Abstract
AIM—To identify clinical factors associated with secondary elevated intraocular pressure (IOP) in eyes with iris malignant melanoma METHODS—A retrospective case series of 169 consecutive patients with microscopically confirmed iris malignant melanoma. The main outcome measure was the presence of tumour induced secondary elevated IOP. Cox proportional regression models were used to calculate the relation of clinical features to elevated IOP. RESULTS—Of 169 patients with microscopically proved iris melanoma, 50 (30%) presented with tumour induced secondary elevated IOP. The mean pressure in those eyes with elevated IOP at diagnosis was 33 mm Hg (median 31 mm Hg, range 23-65 mm Hg). The tumour configuration was nodular in 23 (46%) and diffuse in 27 (54%) with a mean base dimension of 7.4 mm and thickness of 2.0 mm. Invasion of the angle structures by melanoma seeds was visible for a mean of 7 clock hours (median 7, range 0-12 clock hours). The mechanism of elevated IOP was judged to be outflow obstruction from tumour invasion into the trabecular meshwork. There were no cases of neovascular glaucoma. The tumour was ultimately managed with enucleation in 30 patients (60%), local resection (iridectomy, iridocyclectomy, or iridocyclogoniectomy) in 11 (22%), and plaque radiotherapy in five (10%). In four cases (8%), observation of cytologically low grade tumour was the patient's preference. Using multivariate analysis, the clinical factors at initial evaluation associated with tumour induced secondary elevated IOP from iris melanoma included increasing extent of tumour seeding in the anterior chamber angle (p=0.01) and poor visual acuity at presentation (p=0.02). CONCLUSIONS—Microscopically confirmed iris melanoma demonstrates tumour related elevated IOP in 30% cases at the time of presentation, usually secondary to tumour involvement of the trabecular meshwork obstructing aqueous outflow. Enucleation is necessary in the majority of these patients (60%) as opposed to those cases without elevated intraocular pressure (18%).
Full Text
The Full Text of this article is available as a PDF (119.3 KB).
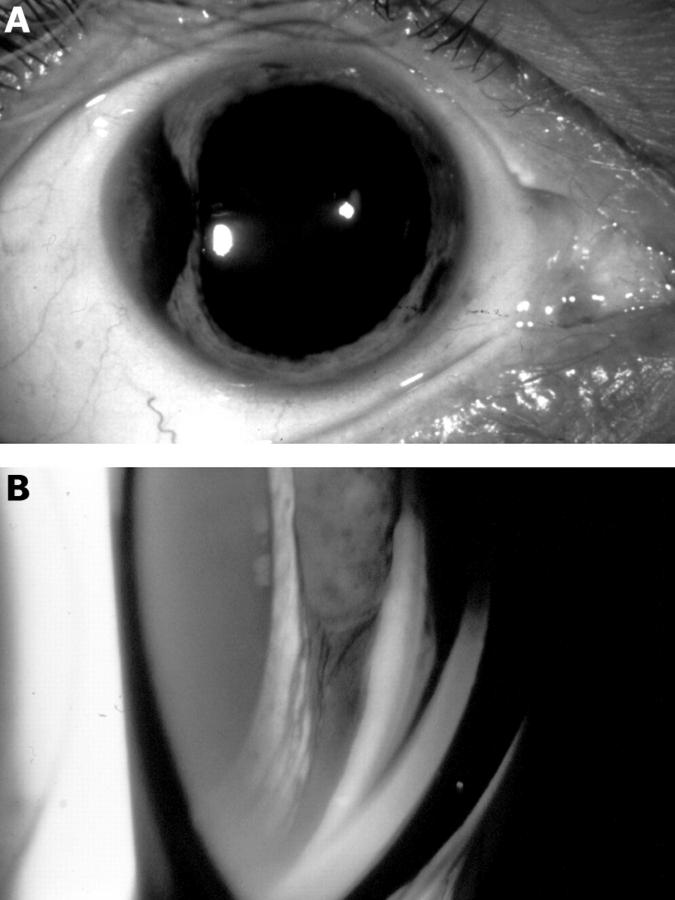
Figure 1 .
Iris melanoma with advanced tumour seeding in the angle and intraocular pressure of 36 mm Hg. (A) Slit lamp appearance of the fusiform pigmented mass involving the temporal portion of the iris. (B) Gonioscopic appearance of the mass with a tail of seeding into the angle for 12 clock hours, completely infiltrating the trabecular meshwork.
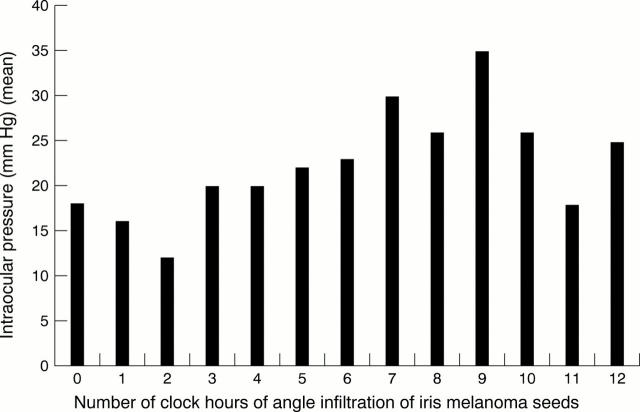
Figure 2 .
Relation of the clock hour extent of iris melanoma seeding in the anterior chamber angle with intraocular pressure in 169 consecutive cases.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arentsen J. J., Green W. R. Melanoma of the iris: report of 72 cases treated surgically. Ophthalmic Surg. 1975 Summer;6(2):23–37. [PubMed] [Google Scholar]
- Batioğlu F., Günalp I. Malignant melanomas of the iris. Jpn J Ophthalmol. 1998 Jul-Aug;42(4):281–285. doi: 10.1016/s0021-5155(98)00011-2. [DOI] [PubMed] [Google Scholar]
- Geisse L. J., Robertson D. M. Iris melanomas. Am J Ophthalmol. 1985 Jun 15;99(6):638–648. doi: 10.1016/s0002-9394(14)76028-3. [DOI] [PubMed] [Google Scholar]
- Grossniklaus H. E., Brown R. H., Stulting R. D., Blasberg R. D. Iris melanoma seeding through a trabeculectomy site. Arch Ophthalmol. 1990 Sep;108(9):1287–1290. doi: 10.1001/archopht.1990.01070110103033. [DOI] [PubMed] [Google Scholar]
- Jakobiec F. A., Silbert G. Are most iris "melanomas' really nevi? A clinicopathologic study of 189 lesions. Arch Ophthalmol. 1981 Dec;99(12):2117–2132. doi: 10.1001/archopht.1981.03930020993002. [DOI] [PubMed] [Google Scholar]
- Jensen O. A. Mlalignant melanomas of the human uvea. Recent follow-up of cases in Denmark, 1943-1952. Acta Ophthalmol (Copenh) 1970;48(6):1113–1128. doi: 10.1111/j.1755-3768.1970.tb06592.x. [DOI] [PubMed] [Google Scholar]
- RONES B., ZIMMERMAN L. E. The prognosis of primary tumors of the iris treated by iridectomy. AMA Arch Ophthalmol. 1958 Aug;60(2):193–205. doi: 10.1001/archopht.1958.00940080207003. [DOI] [PubMed] [Google Scholar]
- Shields C. L., Shields J. A., Baez K., Cater J. R., De Potter P. Optic nerve invasion of retinoblastoma. Metastatic potential and clinical risk factors. Cancer. 1994 Feb 1;73(3):692–698. doi: 10.1002/1097-0142(19940201)73:3<692::aid-cncr2820730331>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- Shields C. L., Shields J. A., De Potter P., Singh A. D., Hernandez C., Brady L. W. Treatment of non-resectable malignant iris tumours with custom designed plaque radiotherapy. Br J Ophthalmol. 1995 Apr;79(4):306–312. doi: 10.1136/bjo.79.4.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shields C. L., Shields J. A., Shields M. B., Augsburger J. J. Prevalence and mechanisms of secondary intraocular pressure elevation in eyes with intraocular tumors. Ophthalmology. 1987 Jul;94(7):839–846. doi: 10.1016/s0161-6420(87)33537-7. [DOI] [PubMed] [Google Scholar]
- Shields J. A., Sanborn G. E., Augsburger J. J. The differential diagnosis of malignant melanoma of the iris. A clinical study of 200 patients. Ophthalmology. 1983 Jun;90(6):716–720. doi: 10.1016/s0161-6420(83)34500-0. [DOI] [PubMed] [Google Scholar]
- Shields J. A., Shields C. L. Surgical approach to lamellar sclerouvectomy for posterior uveal melanomas: the 1986 Schoenberg lecture. Ophthalmic Surg. 1988 Nov;19(11):774–780. doi: 10.3928/0090-4481-19881101-04. [DOI] [PubMed] [Google Scholar]
- Sunba M. S., Rahi A. H., Morgan G. Tumors of the anterior uvea. I. Metastasizing malignant melanoma of the iris. Arch Ophthalmol. 1980 Jan;98(1):82–85. doi: 10.1001/archopht.1980.01020030084004. [DOI] [PubMed] [Google Scholar]
- Territo C., Shields C. L., Shields J. A., Augsburger J. J., Schroeder R. P. Natural course of melanocytic tumors of the iris. Ophthalmology. 1988 Sep;95(9):1251–1255. doi: 10.1016/s0161-6420(88)33022-8. [DOI] [PubMed] [Google Scholar]