Abstract
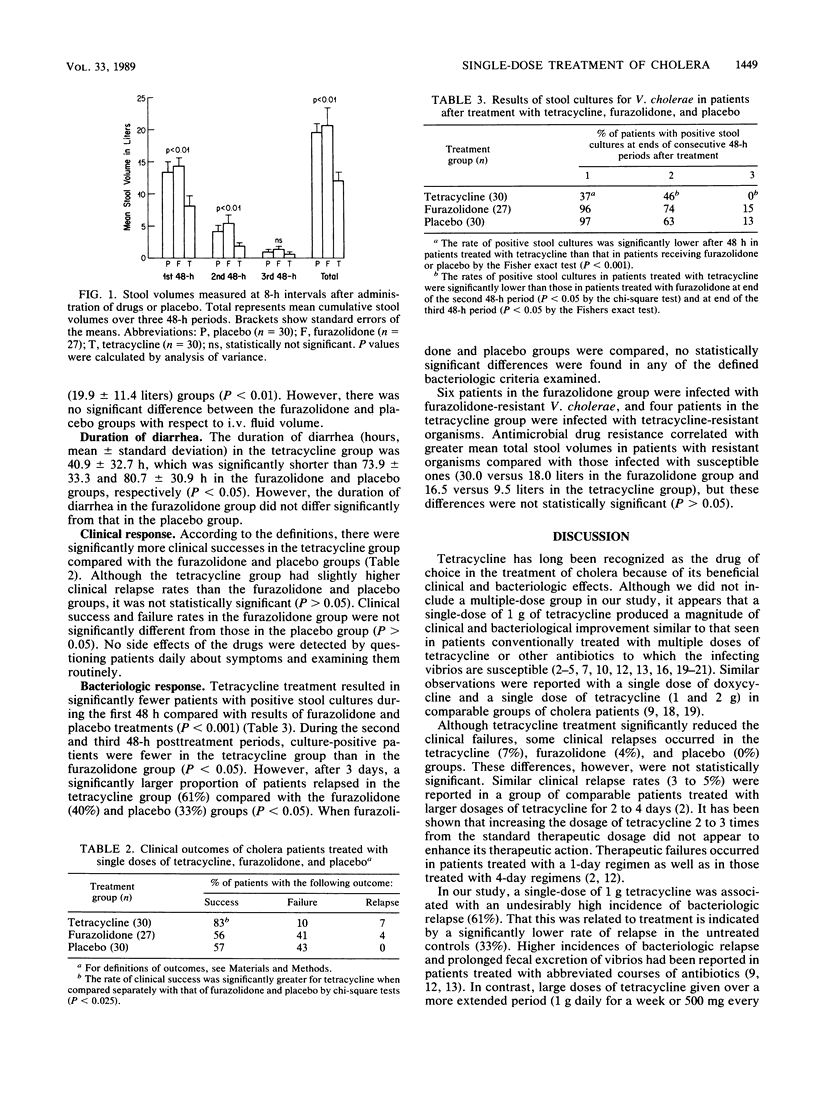
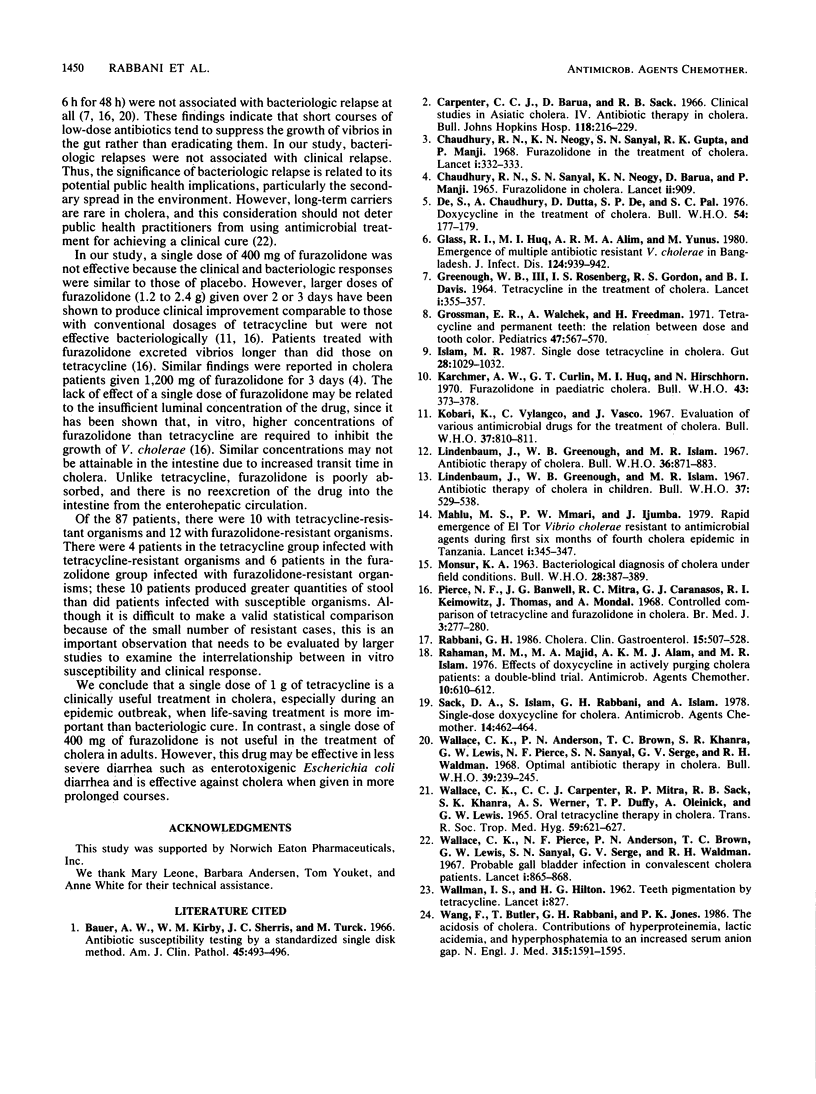
To evaluate single doses of 400 mg of furazolidone and 1 g of tetracycline given orally to patients with diarrhea due to Vibrio cholerae, we studied 87 adults in a randomized, double-blind, placebo-controlled trial. All patients received intravenous fluids for rehydration and no other drugs. The total volumes of stool (mean +/- standard deviation) during a 6-day period after treatment were significantly smaller in the tetracycline group (10.5 +/- 8.6 liters) than in the furazolidone group (20.9 +/- 15.9 liters) and the placebo group (19.1 +/- 10.5 liters) (P less than 0.01). The duration of diarrhea and volumes of intravenous fluids were also significantly reduced in the tetracycline group (P less than 0.05). However, there were no differences between the furazolidone and the placebo groups with regard to stool volume, intravenous fluid, and duration of diarrhea. Within 48 h of treatment, tetracycline significantly reduced the number of patients with positive stool cultures for V. cholerae (37%) compared with furazolidone treatment (96%) and the placebo (97%) (P less than 0.001). Although the tetracycline group had a significantly higher incidence (61%) of bacteriologic relapse (negative stool cultures on days 2 and 3, followed by positive cultures afterward) compared with that in the furazolidone group (40%) and the placebo group (33%), this was not associated with clinical relapse. There were no differences between the furazolidone and placebo groups with regard to any of the bacteriologic responses examined. These data indicate that a single dose of 1 g of tetracycline is effective in the treatment of cholera, but it is asymptomatic bacteriologic relapse. A single dose of 400 mg of furazolidone is not therapeutically effective in cholera.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bauer A. W., Kirby W. M., Sherris J. C., Turck M. Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol. 1966 Apr;45(4):493–496. [PubMed] [Google Scholar]
- Chaudhuri R. N., Neogy K. N., Sanyal S. N., Gupta R. K., Manji P. Furazolidone in the treatment of cholera. Lancet. 1968 Feb 17;1(7538):332–333. doi: 10.1016/s0140-6736(68)90796-4. [DOI] [PubMed] [Google Scholar]
- De S., Chaudhuri A., Dutta P., Dutta D., De S. P., Pal S. C. Doxycycline in the treatment of cholera. Bull World Health Organ. 1976;54(2):177–179. [PMC free article] [PubMed] [Google Scholar]
- GREENOUGH W. B., 3rd, GORDON R. S., Jr, ROSENBERG I. S., DAVIES B. I., BENENSON A. S. TETRACYCLINE IN THE TREATMENT OF CHOLERA. Lancet. 1964 Feb 15;1(7329):355–357. doi: 10.1016/s0140-6736(64)92099-9. [DOI] [PubMed] [Google Scholar]
- Glass R. I., Huq I., Alim A. R., Yunus M. Emergence of multiply antibiotic-resistant Vibrio cholerae in Bangladesh. J Infect Dis. 1980 Dec;142(6):939–942. doi: 10.1093/infdis/142.6.939. [DOI] [PubMed] [Google Scholar]
- Grossman E. R., Walchek A., Freedman H. Tetracyclines and permanent teeth: the relation between dose and tooth color. Pediatrics. 1971 Mar;47(3):567–570. [PubMed] [Google Scholar]
- Islam M. R. Single dose tetracycline in cholera. Gut. 1987 Aug;28(8):1029–1032. doi: 10.1136/gut.28.8.1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karchmer A. W., Curlin G. T., Huq M. I., Hirschhorn N. Furazolidone in paediatric cholera. Bull World Health Organ. 1970;43(3):373–378. [PMC free article] [PubMed] [Google Scholar]
- Kobari K., Uylangco C., Vasco J. Evaluation of various antimicrobial drugs for the treatment of cholera. Bull World Health Organ. 1967;37(5):810–811. [PMC free article] [PubMed] [Google Scholar]
- Lindenbaum J., Greenough W. B., Islam M. R. Antibiotic therapy of cholera in children. Bull World Health Organ. 1967;37(4):529–538. [PMC free article] [PubMed] [Google Scholar]
- Lindenbaum J., Greenough W. B., Islam M. R. Antibiotic therapy of cholera. Bull World Health Organ. 1967;36(6):871–883. [PMC free article] [PubMed] [Google Scholar]
- Mhalu F. S., Mmari P. W., Ijumba J. Rapid emergence of El Tor Vibrio cholerae resistant to antimicrobial agents during first six months of fourth cholera epidemic in Tanzania. Lancet. 1979 Feb 17;1(8112):345–347. doi: 10.1016/s0140-6736(79)92889-7. [DOI] [PubMed] [Google Scholar]
- Pierce N. F., Banwell J. G., Mitra R. C., Caranasos G. J., Keimowitz R. I., Thomas J., Mondal A. Controlled comparison of tetracycline and furazolidone in cholera. Br Med J. 1968 Aug 3;3(5613):277–280. doi: 10.1136/bmj.3.5613.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabbani G. H. Cholera. Clin Gastroenterol. 1986 Jul;15(3):507–528. [PubMed] [Google Scholar]
- Rahaman M. M., Majid M. A., Alam AKMJ, Islam M. R. Effects of doxycycline in actively purging cholera patients: a double-blind clinical trial. Antimicrob Agents Chemother. 1976 Oct;10(4):610–612. doi: 10.1128/aac.10.4.610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts H. J. Amphetamine. Lancet. 1965 Oct 30;2(7418):909–910. doi: 10.1016/s0140-6736(65)92549-3. [DOI] [PubMed] [Google Scholar]
- Sack D. A., Islam S., Rabbani H., Islam A. Single-dose doxycycline for cholera. Antimicrob Agents Chemother. 1978 Sep;14(3):462–464. doi: 10.1128/aac.14.3.462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WALLMAN I. S., HILTON H. B. Teeth pigmented by tetracycline. Lancet. 1962 Apr 21;1(7234):827–829. doi: 10.1016/s0140-6736(62)91840-8. [DOI] [PubMed] [Google Scholar]
- Wallace C. K., Anderson P. N., Brown T. C., Khanra S. R., Lewis G. W., Pierce N. F., Sanyal S. N., Segre G. V., Waldman R. H. Optimal antibiotic therapy in cholera. Bull World Health Organ. 1968;39(2):239–245. [PMC free article] [PubMed] [Google Scholar]
- Wallace C. K., Anderson P. N., Lewis G. W., Segre G. V., Pierce N. F., Brown T. C., Sanyal S. N., Waldman R. H. Probable gallbladder infection in convalescent cholera patients. Lancet. 1967 Apr 22;1(7495):865–868. doi: 10.1016/s0140-6736(67)91427-4. [DOI] [PubMed] [Google Scholar]
- Wang F., Butler T., Rabbani G. H., Jones P. K. The acidosis of cholera. Contributions of hyperproteinemia, lactic acidemia, and hyperphosphatemia to an increased serum anion gap. N Engl J Med. 1986 Dec 18;315(25):1591–1595. doi: 10.1056/NEJM198612183152506. [DOI] [PubMed] [Google Scholar]


