Abstract
AIMS—To analyse the histopathology of vascularised pigment epithelial detachments and tears of the retinal pigment epithelium (RPE) in age related macular degeneration (AMD). METHODS—The light microscopic architecture of 10 surgically removed subretinal specimens—three vascularised pigment epithelial detachments, four recent tears, and three scarred tears as a manifestation of AMD—were studied and correlated with the angiographic findings. RESULTS—Recent tears: a large fibrovascular membrane was found to be originally situated in Bruch's membrane. About half of the surface of the fibrovascular tissue was denuded of RPE and diffuse drusen. The RPE and diffuse drusen had retracted and rolled up, covering a neighbouring part of the intra-Bruch's fibrovascular membrane. The rolled up RPE and diffuse drusen were not interspersed with fibrovascular tissue but lay superficial to the intra-Bruch's fibrovascular membrane itself. Scarred tears: a collagen capsule surrounded the rolled up diffuse drusen and RPE. Fibrovascular tissue was found inside the rolled up material, predominantly at its choroidal side. CONCLUSION—The area of choroidal neovascularisation associated with a vascularised pigment epithelial detachment and a tear of the RPE may be larger than was hitherto thought or indicated by fluorescein angiography. This neovascular tissue may be present within the bed of the RPE tear, as well as at the site of the scrolled up RPE.
Full Text
The Full Text of this article is available as a PDF (260.3 KB).
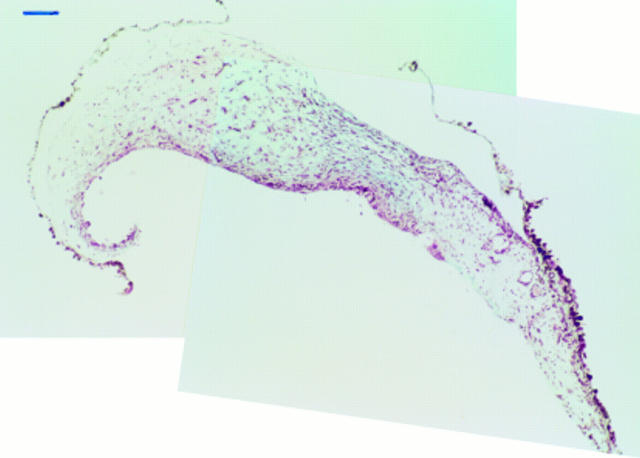
Figure 1 .
Specimen corresponding to a vascularised pigment epithelial detachment with non-homogeneous fluorescein filling. Indocyanine green angiography revealed an ill defined underlying plaque (case 1). The RPE and diffuse drusen have partially detached from the intra-Bruch's fibrovascular tissue. Masson trichrome, bar = 100 µm.
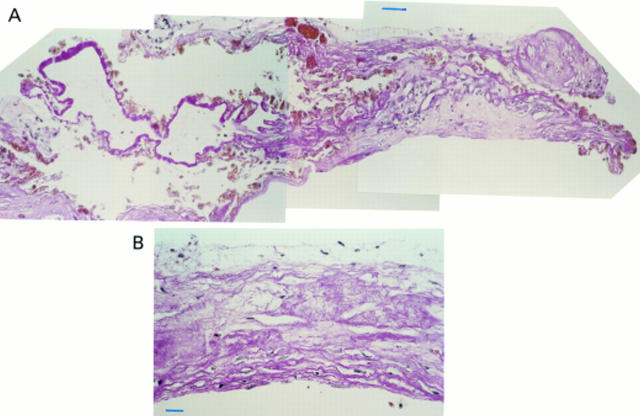
Figure 2 .
Specimen corresponding to a recent tear (case 5). (A) At one edge of the specimen intra-Bruch's fibrovascular tissue is recognised, more centrally to it rolled up RPE and diffuse drusen are seen that are only partially covered by fibrovascular tissue and amorphous debris on their retinal side. (B) Towards the opposite edge, rather fibrous fibrovascular membrane is observed denuded of RPE and diffuse drusen but covered by a thin layer of amorphous debris. Periodic acid Schiff, bar = 50 µm in (A) and 25 µm in (B).
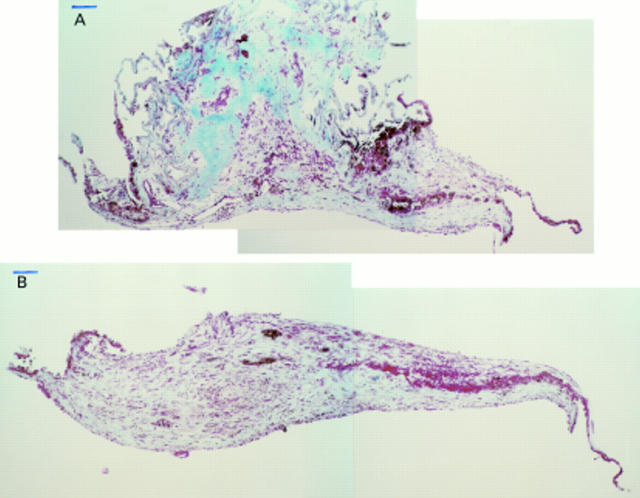
Figure 3 .
Specimen corresponding to a recent tear (case 7). (A) At the level of the rolled up RPE and diffuse drusen, at both edges RPE and diffuse drusen allow orientation of the section. (B) Distant to the rolled up RPE and diffuse drusen, fibrovascular tissue is found that is centrally denuded from RPE and diffuse drusen. The latter structures are, however, identified at the edge of the section and suggest that at least the majority at this level is situated in the Bruch's membrane. Masson trichrome, bar = 100 µm in (A) and (B).
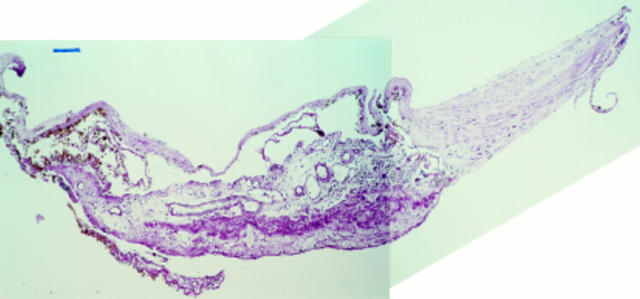
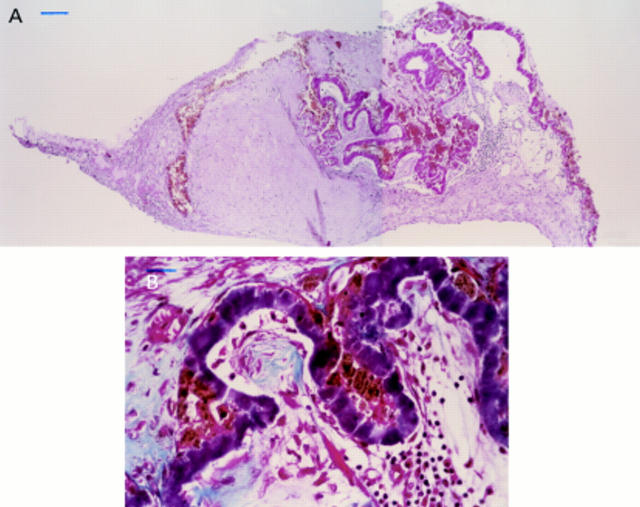
Figure 4 .
Specimen corresponding to a less recent tear (case 8). Rolled up RPE and diffuse drusen, which are covered by a thin fibrocellular membrane on their retinal side, are readily recognised. On their choroidal side fibrovascular tissue is observed with large bore vessels and a moderately strong inflammatory cell infiltration. Adjacent to this part of the specimen, fibrovascular tissue denuded of RPE and diffuse drusen but covered by a thin layer of amorphous debris is found. At one edge of the specimen, RPE, diffuse drusen, and a thin layer of intra-Bruch's fibrovascular tissue are found that has, however, turned over as shown on serial sectioning. At the opposite edge, RPE, diffuse drusen and a thin layer of intra-Bruch's fibrovascular tissue is found that has also turned over but does not physically make contact with the edge of the section itself at this level. Periodic acid Schiff, bar = 100 µm.
Figure 5 .
Specimen corresponding to a scarred tear (case 10). (A) Rolled up RPE and diffuse drusen are found centrally embedded in a fibrous capsule. At one side an intra-Bruch's fibrovascular membrane is recognised whereas the fibrovascular tissue at the other side of the specimen cannot be attributed since it is entirely denuded of RPE and diffuse drusen. In some areas the diffuse drusen are not accompanied by pigmented cells and a group of pigmented cells has migrated from the diffuse drusen and appears to separate the densely collagenised nodule from the remainder of the specimen. A moderately strong inflammatory cell infiltration is seen at the choroidal side of the rolled up diffuse drusen. (B) Detail of rolled up drusen with interspersing fibrovascular and inflammatory tissue at their choroidal side. Masson trichrome, bar = 100 µm in (A) and 25 µm in (B).
Figure 6 .
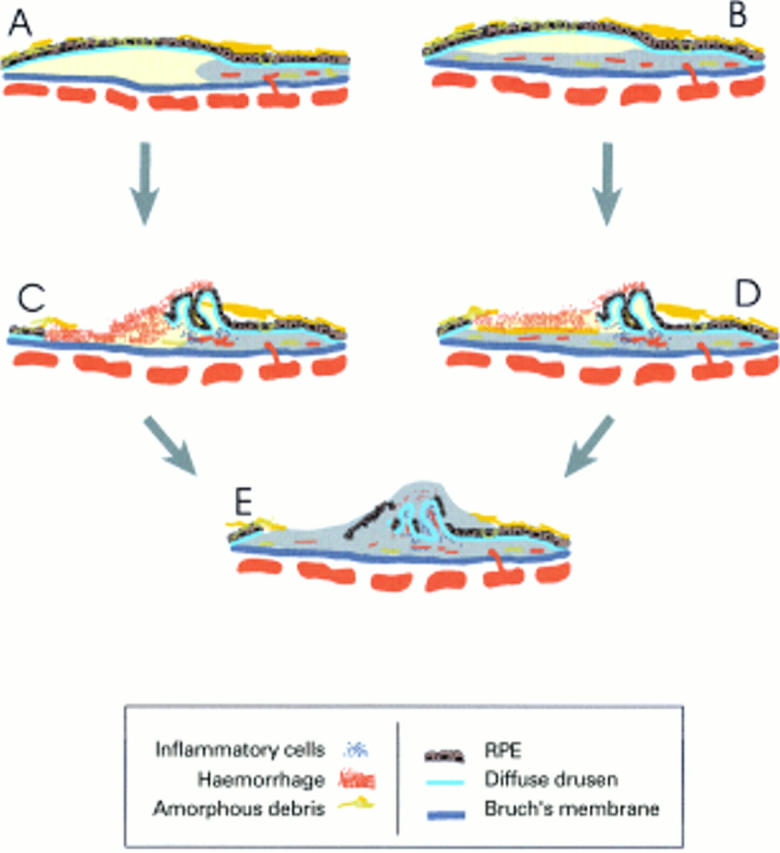
Hypothesis of a flow chart for the histoarchitectural stages that ultimately may lead to a scarred tear of the retinal pigment epithelium. (A) Corresponds to a vascularised PED with a plaque or hot spot, (B) corresponds to a pretear PED, (C) and (D) correspond to fresh tears respectively without or with denuded intra-Bruch's fibrovascular tissue, and finally (E) represents a scarred tear.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arroyo J. G., Schatz H., McDonald R., Johnson R. N. Indocyanine green videoangiography after acute retinal pigment epithelial tears in age-related macular degeneration. Am J Ophthalmol. 1997 Mar;123(3):377–385. doi: 10.1016/s0002-9394(14)70134-5. [DOI] [PubMed] [Google Scholar]
- Bressler N. M., Finklestein D., Sunness J. S., Maguire A. M., Yarian D. Retinal pigment epithelial tears through the fovea with preservation of good visual acuity. Arch Ophthalmol. 1990 Dec;108(12):1694–1697. doi: 10.1001/archopht.1990.01070140048026. [DOI] [PubMed] [Google Scholar]
- Cantrill H. L., Ramsay R. C., Knobloch W. H. Rips in the pigment epithelium. Arch Ophthalmol. 1983 Jul;101(7):1074–1079. doi: 10.1001/archopht.1983.01040020076013. [DOI] [PubMed] [Google Scholar]
- Chuang E. L., Bird A. C. Repair after tears of the retinal pigment epithelium. Eye (Lond) 1988;2(Pt 1):106–113. doi: 10.1038/eye.1988.22. [DOI] [PubMed] [Google Scholar]
- Chuang E. L., Bird A. C. The pathogenesis of tears of the retinal pigment epithelium. Am J Ophthalmol. 1988 Mar 15;105(3):285–290. doi: 10.1016/0002-9394(88)90011-6. [DOI] [PubMed] [Google Scholar]
- Colucciello M., Ginsburg L. H., Sammartino J. P. Indocyanine green angiographic evaluation of retinal pigment epithelial tears. Retina. 1997;17(1):23–27. doi: 10.1097/00006982-199701000-00005. [DOI] [PubMed] [Google Scholar]
- Coscas G., Koenig F., Soubrane G. The pretear characteristics of pigment epithelial detachments. A study of 40 eyes. Arch Ophthalmol. 1990 Dec;108(12):1687–1693. doi: 10.1001/archopht.1990.01070140041025. [DOI] [PubMed] [Google Scholar]
- Coscas G., Quentel G., Pinon F., Soubrane G. Déchirure spontanée de l'épithélium pigmentaire dans la région maculaire. Bull Soc Ophtalmol Fr. 1982 Jun-Jul;82(6-7):815–820. [PubMed] [Google Scholar]
- Gass J. D. Pathogenesis of tears of the retinal pigment epithelium. Br J Ophthalmol. 1984 Aug;68(8):513–519. doi: 10.1136/bjo.68.8.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gass J. D. Retinal pigment epithelial rip during krypton red laser photocoagulation. Am J Ophthalmol. 1984 Dec 15;98(6):700–706. doi: 10.1016/0002-9394(84)90684-6. [DOI] [PubMed] [Google Scholar]
- Giovannini A., Scassellati-Sforzlini B., Lafaut B., Edeling J., D'Altobrando E., De Laey J. J. Indocyanine green angiography of retinal pigment epithelial tears. Acta Ophthalmol Scand. 1999 Feb;77(1):83–87. doi: 10.1034/j.1600-0420.1999.770119.x. [DOI] [PubMed] [Google Scholar]
- Green W. R., Enger C. Age-related macular degeneration histopathologic studies. The 1992 Lorenz E. Zimmerman Lecture. Ophthalmology. 1993 Oct;100(10):1519–1535. doi: 10.1016/s0161-6420(93)31466-1. [DOI] [PubMed] [Google Scholar]
- Green W. R., McDonnell P. J., Yeo J. H. Pathologic features of senile macular degeneration. Ophthalmology. 1985 May;92(5):615–627. [PubMed] [Google Scholar]
- Grossniklaus H. E., Hutchinson A. K., Capone A., Jr, Woolfson J., Lambert H. M. Clinicopathologic features of surgically excised choroidal neovascular membranes. Ophthalmology. 1994 Jun;101(6):1099–1111. doi: 10.1016/s0161-6420(13)31216-0. [DOI] [PubMed] [Google Scholar]
- Guyer D. R., Yannuzzi L. A., Slakter J. S., Sorenson J. A., Hope-Ross M., Orlock D. R. Digital indocyanine-green videoangiography of occult choroidal neovascularization. Ophthalmology. 1994 Oct;101(10):1727–1737. doi: 10.1016/s0161-6420(13)31433-x. [DOI] [PubMed] [Google Scholar]
- Hartnett M. E., Weiter J. J., Garsd A., Jalkh A. E. Classification of retinal pigment epithelial detachments associated with drusen. Graefes Arch Clin Exp Ophthalmol. 1992;230(1):11–19. doi: 10.1007/BF00166756. [DOI] [PubMed] [Google Scholar]
- Hoskin A., Bird A. C., Sehmi K. Tears of detached retinal pigment epithelium. Br J Ophthalmol. 1981 Jun;65(6):417–422. doi: 10.1136/bjo.65.6.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishan N. R., Chandra S. R., Stevens T. S. Diagnosis and pathogenesis of retinal pigment epithelial tears. Am J Ophthalmol. 1985 Nov 15;100(5):698–707. doi: 10.1016/0002-9394(85)90626-9. [DOI] [PubMed] [Google Scholar]
- Kuhn D., Meunier I., Soubrane G., Coscas G. Imaging of chorioretinal anastomoses in vascularized retinal pigment epithelium detachments. Arch Ophthalmol. 1995 Nov;113(11):1392–1398. doi: 10.1001/archopht.1995.01100110052025. [DOI] [PubMed] [Google Scholar]
- Lafaut B. A., Aisenbrey S., Vanden Broecke C., Bartz-Schmidt K. U. Clinicopathological correlation of deep retinal vascular anomalous complex in age related macular degeneration. Br J Ophthalmol. 2000 Nov;84(11):1269–1274. doi: 10.1136/bjo.84.11.1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lafaut B. A., Bartz-Schmidt K. U., Vanden Broecke C., Aisenbrey S., De Laey J. J., Heimann K. Clinicopathological correlation in exudative age related macular degeneration: histological differentiation between classic and occult choroidal neovascularisation. Br J Ophthalmol. 2000 Mar;84(3):239–243. doi: 10.1136/bjo.84.3.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarks S. H. New vessel formation beneath the retinal pigment epithelium in senile eyes. Br J Ophthalmol. 1973 Dec;57(12):951–965. doi: 10.1136/bjo.57.12.951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toth C. A., Pasquale A. C., 3rd, Graichen D. F. Clinicopathologic correlation of spontaneous retinal pigment epithelial tears with choroidal neovascular membranes in age-related macular degeneration. Ophthalmology. 1995 Feb;102(2):272–277. doi: 10.1016/s0161-6420(95)31045-7. [DOI] [PubMed] [Google Scholar]
- Tutein Nolthenius P. A., Deutman A. F. Rips of the retinal pigmentepithelium. Int Ophthalmol. 1985 Apr;8(1):19–23. doi: 10.1007/BF00136457. [DOI] [PubMed] [Google Scholar]
- Yannuzzi L. A., Hope-Ross M., Slakter J. S., Guyer D. R., Sorenson J. A., Ho A. C., Sperber D. E., Freund K. B., Orlock D. A. Analysis of vascularized pigment epithelial detachments using indocyanine green videoangiography. Retina. 1994;14(2):99–113. doi: 10.1097/00006982-199414020-00003. [DOI] [PubMed] [Google Scholar]
- Yeo J. H., Marcus S., Murphy R. P. Retinal pigment epithelial tears. Patterns and prognosis. Ophthalmology. 1988 Jan;95(1):8–13. [PubMed] [Google Scholar]