Abstract
Background—Studies have shown that an altered visceral perception threshold plays a role in the pathogenesis of upper gastrointestinal tract symptoms in dyspeptic patients. However, it is not clear whether the compliance and adaptive relaxation of the proximal stomach contribute to the symptoms. Aims—To investigate whether abnormal relaxation or adaptation of the proximal stomach during the interdigestive state and the postprandial phase could explain the symptoms of functional dyspepsia. Subjects—Twelve volunteers and 12 patients with dysmotility-like functional dyspepsia were included in the study. Methods—An electronic barostat was used to investigate adaptation to distension of the proximal stomach and accommodation in response to a liquid meal. Dyspeptic symptoms during distension and accommodation were assessed. Results—When the subjects were in the fasting state, the pressure-volume curve showed slightly higher compliance in the dyspeptic patients (p<0.05). Patients not only had a higher score for nausea, bloating, and pain but also the increase in nausea and pain scores with intragastric pressure was higher than in volunteers (p<0.05). The increase in intragastric bag volume in response to a meal was significantly lower in patients (p<0.05). Both bloating and pain significantly increased in the patients (p<0.05), but not in the healthy volunteers. Conclusions—Patients with functional dyspepsia show slightly higher compliance to mechanical distension. Their visceral perception of mechanical stress is enhanced. In contrast with the balloon distension, relaxation after a meal was less. Therefore the postprandial symptoms cannot be explained fully by greater global tension in the stomach wall, as assessed by the barostat technique. Visceral hypersensitivity plays a major role in the pathogenesis of the symptoms.
Keywords: dyspepsia; gastric distension; gastric accommodation; gastric sensitivity
Full Text
The Full Text of this article is available as a PDF (222.8 KB).
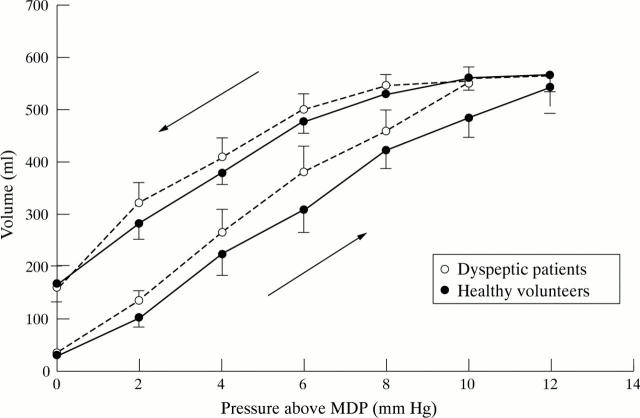
Figure 1 .
Mean volume-pressure curve in the dyspeptic patients and healthy volunteers. The inflation (ascending part of the pressure-volume) curve showed a significantly steeper slope (p<0.05) in the dyspeptic patients than in the controls, indicating a higher compliance in the dyspeptic patients. The descending part of the pressure-volume curve (deflation) showed a delay in the return of the gastric volume toward the values at minimal distending pressure (MDP) (hysteresis).
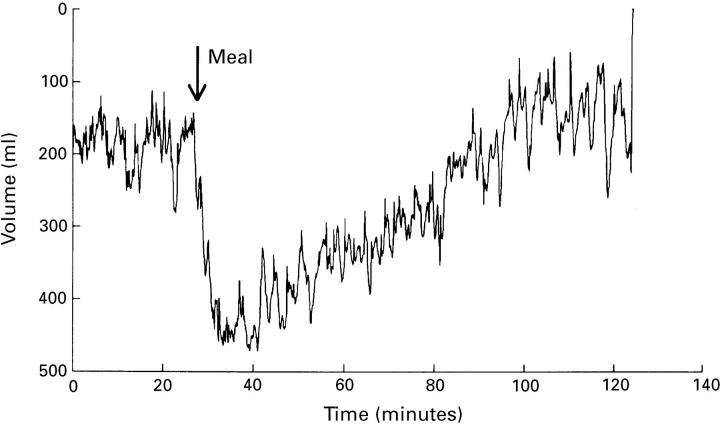
Figure 2 .
Example of a postprandial relaxation curve in a healthy volunteer. Baseline volume was measured at minimal distending pressure + 1 mm Hg. After the meal there was an increase in gastric bag volume to a maximum. The volume returned to the baseline value within 80 minutes.
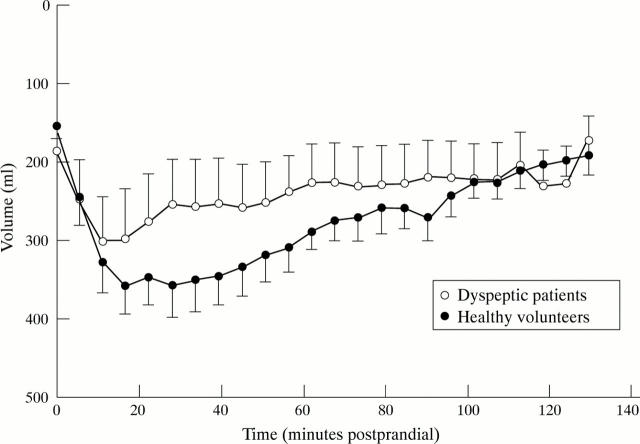
Figure 3 .
Mean postprandial relaxation curves in the dyspeptic patients and healthy volunteers. The increase in intragastric bag volume in the dyspeptic patients was significantly lower than that in the healthy volunteers (p<0.05). The time interval between the start of ingestion of the meal and the time at which the maximum volume was reached was significantly shorter in patients than in controls (p<0.01).
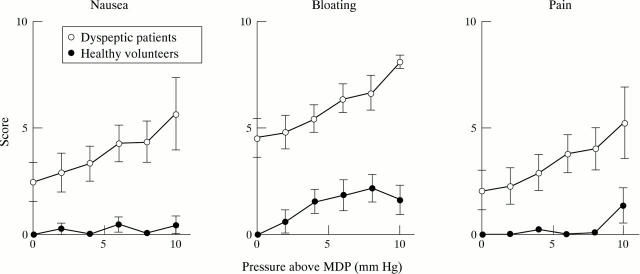
Figure 4 .
Nausea, bloating, and pain scores in relation to the gastric bag pressure above the minimal distending pressure (MDP) in dyspeptic patients and healthy volunteers. There was a significantly greater increase in nausea and pain scores with increasing pressure in the patients than in the healthy volunteers (p<0.05, p<0.01).
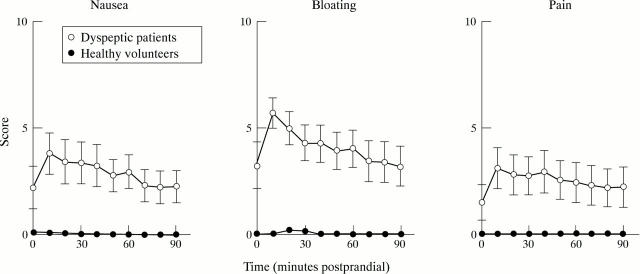
Figure 5 .
Nausea, bloating, and pain scores after the test meal in dyspeptic patients and healthy volunteers. After the meal, the dyspeptic patients had significantly more nausea, bloating, and pain than the healthy volunteers (p<0.05, p<0.05, p<0.05 respectively). The patients showed a significant increase in bloating and pain scores (p<0.05, p<0.04).
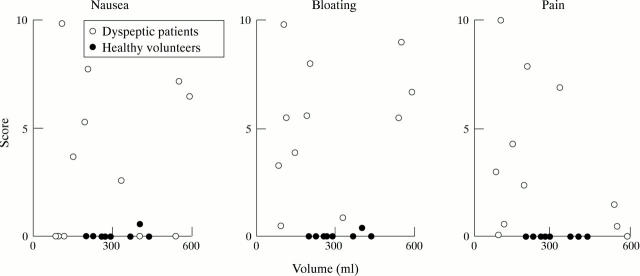
Figure 6 .
Individual nausea, bloating, and pain scores 10 minutes after the test meal plotted against relaxation volume. Postprandial symptoms are not related to volume.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ahluwalia N. K., Thompson D. G., Barlow J., Troncon L. E., Hollis S. Relaxation responses of the human proximal stomach to distension during fasting and after food. Am J Physiol. 1994 Aug;267(2 Pt 1):G166–G172. doi: 10.1152/ajpgi.1994.267.2.G166. [DOI] [PubMed] [Google Scholar]
- Azpiroz F., Malagelada J. R. Gastric tone measured by an electronic barostat in health and postsurgical gastroparesis. Gastroenterology. 1987 Apr;92(4):934–943. doi: 10.1016/0016-5085(87)90967-x. [DOI] [PubMed] [Google Scholar]
- Azpiroz F., Malagelada J. R. Importance of vagal input in maintaining gastric tone in the dog. J Physiol. 1987 Mar;384:511–524. doi: 10.1113/jphysiol.1987.sp016467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azpiroz F., Malagelada J. R. Intestinal control of gastric tone. Am J Physiol. 1985 Oct;249(4 Pt 1):G501–G509. doi: 10.1152/ajpgi.1985.249.4.G501. [DOI] [PubMed] [Google Scholar]
- Azpiroz F., Malagelada J. R. Physiological variations in canine gastric tone measured by an electronic barostat. Am J Physiol. 1985 Feb;248(2 Pt 1):G229–G237. doi: 10.1152/ajpgi.1985.248.2.G229. [DOI] [PubMed] [Google Scholar]
- Azpiroz F., Malagelada J. R. Pressure activity patterns in the canine proximal stomach: response to distension. Am J Physiol. 1984 Sep;247(3 Pt 1):G265–G272. doi: 10.1152/ajpgi.1984.247.3.G265. [DOI] [PubMed] [Google Scholar]
- Bassotti G., Pelli M. A., Morelli A. Duodenojejunal motor activity in patients with chronic dyspeptic symptoms. J Clin Gastroenterol. 1990 Feb;12(1):17–21. doi: 10.1097/00004836-199002000-00006. [DOI] [PubMed] [Google Scholar]
- Bradette M., Pare P., Douville P., Morin A. Visceral perception in health and functional dyspepsia. Crossover study of gastric distension with placebo and domperidone. Dig Dis Sci. 1991 Jan;36(1):52–58. doi: 10.1007/BF01300087. [DOI] [PubMed] [Google Scholar]
- Camilleri M., Brown M. L., Malagelada J. R. Relationship between impaired gastric emptying and abnormal gastrointestinal motility. Gastroenterology. 1986 Jul;91(1):94–99. doi: 10.1016/0016-5085(86)90444-0. [DOI] [PubMed] [Google Scholar]
- Jian R., Ducrot F., Ruskone A., Chaussade S., Rambaud J. C., Modigliani R., Rain J. D., Bernier J. J. Symptomatic, radionuclide and therapeutic assessment of chronic idiopathic dyspepsia. A double-blind placebo-controlled evaluation of cisapride. Dig Dis Sci. 1989 May;34(5):657–664. doi: 10.1007/BF01540334. [DOI] [PubMed] [Google Scholar]
- Lémann M., Dederding J. P., Flourié B., Franchisseur C., Rambaud J. C., Jian R. Abnormal perception of visceral pain in response to gastric distension in chronic idiopathic dyspepsia. The irritable stomach syndrome. Dig Dis Sci. 1991 Sep;36(9):1249–1254. doi: 10.1007/BF01307517. [DOI] [PubMed] [Google Scholar]
- Malagelada J. R. Gastrointestinal motor disturbances in functional dyspepsia. Scand J Gastroenterol Suppl. 1991;182:29–32. doi: 10.3109/00365529109109534. [DOI] [PubMed] [Google Scholar]
- Malagelada J. R., Stanghellini V. Manometric evaluation of functional upper gut symptoms. Gastroenterology. 1985 May;88(5 Pt 1):1223–1231. doi: 10.1016/s0016-5085(85)80083-4. [DOI] [PubMed] [Google Scholar]
- Management of dyspepsia: report of a working party. Lancet. 1988 Mar 12;1(8585):576–579. [PubMed] [Google Scholar]
- Mearin F., Cucala M., Azpiroz F., Malagelada J. R. The origin of symptoms on the brain-gut axis in functional dyspepsia. Gastroenterology. 1991 Oct;101(4):999–1006. doi: 10.1016/0016-5085(91)90726-2. [DOI] [PubMed] [Google Scholar]
- Notivol R., Coffin B., Azpiroz F., Mearin F., Serra J., Malagelada J. R. Gastric tone determines the sensitivity of the stomach to distention. Gastroenterology. 1995 Feb;108(2):330–336. doi: 10.1016/0016-5085(95)90057-8. [DOI] [PubMed] [Google Scholar]
- Ropert A., des Varannes S. B., Bizais Y., Rozé C., Galmiche J. P. Simultaneous assessment of liquid emptying and proximal gastric tone in humans. Gastroenterology. 1993 Sep;105(3):667–674. doi: 10.1016/0016-5085(93)90881-c. [DOI] [PubMed] [Google Scholar]
- Stanghellini V., Ghidini C., Maccarini M. R., Paparo G. F., Corinaldesi R., Barbara L. Fasting and postprandial gastrointestinal motility in ulcer and non-ulcer dyspepsia. Gut. 1992 Feb;33(2):184–190. doi: 10.1136/gut.33.2.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talley N. J., Piper D. W. The association between non-ulcer dyspepsia and other gastrointestinal disorders. Scand J Gastroenterol. 1985 Sep;20(7):896–900. doi: 10.3109/00365528509088842. [DOI] [PubMed] [Google Scholar]
- Troncon L. E., Thompson D. G., Ahluwalia N. K., Barlow J., Heggie L. Relations between upper abdominal symptoms and gastric distension abnormalities in dysmotility like functional dyspepsia and after vagotomy. Gut. 1995 Jul;37(1):17–22. doi: 10.1136/gut.37.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wegener M., Börsch G., Schaffstein J., Schulz-Flake C., Mai U., Leverkus F. Are dyspeptic symptoms in patients with Campylobacter pylori-associated type B gastritis linked to delayed gastric emptying? Am J Gastroenterol. 1988 Jul;83(7):737–740. [PubMed] [Google Scholar]
- Whitehead W. E., Delvaux M. Standardization of barostat procedures for testing smooth muscle tone and sensory thresholds in the gastrointestinal tract. The Working Team of Glaxo-Wellcome Research, UK. Dig Dis Sci. 1997 Feb;42(2):223–241. doi: 10.1023/a:1018885028501. [DOI] [PubMed] [Google Scholar]