Abstract
AIM—Ocular involvement in giant cell arteritis (GCA) is an ophthalmic emergency which, if untreated, can progress to permanent blindness. There is little evidence in the literature to support current protocols for the acute treatment of GCA with steroids. The authors sought to review the effects of intravenous and oral steroids in GCA. METHODS—This retrospective study reviewed the records of 100 consecutive patients with biopsy proved giant cell arteritis. 73 patients with visual loss who were treated at the Royal Victorian Eye and Ear Hospital (RVEEH) and St Vincent's Hospital were included in the final series. The authors studied the management of the patients in the first week after presentation, analysing types of treatment, dose, effect on visual acuity, and complications. RESULTS—All the patients except one had visual loss due to anterior ischaemic optic neuropathy (AION). 17 patients (23%) had bilateral eye involvement. Visual acuity improved in 21 of 73 patients (29%) by a mean of two Snellen chart lines after commencement of steroids. There was an increased likelihood of improved vision in the group who had intravenous steroids (40%) compared with those who received oral steroids (13%). In all except four patients (95%) vision remained stable at 1 month review. CONCLUSIONS—Prompt treatment of GCA with steroids leads to improvement of visual acuity in a significant number of cases. Intravenous steroids may offer a greater prospect of improvement compared with oral steroids. A prospective trial comparing intravenous with oral steroids is needed to validate these findings and would not expose elderly patients to unacceptable risks.
Full Text
The Full Text of this article is available as a PDF (133.8 KB).
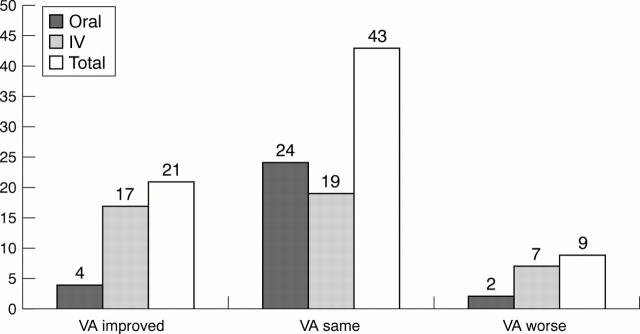
Figure 1 .
Change in visual acuity after treatment with intravenous or oral steroids.
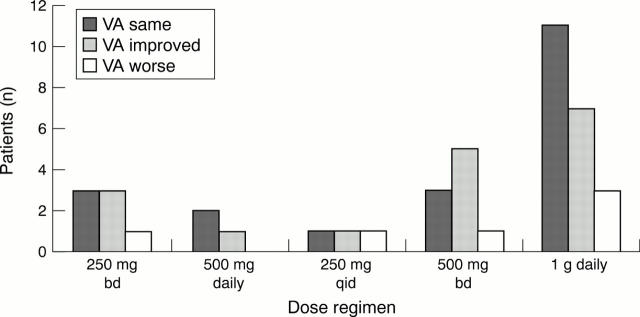
Figure 2 .
No trends are evident when comparing different intravenous steroid regimens as to which is more effective in treatment of GCA in terms of visual acuity outcome (p=0.93)
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Andersson R., Malmvall B. E., Bengtsson B. A. Long-term corticosteroid treatment in giant cell arteritis. Acta Med Scand. 1986;220(5):465–469. doi: 10.1111/j.0954-6820.1986.tb02796.x. [DOI] [PubMed] [Google Scholar]
- Bengtsson B. A., Malmvall B. E. The epidemiology of giant cell arteritis including temporal arteritis and polymyalgia rheumatica. Incidences of different clinical presentations and eye complications. Arthritis Rheum. 1981 Jul;24(7):899–904. doi: 10.1002/art.1780240706. [DOI] [PubMed] [Google Scholar]
- Bengtsson B. A., Malmvall B. E. The epidemiology of giant cell arteritis including temporal arteritis and polymyalgia rheumatica. Incidences of different clinical presentations and eye complications. Arthritis Rheum. 1981 Jul;24(7):899–904. doi: 10.1002/art.1780240706. [DOI] [PubMed] [Google Scholar]
- CULLEN J. F. OCCULT TEMPORAL ARTERITIS. Trans Ophthalmol Soc U K. 1963;83:725–736. [PubMed] [Google Scholar]
- Calamia K. T., Hunder G. G. Giant cell arteritis (temporal arteritis) presenting as fever of undetermined origin. Arthritis Rheum. 1981 Nov;24(11):1414–1418. doi: 10.1002/art.1780241113. [DOI] [PubMed] [Google Scholar]
- Clearkin L. G. IV steroids for central retinal artery occlusion in giant-cell arteritis. Ophthalmology. 1992 Oct;99(10):1482–1484. doi: 10.1016/s0161-6420(92)31777-4. [DOI] [PubMed] [Google Scholar]
- Cornblath W. T., Eggenberger E. R. Progressive visual loss from giant cell arteritis despite high-dose intravenous methylprednisolone. Ophthalmology. 1997 May;104(5):854–858. doi: 10.1016/s0161-6420(97)30222-x. [DOI] [PubMed] [Google Scholar]
- Diamond J. P. IV steroid treatment of giant cell arteritis. Ophthalmology. 1993 Mar;100(3):291–292. [PubMed] [Google Scholar]
- Ferris J., Lamb R. Polymyalgia rheumatica and giant cell arteritis. High dose corticosteroids are recommended. BMJ. 1995 Aug 12;311(7002):455–455. doi: 10.1136/bmj.311.7002.455a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gambertoglio J. G., Amend W. J., Jr, Benet L. Z. Pharmacokinetics and bioavailability of prednisone and prednisolone in healthy volunteers and patients: a review. J Pharmacokinet Biopharm. 1980 Feb;8(1):1–52. doi: 10.1007/BF01059447. [DOI] [PubMed] [Google Scholar]
- González-Gay M. A., Blanco R., Rodríguez-Valverde V., Martínez-Taboada V. M., Delgado-Rodriguez M., Figueroa M., Uriarte E. Permanent visual loss and cerebrovascular accidents in giant cell arteritis: predictors and response to treatment. Arthritis Rheum. 1998 Aug;41(8):1497–1504. doi: 10.1002/1529-0131(199808)41:8<1497::AID-ART22>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- Graham E., Holland A., Avery A., Russell R. W. Prognosis in giant-cell arteritis. Br Med J (Clin Res Ed) 1981 Jan 24;282(6260):269–271. doi: 10.1136/bmj.282.6260.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayreh S. S. Anterior ischaemic optic neuropathy. Differentiation of arteritic from non-arteritic type and its management. Eye (Lond) 1990;4(Pt 1):25–41. doi: 10.1038/eye.1990.4. [DOI] [PubMed] [Google Scholar]
- Hayreh S. S. Ophthalmic features of giant cell arteritis. Baillieres Clin Rheumatol. 1991 Dec;5(3):431–459. doi: 10.1016/s0950-3579(05)80064-0. [DOI] [PubMed] [Google Scholar]
- Hayreh S. S., Podhajsky P. A., Zimmerman B. Ocular manifestations of giant cell arteritis. Am J Ophthalmol. 1998 Apr;125(4):509–520. doi: 10.1016/s0002-9394(99)80192-5. [DOI] [PubMed] [Google Scholar]
- Hugod C., Scheibel M. Temporal arteritis--progressive affection of vision during high-level corticosteroid therapy. A case report. Acta Med Scand. 1979;205(5):445–446. doi: 10.1111/j.0954-6820.1979.tb06080.x. [DOI] [PubMed] [Google Scholar]
- Hunder G. G. Giant cell (temporal) arteritis. Rheum Dis Clin North Am. 1990 May;16(2):399–409. [PubMed] [Google Scholar]
- Hwang J. M., Girkin C. A., Perry J. D., Lai J. C., Miller N. R., Hellmann D. B. Bilateral ocular ischemic syndrome secondary to giant cell arteritis progressing despite corticosteroid treatment. Am J Ophthalmol. 1999 Jan;127(1):102–104. doi: 10.1016/s0002-9394(98)00313-4. [DOI] [PubMed] [Google Scholar]
- Liu G. T., Glaser J. S., Schatz N. J., Smith J. L. Visual morbidity in giant cell arteritis. Clinical characteristics and prognosis for vision. Ophthalmology. 1994 Nov;101(11):1779–1785. doi: 10.1016/s0161-6420(94)31102-x. [DOI] [PubMed] [Google Scholar]
- Myles A. B. Prognosis of polymyalgia rheumatica and giant cell arteritis. Baillieres Clin Rheumatol. 1991 Dec;5(3):493–503. doi: 10.1016/s0950-3579(05)80068-8. [DOI] [PubMed] [Google Scholar]
- Paice E. W. Giant cell arteritis: difficult decisions in diagnosis, investigation and treatment. Postgrad Med J. 1989 Oct;65(768):743–747. doi: 10.1136/pgmj.65.768.743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Postel E. A., Pollock S. C. Recovery of vision in a 47-year-old man with fulminant giant cell arteritis. J Clin Neuroophthalmol. 1993 Dec;13(4):262–270. [PubMed] [Google Scholar]
- WHITFIELD A. G., BATEMAN M., COOKE W. T. TEMPORAL ARTERITIS. Br J Ophthalmol. 1963 Sep;47:555–566. doi: 10.1136/bjo.47.9.555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wind B. E. Temporal arteritis. Aggressive treatment prevents visual complications. Postgrad Med. 1992 May 1;91(6):337-8, 341-2. doi: 10.1080/00325481.1992.11701333. [DOI] [PubMed] [Google Scholar]
- Wray S. H. Optic neuritis: guidelines. Curr Opin Neurol. 1995 Feb;8(1):72–76. doi: 10.1097/00019052-199502000-00012. [DOI] [PubMed] [Google Scholar]