Abstract
Background—Peripheral arthropathy is a well-recognised complication of inflammatory bowel disease (IBD). Little is known of its natural history, but a variety of joint involvement has been described, from large joint pauciarticular arthropathy to a rheumatoid pattern polyarthropathy. Aims—To classify the peripheral arthropathies according to pattern of articular involvement, and study their natural history and clinical associations. Methods—The case notes of all patients attending the Oxford IBD clinic were reviewed, and information on general disease characteristics, extraintestinal features, and arthropathy extracted. This was confirmed by direct patient interview using questionnaires at routine follow up. Patients with recorded joint swelling or effusion were classified as type 1 (pauciarticular) if less than five joints were involved and type 2 (polyarticular) if five or more were involved. Patients without evidence of swelling were classified as arthralgia. Results—In total, 976 patients with ulcerative colitis (UC) and 483 with Crohn's disease (CD) were reviewed. Type 1 occurred in 3.6% of patients with UC (83% acute and self-limiting) and in 6.0% of those with CD (79% self-limiting); 83% and 76%, respectively, were associated with relapsing IBD. Type 2 occurred in 2.5% of patients with UC and 4.0% of those with CD; 87% and 89%, respectively, caused persistent symptoms whereas only 29% and 42%, respectively, were associated with relapsing IBD. Conclusion—Enteropathic peripheral arthropathy without axial involvement can be subdivided into a pauciarticular, large joint arthropathy, and a bilateral symmetrical polyarthropathy, each being distinguished by its articular distribution and natural history.
Keywords: ulcerative colitis; Crohn's disease; peripheral arthropathy; extraintestinal manifestations
Full Text
The Full Text of this article is available as a PDF (118.3 KB).
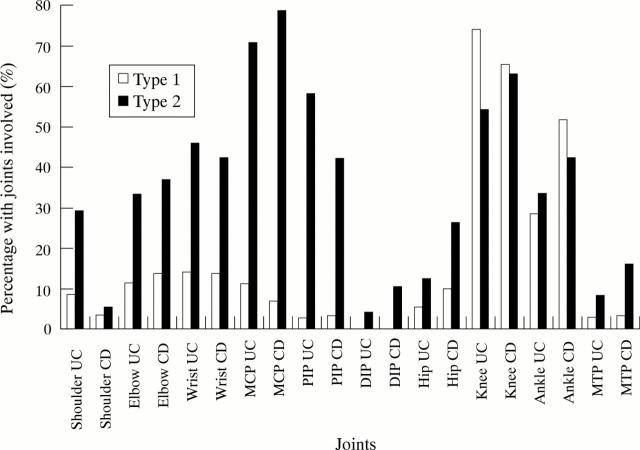
Figure 1 .
Articular distribution of peripheral arthropathies in inflammatory bowel disease. UC, ulcerative colitis; CD, Crohn's disease; MCP, metacarpophalangealjoint; PIP, proximal interphalangeal joint; DIP, distal interphalangeal joint; MTP, metatarsophalangeal joint.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brewerton D. A., Caffrey M., Nicholls A., Walters D., James D. C. HL-A 27 and arthropathies associated with ulcerative colitis and psoriasis. Lancet. 1974 May 18;1(7864):956–958. doi: 10.1016/s0140-6736(74)91262-8. [DOI] [PubMed] [Google Scholar]
- Brewerton D. A., Caffrey M., Nicholls A., Walters D., Oates J. K., James D. C. Reiter's disease and HL-A 27. Lancet. 1973 Nov 3;302(7836):996–998. doi: 10.1016/s0140-6736(73)91091-x. [DOI] [PubMed] [Google Scholar]
- Brown M. A., Pile K. D., Kennedy L. G., Calin A., Darke C., Bell J., Wordsworth B. P., Cornélis F. HLA class I associations of ankylosing spondylitis in the white population in the United Kingdom. Ann Rheum Dis. 1996 Apr;55(4):268–270. doi: 10.1136/ard.55.4.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calin A., Fries J. F. An "experimental" epidemic of Reiter's syndrome revisited. Follow-up evidence on genetic and environmental factors. Ann Intern Med. 1976 May;84(5):564–566. doi: 10.7326/0003-4819-84-5-564. [DOI] [PubMed] [Google Scholar]
- Dekker-Saeys B. J., Meuwissen S. G., Van Den Berg-Loonen E. M., De Haas W. H., Agenant D., Tytgat G. N. Ankylosing spondylitis and inflammatory bowel disease. II. Prevalence of peripheral arthritis, sacroiliitis, and ankylosing spondylitis in patients suffering from inflammatory bowel disease. Ann Rheum Dis. 1978 Feb;37(1):33–35. doi: 10.1136/ard.37.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EDWARDS F. C., TRUELOVE S. C. THE COURSE AND PROGNOSIS OF ULCERATIVE COLITIS. III. COMPLICATIONS. Gut. 1964 Feb;5:1–22. doi: 10.1136/gut.5.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enlow R. W., Bias W. B., Arnett F. C. The spondylitis of inflammatory bowel disease. Evidence for a non-HLA linked axial arthropathy. Arthritis Rheum. 1980 Dec;23(12):1359–1365. doi: 10.1002/art.1780231205. [DOI] [PubMed] [Google Scholar]
- Gravallese E. M., Kantrowitz F. G. Arthritic manifestations of inflammatory bowel disease. Am J Gastroenterol. 1988 Jul;83(7):703–709. [PubMed] [Google Scholar]
- Greenstein A. J., Janowitz H. D., Sachar D. B. The extra-intestinal complications of Crohn's disease and ulcerative colitis: a study of 700 patients. Medicine (Baltimore) 1976 Sep;55(5):401–412. doi: 10.1097/00005792-197609000-00004. [DOI] [PubMed] [Google Scholar]
- Leirisalo-Repo M. Enteropathic arthritis, Whipple's disease, juvenile spondyloarthropathy, uveitis, and SAPHO syndrome. Curr Opin Rheumatol. 1995 Jul;7(4):284–289. doi: 10.1097/00002281-199507000-00004. [DOI] [PubMed] [Google Scholar]
- Mallas E. G., Mackintosh P., Asquith P., Cooke W. T. Histocompatibility antigens in inflammatory bowel disease. Their clinical significance and their association with arthropathy with special reference to HLA-B27 (W27). Gut. 1976 Nov;17(11):906–910. doi: 10.1136/gut.17.11.906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mielants H., Veys E. M., Cuvelier C., De Vos M., Goemaere S., De Clercq L., Schatteman L., Gyselbrecht L., Elewaut D. The evolution of spondyloarthropathies in relation to gut histology. III. Relation between gut and joint. J Rheumatol. 1995 Dec;22(12):2279–2284. [PubMed] [Google Scholar]
- Mielants H., Veys E. M., De Vos M., Cuvelier C., Goemaere S., De Clercq L., Schatteman L., Elewaut D. The evolution of spondyloarthropathies in relation to gut histology. I. Clinical aspects. J Rheumatol. 1995 Dec;22(12):2266–2272. [PubMed] [Google Scholar]
- Mielants H., Veys E. M. HLA-B27 related arthritis and bowel inflammation. Part 1. Sulfasalazine (salazopyrin) in HLA-B27 related reactive arthritis. J Rheumatol. 1985 Apr;12(2):287–293. [PubMed] [Google Scholar]
- Russell A. S., Percy J. S., Schlaut J., Sartor V. E., Goodhart J. M., Sherbaniuk R. W., Kidd E. G. Transplantation antigens in Crohn's disease: Linkage of associated ankylosing spondylitis with HL-Aw27. Am J Dig Dis. 1975 Apr;20(4):359–361. doi: 10.1007/BF01237793. [DOI] [PubMed] [Google Scholar]
- Satsangi J., Grootscholten C., Holt H., Jewell D. P. Clinical patterns of familial inflammatory bowel disease. Gut. 1996 May;38(5):738–741. doi: 10.1136/gut.38.5.738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satsangi J., Welsh K. I., Bunce M., Julier C., Farrant J. M., Bell J. I., Jewell D. P. Contribution of genes of the major histocompatibility complex to susceptibility and disease phenotype in inflammatory bowel disease. Lancet. 1996 May 4;347(9010):1212–1217. doi: 10.1016/s0140-6736(96)90734-5. [DOI] [PubMed] [Google Scholar]
- WRIGHT V., WATKINSON G. THE ARTHRITIS OF ULCERATIVE COLITIS. Br Med J. 1965 Sep 18;2(5463):670–675. doi: 10.1136/bmj.2.5463.670. [DOI] [PMC free article] [PubMed] [Google Scholar]