tuberous sclerosis complex consensus conference: revised clinical diagnostic criteria. J Child Neurol. 1998 Dec;13(12):624–628. doi: 10.1177/088307389801301206. [DOI] [PubMed] [Google Scholar]
- Robertson D. M. Ophthalmic manifestations of tuberous sclerosis. Ann N Y Acad Sci. 1991;615:17–25. doi: 10.1111/j.1749-6632.1991.tb37744.x. [DOI] [PubMed] [Google Scholar]
- Shelton R. W. The incidence of ocular lesions in tuberous sclerosis. Ann Ophthalmol. 1975 Jun;7(6):771–774. [PubMed] [Google Scholar]
- Sperduto R. D., Seigel D., Roberts J., Rowland M. Prevalence of myopia in the United States. Arch Ophthalmol. 1983 Mar;101(3):405–407. doi: 10.1001/archopht.1983.01040010405011. [DOI] [PubMed] [Google Scholar]
- Teasdale T. W., Fuchs J., Goldschmidt E. Degree of myopia in relation to intelligence and educational level. Lancet. 1988 Dec 10;2(8624):1351–1354. doi: 10.1016/s0140-6736(88)90880-x. [DOI] [PubMed] [Google Scholar]
- Wang Q., Klein B. E., Klein R., Moss S. E. Refractive status in the Beaver Dam Eye Study. Invest Ophthalmol Vis Sci. 1994 Dec;35(13):4344–4347. [PubMed] [Google Scholar]
- Webb D. W., Fryer A. E., Osborne J. P. Morbidity associated with tuberous sclerosis: a population study. Dev Med Child Neurol. 1996 Feb;38(2):146–155. doi: 10.1111/j.1469-8749.1996.tb12086.x. [DOI] [PubMed] [Google Scholar]
- Zimmer-Galler I. E., Robertson D. M. Long-term observation of retinal lesions in tuberous sclerosis. Am J Ophthalmol. 1995 Mar;119(3):318–324. doi: 10.1016/s0002-9394(14)71174-2. [DOI] [PubMed] [Google Scholar]


