Abstract
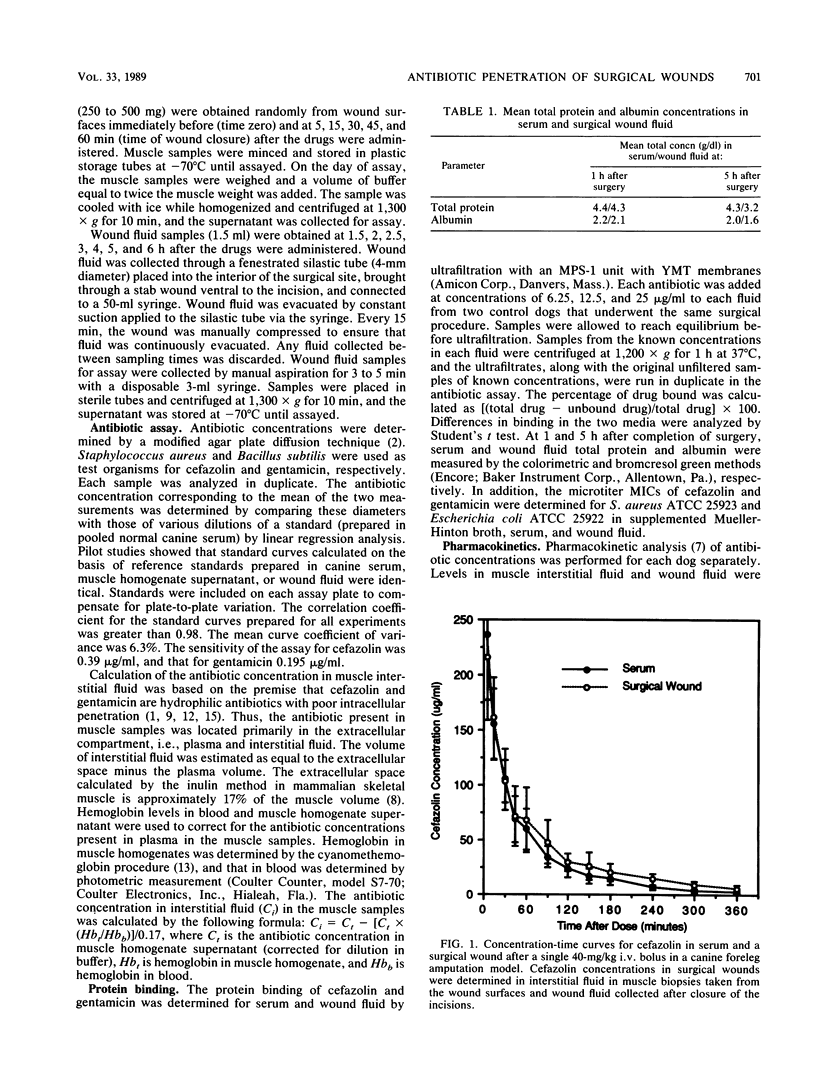
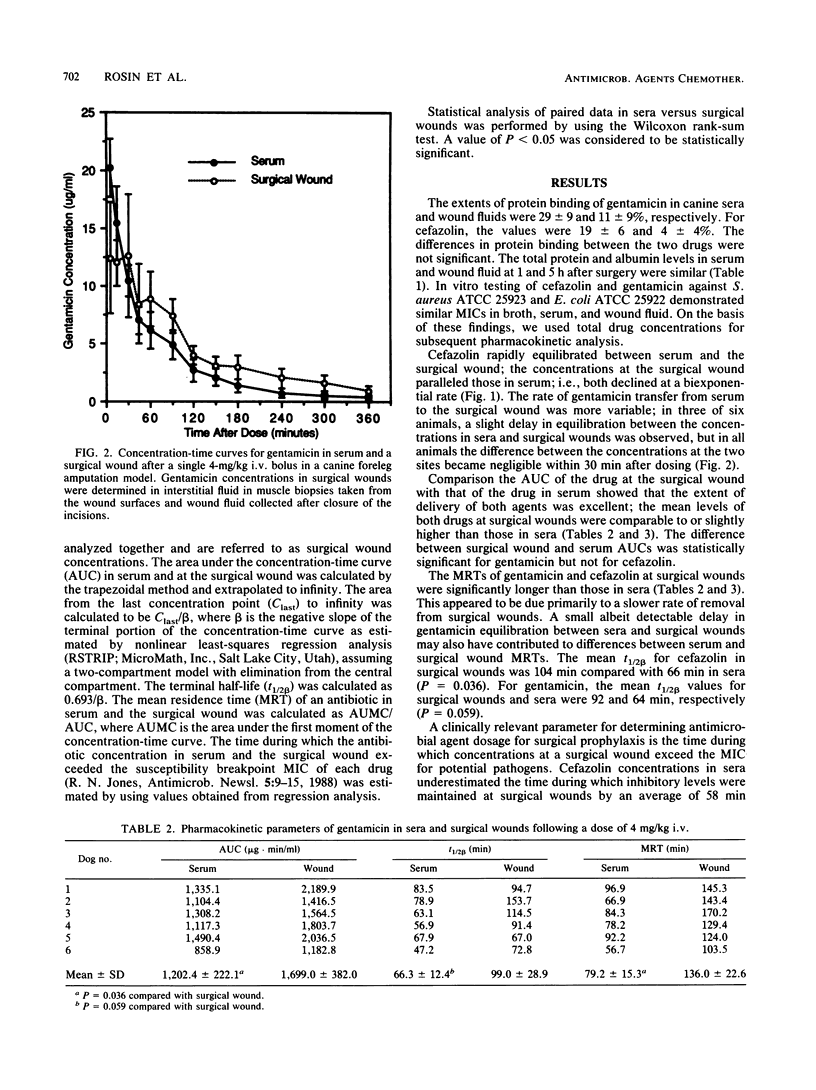
The dose and timing of antimicrobial agents given for surgical wound prophylaxis should be based on the concentration-time profile of the drug in tissue at the site of contamination. However, concentrations of antimicrobial agents in surgical wounds are difficult to determine accurately. Since a surgical wound is a unique extravascular compartment with increased vascular permeability and a high surface area/volume ratio, antibiotic concentrations in sera and surgical wounds should be similar. To test this hypothesis, the pharmacokinetics of single intravenous doses of cefazolin (40 mg/kg) and gentamicin (4 mg/kg) in sera and surgical wounds in a clinically relevant surgical model using dogs were compared. Drug concentrations were determined in interstitial fluid in muscle biopsies taken randomly from wound surfaces and serial wound fluid samples collected after the incisions were closed. Protein binding of cefazolin and gentamicin in sera and wound fluids was low (less than or equal to 29 +/- 9%) in this canine model. Cefazolin and gentamicin equilibrated rapidly (less than or equal to 30 min) between serum and the surgical wound, and concentrations in the two sites declined in parallel. Values for the area under the concentration-time curve, mean residence time, and terminal half-life in serum and the surgical site for each drug were similar. Cefazolin concentrations in serum underestimated the time during which concentrations in surgical wounds exceeded the susceptibility breakpoint MIC for important pathogens by an average of 58 min (range, 26 to 109 min; P = 0.036); for gentamicin, the underestimation averaged 30 min (range, 10 to 60 min; P = 0.036). These data support the concept that the concentration-time profiles of antimicrobial agents in serum may prove valuable clinically as guides to determining the and timing of antibiotic administration necessary for effective antimicrobial prophylaxis in surgery. Further studies are needed to determine the surgical wound pharmacokinetics of highly protein-bound antibodies.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alexander J. W., Sykes N. S., Mitchell M. M., Fisher M. W. Concentration of selected intravenously administered antibiotics in experimental surgical wounds. J Trauma. 1973 May;13(5):423–434. doi: 10.1097/00005373-197305000-00004. [DOI] [PubMed] [Google Scholar]
- Bennett J. V., Brodie J. L., Benner E. J., Kirby W. M. Simplified, accurate method for antibiotic assay of clinical specimens. Appl Microbiol. 1966 Mar;14(2):170–177. doi: 10.1128/am.14.2.170-177.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cars O. Tissue distribution of ampicillin: assays in muscle tissue and subcutaneous tissue cage fluid from normal and nephrectomized rabbits. Scand J Infect Dis. 1981;13(4):283–289. doi: 10.3109/inf.1981.13.issue-4.09. [DOI] [PubMed] [Google Scholar]
- Chisholm G. D., Waterworth P. M., Calnan J. S., Garrod L. P. Concentration of antibacterial agents in interstitial tissue fluid. Br Med J. 1973 Mar 10;1(5853):569–573. doi: 10.1136/bmj.1.5853.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Condon R. E., Bartlett J. G., Nichols R. L., Schulte W. J., Gorbach S. L., Ochi S. Preoperative prophylactic cephalothin fails to control septic complications of colorectal operations: results of controlled clinical trial. A Veterans Administration cooperative study. Am J Surg. 1979 Jan;137(1):68–74. doi: 10.1016/0002-9610(79)90013-8. [DOI] [PubMed] [Google Scholar]
- Frongillo R. F., Galuppo L., Moretti A. Suction skin blister, skin window, and skin chamber techniques to determine extravascular passage of cefotaxime in humans. Antimicrob Agents Chemother. 1981 Jan;19(1):22–28. doi: 10.1128/aac.19.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heffron J. J., Hegarty P. V. Evidence for a relationship between ATP hydrolysis and changes in extracellular space and fibre diameter during rigor development in skeletal muscle. Comp Biochem Physiol A Comp Physiol. 1974 Sep 1;49(1A):43–56. doi: 10.1016/0300-9629(74)90540-4. [DOI] [PubMed] [Google Scholar]
- Johnson J. D., Hand W. L., Francis J. B., King-Thompson N., Corwin R. W. Antibiotic uptake by alveolar macrophages. J Lab Clin Med. 1980 Mar;95(3):429–439. [PubMed] [Google Scholar]
- Kaiser A. B. Antimicrobial prophylaxis in surgery. N Engl J Med. 1986 Oct 30;315(18):1129–1138. doi: 10.1056/NEJM198610303151805. [DOI] [PubMed] [Google Scholar]
- Kornguth M. L., Kunin C. M. Uptake of antibiotics by human erythrocytes. J Infect Dis. 1976 Feb;133(2):175–184. doi: 10.1093/infdis/133.2.175. [DOI] [PubMed] [Google Scholar]
- Polk H. C., Jr, Trachtenberg L., Finn M. P. Antibiotic activity in surgical incisions. The basis of prophylaxis in selected operations. JAMA. 1980 Sep 19;244(12):1353–1354. [PubMed] [Google Scholar]
- Prokesch R. C., Hand W. L. Antibiotic entry into human polymorphonuclear leukocytes. Antimicrob Agents Chemother. 1982 Mar;21(3):373–380. doi: 10.1128/aac.21.3.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan D. M., Cars O. Antibiotic assays in muscle: are conventional tissue levels misleading as indicator of the antibacterial activity? Scand J Infect Dis. 1980;12(4):307–309. doi: 10.3109/inf.1980.12.issue-4.12. [DOI] [PubMed] [Google Scholar]
- Shyu W. C., Quintiliani R., Nightingale C. H., Dudley M. N. Effect of protein binding on drug penetration into blister fluid. Antimicrob Agents Chemother. 1988 Jan;32(1):128–130. doi: 10.1128/aac.32.1.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Etta L. L., Peterson L. R., Fasching C. E., Gerding D. N. Effect of the ratio of surface area to volume on the penetration of antibiotics in to extravascular spaces in an in vitro model. J Infect Dis. 1982 Sep;146(3):423–428. doi: 10.1093/infdis/146.3.423. [DOI] [PubMed] [Google Scholar]
- Waterman N. G., Kastan L. B. Interstitial fluid and serum antibiotic concentrations. Arch Surg. 1972 Aug;105(2):192–196. doi: 10.1001/archsurg.1972.04180080046008. [DOI] [PubMed] [Google Scholar]
- Wise R., Gillett A. P., Cadge B., Durham S. R., Baker S. The influence of protein binding upon tissue fluid levels of six beta-lactam antibiotics. J Infect Dis. 1980 Jul;142(1):77–82. doi: 10.1093/infdis/142.1.77. [DOI] [PubMed] [Google Scholar]


