Abstract
Aims—To compare the incidence of oesophageal abnormalities and their correlation with chest pain in patients with normal coronary angiograms, and in controls with angina. Patients—Sixty one patients with normal coronary angiograms (NCA group) referred to a single cardiac centre between March 1990 and April 1991; 25 matched controls with confirmed coronary artery disease (CAD group). Setting—Cardiac referral centre and oesophageal function testing laboratory. Main outcome measures—Oesophageal manometry, provocation tests, and 24 hour ambulatory pH monitoring. Results—Simultaneous contractions were more common (6.7% versus 0.8%, p<0.01), and the duration of peristaltic contractions was longer (2.9 versus 2.4 seconds, p<0.01) in the NCA group than in the CAD group. There were no group differences in the amplitude of peristaltic contractions, and none had nutcracker oesophagus. Ten (16%) patients with NCA and no patients with CAD had diffuse spasm (p=0.03). Twenty one (34%) patients with NCA, and five (20%) patients with CAD had abnormal gastro-oesophageal reflux (p>0.05). There was no significant difference between the groups in the number of patients whose pain was temporally related to pH events. Particular chest pain characteristics, or the presence of additional oesophageal symptoms, were not predictive of an oesophageal abnormality. Conclusion—Oesophageal function tests commonly implicate the oesophagus as a source of pain in patients with normal coronary angiograms. With the exception of simultaneous contractions during manometry however, the incidence of abnormalities and in particular the correlation of pH events with chest pain are as common in patients with normal coronary angiograms as in controls with angina. The oesophagus may often be an unrecognised source of pain in both groups of patients.
Keywords: oesophageal function; coronary artery disease; chest pain
Full Text
The Full Text of this article is available as a PDF (137.9 KB).
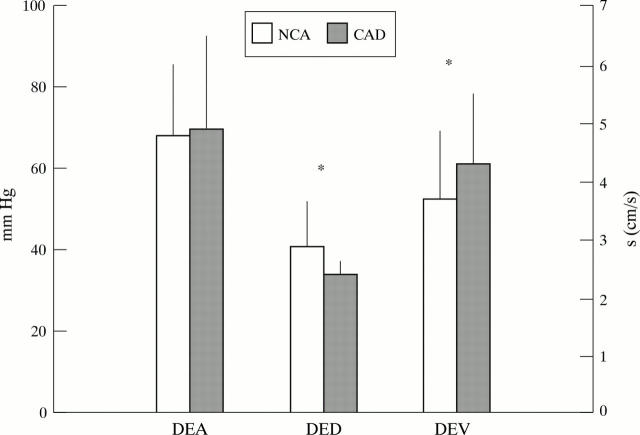
Figure 1 .
| NCA | CAD | p Value | |
| DEA (mm Hg) | 67.8 (29.4) | 69.4 (25.6) | 0.9 |
| DED (s) | 2.9 (0.7) | 2.4 (0.4) | <0.001 |
| DEV (cm/s) | 4.3 (1.2) | 4.3 (1.2) | 0.037 |
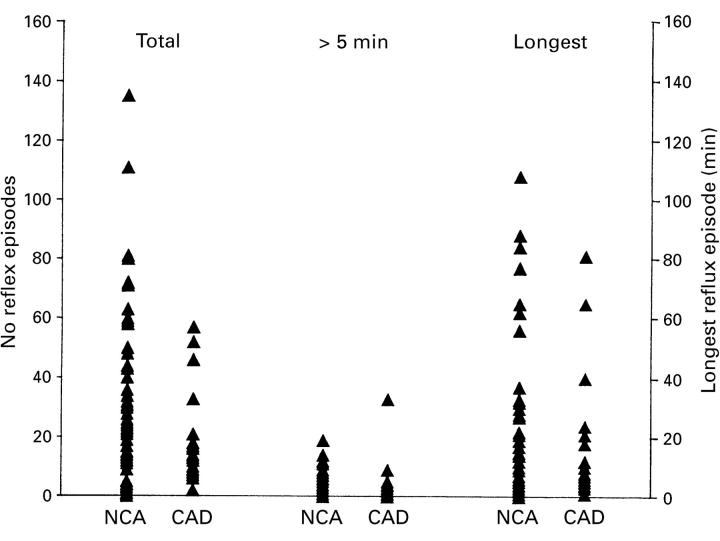
Figure 2 .
| Reflux episodes | NCA | CAD | p Value* |
| Total number | 20 (3.2 to 39.0) | 12.0 (7.5 to 17.5) | 0.3 |
| Number >5 min | 1.0 (0.0 to 5.0) | 1.0 (0.0 to 3.0) | 0.9 |
| Longest duration | 9.0 (1.2 to 21.7) | 7.0 (5.0 to 15.0) | 0.7 |
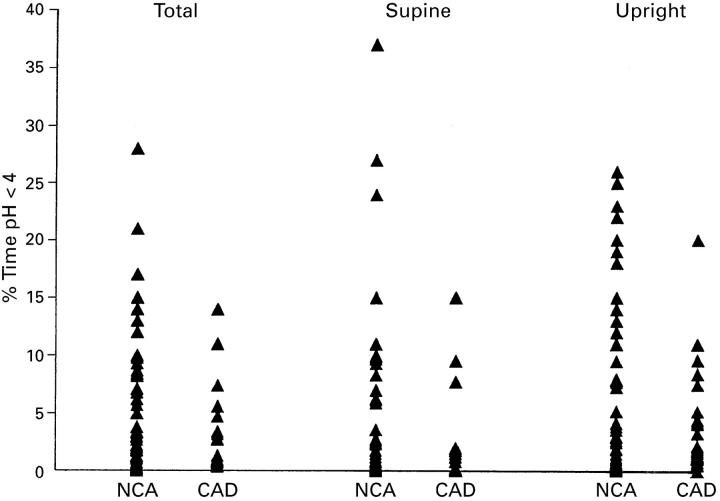
Figure 3 .
| Per cent time pH <4 | NCA | CAD | p Value* |
| Total (24 h) | 1.9 (0.3 to 8.6) | 1.3 (0.7 to 4.1) | 0.90 |
| Supine | 0.5 (0.0 to 5.3) | 0.0 (0.0 to 1.4) | 0.09 |
| Upright | 2.3 (0.4 to 10.3) | 1.8 (1.1 to 4.9) | 0.98 |
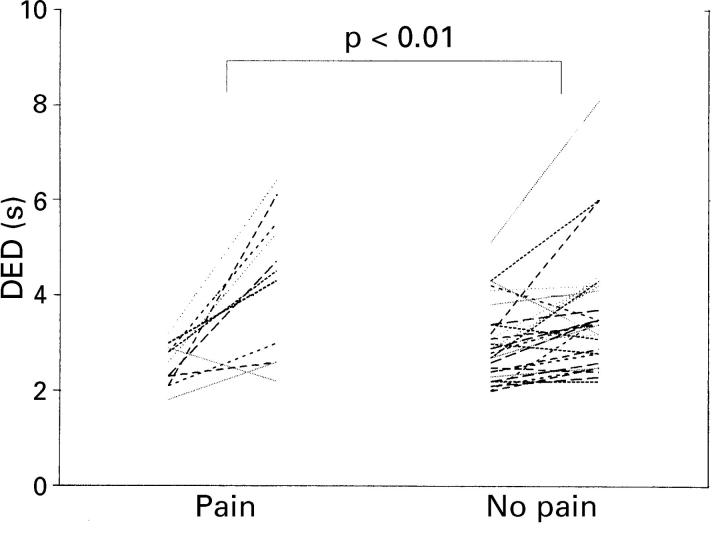
Figure 4 .
Mean distal peristaltic duration (DED) at baseline and after edrophonium in patients who reported pain, compared with patients who did not report pain.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson K. O., Dalton C. B., Bradley L. A., Richter J. E. Stress induces alteration of esophageal pressures in healthy volunteers and non-cardiac chest pain patients. Dig Dis Sci. 1989 Jan;34(1):83–91. doi: 10.1007/BF01536159. [DOI] [PubMed] [Google Scholar]
- Bennett J. R., Atkinson M. The differentiation between oesophageal and cardiac pain. Lancet. 1966 Nov 19;2(7473):1123–1127. doi: 10.1016/s0140-6736(66)92209-4. [DOI] [PubMed] [Google Scholar]
- Dalton C. B., Castell D. O., Hewson E. G., Wu W. C., Richter J. E. Diffuse esophageal spasm. A rare motility disorder not characterized by high-amplitude contractions. Dig Dis Sci. 1991 Aug;36(8):1025–1028. doi: 10.1007/BF01297441. [DOI] [PubMed] [Google Scholar]
- Dalton C. B., Hewson E. G., Castell D. O., Richter J. E. Edrophonium provocative test in noncardiac chest pain. Evaluation of testing techniques. Dig Dis Sci. 1990 Dec;35(12):1445–1451. doi: 10.1007/BF01540560. [DOI] [PubMed] [Google Scholar]
- Davies H. A., Page Z., Rush E. M., Brown A. L., Lewis M. J., Petch M. C. Oesophageal stimulation lowers exertional angina threshold. Lancet. 1985 May 4;1(8436):1011–1014. doi: 10.1016/s0140-6736(85)91614-9. [DOI] [PubMed] [Google Scholar]
- De Caestecker J. S., Pryde A., Heading R. C. Comparison of intravenous edrophonium and oesophageal acid perfusion during oesophageal manometry in patients with non-cardiac chest pain. Gut. 1988 Aug;29(8):1029–1034. doi: 10.1136/gut.29.8.1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeMeester T. R., O'Sullivan G. C., Bermudez G., Midell A. I., Cimochowski G. E., O'Drobinak J. Esophageal function in patients with angina-type chest pain and normal coronary angiograms. Ann Surg. 1982 Oct;196(4):488–498. doi: 10.1097/00000658-198210000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Pulido J., Patel P. H., Hunter W. C., Douglas J. E., Thomas E. Esophageal contribution to chest pain in patients with coronary artery disease. Chest. 1990 Oct;98(4):806–810. doi: 10.1378/chest.98.4.806. [DOI] [PubMed] [Google Scholar]
- Hewson E. G., Dalton C. B., Richter J. E. Comparison of esophageal manometry, provocative testing, and ambulatory monitoring in patients with unexplained chest pain. Dig Dis Sci. 1990 Mar;35(3):302–309. doi: 10.1007/BF01537406. [DOI] [PubMed] [Google Scholar]
- Hewson E. G., Sinclair J. W., Dalton C. B., Richter J. E. Twenty-four-hour esophageal pH monitoring: the most useful test for evaluating noncardiac chest pain. Am J Med. 1991 May;90(5):576–583. [PubMed] [Google Scholar]
- Hick D. G., Morrison J. F., Casey J. F., al-Ashhab W., Williams G. J., Davies G. A. Oesophageal motility, luminal pH, and electrocardiographic-ST segment analysis during spontaneous episodes of angina like chest pain. Gut. 1992 Jan;33(1):79–86. doi: 10.1136/gut.33.1.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KRAMER P., HOLLANDER W. Comparison of experimental esophageal pain with clinical pain of angina pectoris and esophageal disease. Gastroenterology. 1955 Nov;29(5):719–743. [PubMed] [Google Scholar]
- Linsell J., Owen W. J., Mason R. C., Anggiansah A. Edrophonium provocation test in the diagnosis of diffuse oesophageal spasm. Br J Surg. 1987 Aug;74(8):688–689. doi: 10.1002/bjs.1800740811. [DOI] [PubMed] [Google Scholar]
- Mellow M. H., Simpson A. G., Watt L., Schoolmeester L., Haye O. L. Esophageal acid perfusion in coronary artery disease. Induction of myocardial ischemia. Gastroenterology. 1983 Aug;85(2):306–312. [PubMed] [Google Scholar]
- Nevens F., Janssens J., Piessens J., Ghillebert G., De Geest H., Vantrappen G. Prospective study on prevalence of esophageal chest pain in patients referred on an elective basis to a cardiac unit for suspected myocardial ischemia. Dig Dis Sci. 1991 Feb;36(2):229–235. doi: 10.1007/BF01300762. [DOI] [PubMed] [Google Scholar]
- Richter J. E., Bradley L. A., DeMeester T. R., Wu W. C. Normal 24-hr ambulatory esophageal pH values. Influence of study center, pH electrode, age, and gender. Dig Dis Sci. 1992 Jun;37(6):849–856. doi: 10.1007/BF01300382. [DOI] [PubMed] [Google Scholar]
- Richter J. E., Wu W. C., Johns D. N., Blackwell J. N., Nelson J. L., 3rd, Castell J. A., Castell D. O. Esophageal manometry in 95 healthy adult volunteers. Variability of pressures with age and frequency of "abnormal" contractions. Dig Dis Sci. 1987 Jun;32(6):583–592. doi: 10.1007/BF01296157. [DOI] [PubMed] [Google Scholar]
- Schofield P. M., Bennett D. H., Whorwell P. J., Brooks N. H., Bray C. L., Ward C., Jones P. E. Exertional gastro-oesophageal reflux: a mechanism for symptoms in patients with angina pectoris and normal coronary angiograms. Br Med J (Clin Res Ed) 1987 Jun 6;294(6585):1459–1461. doi: 10.1136/bmj.294.6585.1459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schofield P. M., Whorwell P. J., Brooks N. H., Bennett D. H., Jones P. E. Oesophageal function in patients with angina pectoris: a comparison of patients with normal coronary angiograms and patients with coronary artery disease. Digestion. 1989;42(2):70–78. doi: 10.1159/000199828. [DOI] [PubMed] [Google Scholar]
- Singh S., Richter J. E., Hewson E. G., Sinclair J. W., Hackshaw B. T. The contribution of gastroesophageal reflux to chest pain in patients with coronary artery disease. Ann Intern Med. 1992 Nov 15;117(10):824–830. doi: 10.7326/0003-4819-117-10-824. [DOI] [PubMed] [Google Scholar]
- Svensson O., Stenport G., Tibbling L., Wranne B. Oesophageal function and coronary angiogram in patients with disabling chest pain. Acta Med Scand. 1978;204(3):173–178. doi: 10.1111/j.0954-6820.1978.tb08420.x. [DOI] [PubMed] [Google Scholar]
- Vantrappen G., Janssens J., Ghillebert G. The irritable oesophagus--a frequent cause of angina-like pain. Lancet. 1987 May 30;1(8544):1232–1234. doi: 10.1016/s0140-6736(87)92686-9. [DOI] [PubMed] [Google Scholar]
- Wiener G. J., Richter J. E., Copper J. B., Wu W. C., Castell D. O. The symptom index: a clinically important parameter of ambulatory 24-hour esophageal pH monitoring. Am J Gastroenterol. 1988 Apr;83(4):358–361. [PubMed] [Google Scholar]
- Wilson J. A., Pryde A., Cecilia A., Macintyre C. C., Heading R. C. Normal pharyngoesophageal motility. A study of 50 healthy subjects. Dig Dis Sci. 1989 Oct;34(10):1590–1599. doi: 10.1007/BF01537116. [DOI] [PubMed] [Google Scholar]
- de Caestecker J. S., Blackwell J. N., Brown J., Heading R. C. The oesophagus as a cause of recurrent chest pain: which patients should be investigated and which tests should be used? Lancet. 1985 Nov 23;2(8465):1143–1146. doi: 10.1016/s0140-6736(85)92676-5. [DOI] [PubMed] [Google Scholar]