Abstract
Background—Visceral hyperalgesia is a hallmark of functional gastrointestinal disorders. Antidepressants improve symptoms in these patients, although their mode of action is unclear. Antidepressant, anticholinergic, and analgesic mechanisms have been proposed. Aims—To investigate whether imipramine, which has a visceral analgesic effect, increases pain thresholds to experimental visceral pain. Methods—Visceral perception for first sensation and pain was measured with intraoesophageal balloon distension in 15 male volunteers. The effect of imipramine was studied in a double blind, placebo controlled, crossover study. Imipramine was given in ascending doses for 12 days (25 mg days 1-3, 50 mg days 4-6, 75 mg days 7-12), with oesophageal perception studied on day 13. Results—Inflation volumes and intraballoon pressures at first sensation were not different between placebo and imipramine. Balloon inflation volume at pain threshold was higher on imipramine (p=0.015). Median intraballoon pressures were not different at pain threshold for placebo and imipramine. Oesophageal wall compliance was not affected by imipramine. Conclusion—Increased pain thresholds on imipramine in this group of normal male volunteers in the absence of changes in oesophageal tone imply the presence of a visceral analgesic effect.
Keywords: antidepressants; imipramine; visceral hyperalgesia; oesophageal balloon; distension; functional bowel syndromes
Full Text
The Full Text of this article is available as a PDF (134.8 KB).
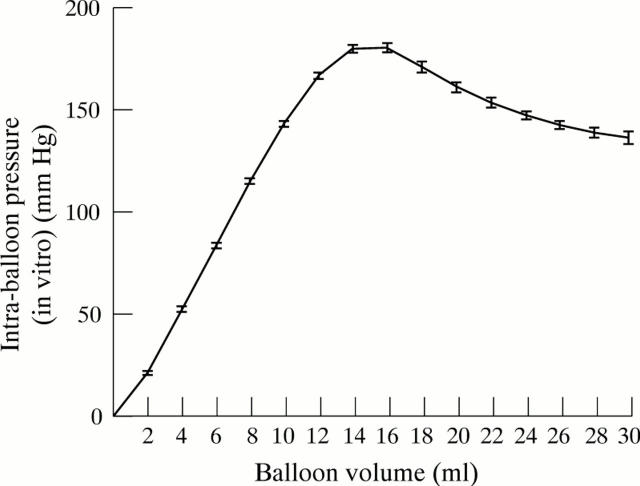
Figure 1 .
Balloon compliance. Mean pressure volume curve of the 30 pre-IOBD, in vitro assessments of the six balloons used in the study.
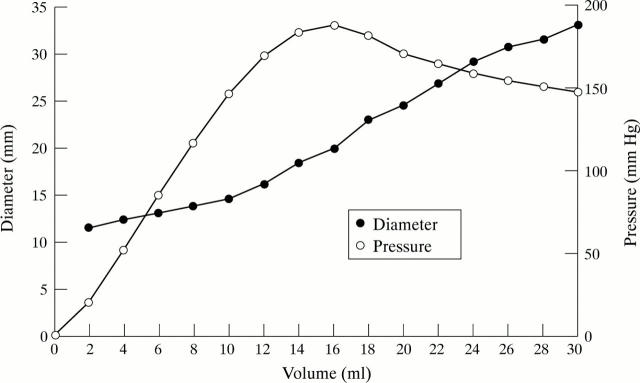
Figure 2 .
Relation between balloon volume, pressure, and diameter in vitro.
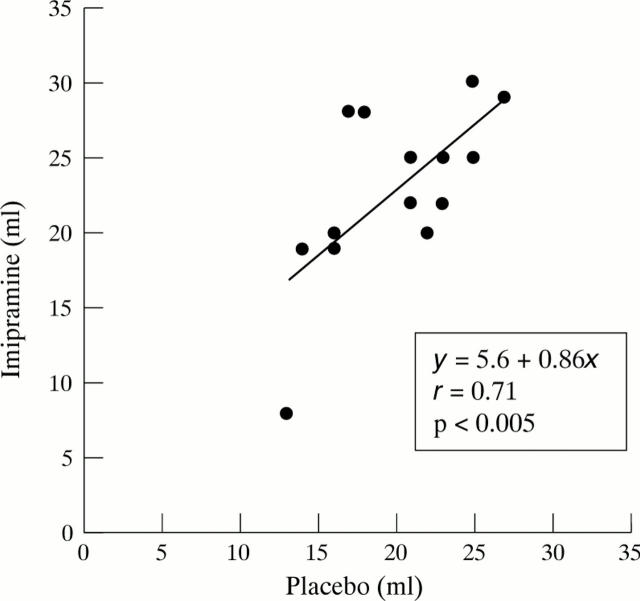
Figure 3 .
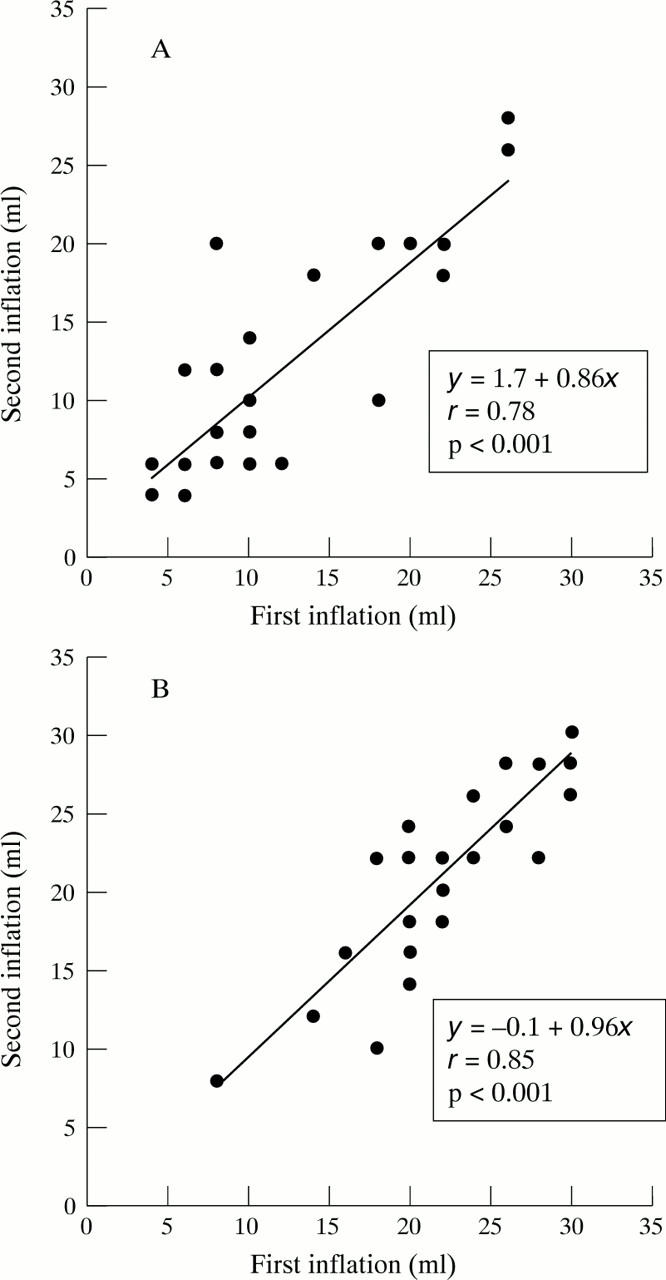
Reproducibility of perception thresholds of the two testing days. Volumes at perception threshold for first inflation series (x axis) plotted against volumes at perception threshold for second inflation series 10 minutes later (y axis). (A) Sensation thresholds; (B) pain thresholds.
Figure 4 .
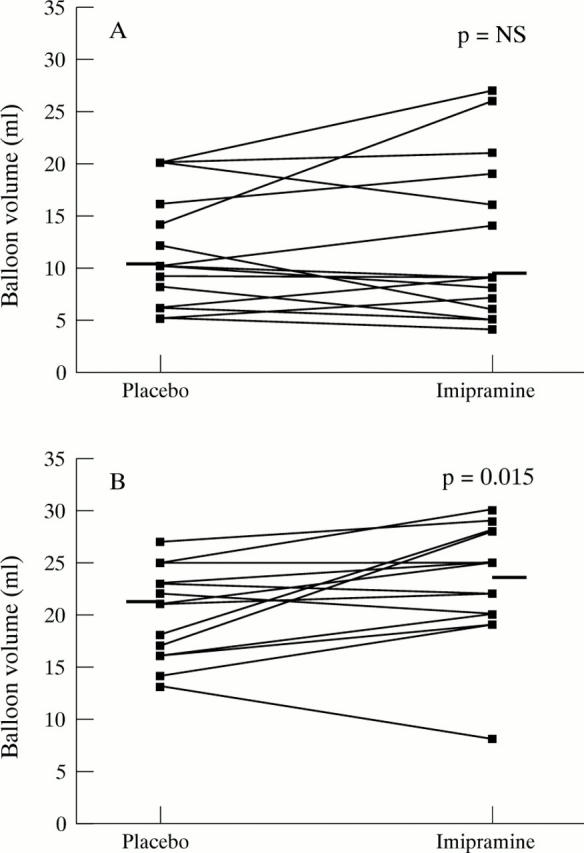
Perception thresholds on placebo and imipramine. (A) Volumes at thresholds for first sensation (n=15); (B) volumes at pain thresholds (n=14). Median represented by horizontal bar.
Figure 5 .
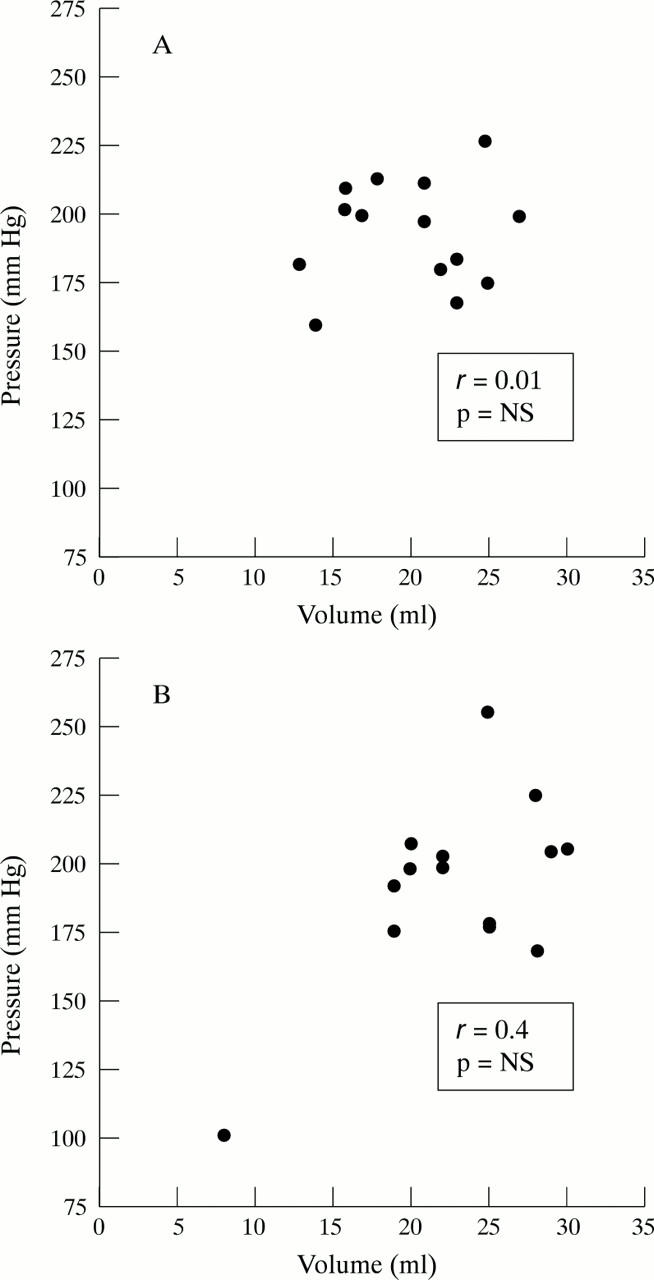
Balloon volume and pressure at pain threshold for placebo (A) and imipramine (B).
Figure 6 .
Volumes at pain threshold on placebo and imipramine.
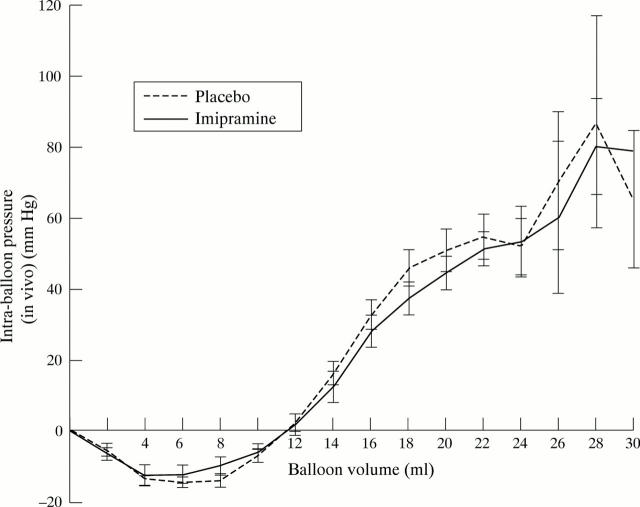
Figure 7 .
Oesophageal wall compliance. Difference between in vivo minus in vitro balloon pressure (mean (SEM)) at corresponding inflation volumes.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barish C. F., Castell D. O., Richter J. E. Graded esophageal balloon distention. A new provocative test for noncardiac chest pain. Dig Dis Sci. 1986 Dec;31(12):1292–1298. doi: 10.1007/BF01299805. [DOI] [PubMed] [Google Scholar]
- Botney M., Fields H. L. Amitriptyline potentiates morphine analgesia by a direct action on the central nervous system. Ann Neurol. 1983 Feb;13(2):160–164. doi: 10.1002/ana.410130209. [DOI] [PubMed] [Google Scholar]
- Bromm B., Meier W., Scharein E. Imipramine reduces experimental pain. Pain. 1986 May;25(2):245–257. doi: 10.1016/0304-3959(86)90100-4. [DOI] [PubMed] [Google Scholar]
- Bueno L., Fioramonti J., Delvaux M., Frexinos J. Mediators and pharmacology of visceral sensitivity: from basic to clinical investigations. Gastroenterology. 1997 May;112(5):1714–1743. doi: 10.1016/s0016-5085(97)70056-8. [DOI] [PubMed] [Google Scholar]
- Cannon R. O., 3rd, Quyyumi A. A., Mincemoyer R., Stine A. M., Gracely R. H., Smith W. B., Geraci M. F., Black B. C., Uhde T. W., Waclawiw M. A. Imipramine in patients with chest pain despite normal coronary angiograms. N Engl J Med. 1994 May 19;330(20):1411–1417. doi: 10.1056/NEJM199405193302003. [DOI] [PubMed] [Google Scholar]
- Clouse R. E., Lustman P. J., Eckert T. C., Ferney D. M., Griffith L. S. Low-dose trazodone for symptomatic patients with esophageal contraction abnormalities. A double-blind, placebo-controlled trial. Gastroenterology. 1987 Apr;92(4):1027–1036. doi: 10.1016/0016-5085(87)90979-6. [DOI] [PubMed] [Google Scholar]
- Clouse R. E., Lustman P. J., Geisman R. A., Alpers D. H. Antidepressant therapy in 138 patients with irritable bowel syndrome: a five-year clinical experience. Aliment Pharmacol Ther. 1994 Aug;8(4):409–416. doi: 10.1111/j.1365-2036.1994.tb00308.x. [DOI] [PubMed] [Google Scholar]
- Cook I. J., van Eeden A., Collins S. M. Patients with irritable bowel syndrome have greater pain tolerance than normal subjects. Gastroenterology. 1987 Oct;93(4):727–733. doi: 10.1016/0016-5085(87)90434-3. [DOI] [PubMed] [Google Scholar]
- Costantini M., Sturniolo G. C., Zaninotto G., D'Incà R., Polo R., Naccarato R., Ancona E. Altered esophageal pain threshold in irritable bowel syndrome. Dig Dis Sci. 1993 Feb;38(2):206–212. doi: 10.1007/BF01307536. [DOI] [PubMed] [Google Scholar]
- DeVault K. R., Castell D. O. Esophageal balloon distention and cerebral evoked potential recording in the evaluation of unexplained chest pain. Am J Med. 1992 May 27;92(5A):20S–26S. doi: 10.1016/0002-9343(92)80052-2. [DOI] [PubMed] [Google Scholar]
- Egbunike I. G., Chaffee B. J. Antidepressants in the management of chronic pain syndromes. Pharmacotherapy. 1990;10(4):262–270. [PubMed] [Google Scholar]
- Fass R. Unexplained noncardiac chest pain. Ann Intern Med. 1997 Apr 15;126(8):662–664. doi: 10.7326/0003-4819-126-8-199704150-00021. [DOI] [PubMed] [Google Scholar]
- Feinmann C. Pain relief by antidepressants: possible modes of action. Pain. 1985 Sep;23(1):1–8. doi: 10.1016/0304-3959(85)90223-4. [DOI] [PubMed] [Google Scholar]
- France R. D., Houpt J. L., Ellinwood E. H. Therapeutic effects of antidepressants in chronic pain. Gen Hosp Psychiatry. 1984 Jan;6(1):55–63. doi: 10.1016/0163-8343(84)90060-4. [DOI] [PubMed] [Google Scholar]
- Greenbaum D. S., Mayle J. E., Vanegeren L. E., Jerome J. A., Mayor J. W., Greenbaum R. B., Matson R. W., Stein G. E., Dean H. A., Halvorsen N. A. Effects of desipramine on irritable bowel syndrome compared with atropine and placebo. Dig Dis Sci. 1987 Mar;32(3):257–266. doi: 10.1007/BF01297051. [DOI] [PubMed] [Google Scholar]
- Isenberg K. E., Cicero T. J. Possible involvement of opiate receptors in the pharmacological profiles of antidepressant compounds. Eur J Pharmacol. 1984 Aug 3;103(1-2):57–63. doi: 10.1016/0014-2999(84)90189-4. [DOI] [PubMed] [Google Scholar]
- Kvinesdal B., Molin J., Frøland A., Gram L. F. Imipramine treatment of painful diabetic neuropathy. JAMA. 1984 Apr 6;251(13):1727–1730. [PubMed] [Google Scholar]
- Lasch H., DeVault K. R., Castell D. O. Intraesophageal balloon distention in the evaluation of sensory thresholds: studies on reproducibility and comparison of balloon composition. Am J Gastroenterol. 1994 Aug;89(8):1185–1190. [PubMed] [Google Scholar]
- Lynn R. B. Mechanisms of esophageal pain. Am J Med. 1992 May 27;92(5A):11S–19S. doi: 10.1016/0002-9343(92)80051-z. [DOI] [PubMed] [Google Scholar]
- Lémann M., Dederding J. P., Flourié B., Franchisseur C., Rambaud J. C., Jian R. Abnormal perception of visceral pain in response to gastric distension in chronic idiopathic dyspepsia. The irritable stomach syndrome. Dig Dis Sci. 1991 Sep;36(9):1249–1254. doi: 10.1007/BF01307517. [DOI] [PubMed] [Google Scholar]
- Magni G. The use of antidepressants in the treatment of chronic pain. A review of the current evidence. Drugs. 1991 Nov;42(5):730–748. doi: 10.2165/00003495-199142050-00002. [DOI] [PubMed] [Google Scholar]
- Max M. B., Lynch S. A., Muir J., Shoaf S. E., Smoller B., Dubner R. Effects of desipramine, amitriptyline, and fluoxetine on pain in diabetic neuropathy. N Engl J Med. 1992 May 7;326(19):1250–1256. doi: 10.1056/NEJM199205073261904. [DOI] [PubMed] [Google Scholar]
- Mayer E. A., Gebhart G. F. Basic and clinical aspects of visceral hyperalgesia. Gastroenterology. 1994 Jul;107(1):271–293. doi: 10.1016/0016-5085(94)90086-8. [DOI] [PubMed] [Google Scholar]
- Mayer E. A., Raybould H. E. Role of visceral afferent mechanisms in functional bowel disorders. Gastroenterology. 1990 Dec;99(6):1688–1704. doi: 10.1016/0016-5085(90)90475-g. [DOI] [PubMed] [Google Scholar]
- Montastruc J. L., Tran M. A., Blanc M., Charlet J. P., David J., Mansat M., Cotonat J., Patacq-Sapijanskas M., Guiraud-Chaumeil B., Rascol A. Measurement of plasma levels of clomipramine in the treatment of chronic pain. Clin Neuropharmacol. 1985;8(1):78–82. doi: 10.1097/00002826-198503000-00008. [DOI] [PubMed] [Google Scholar]
- Naliboff B., Mayer E. A. Sensational developments in the irritable bowel. Gut. 1996 Nov;39(5):770–771. doi: 10.1136/gut.39.5.770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paterson W. G., Selucky M., Hynna-Liepert T. T. Effect of intraesophageal location and muscarinic blockade on balloon distension-induced chest pain. Dig Dis Sci. 1991 Mar;36(3):282–288. doi: 10.1007/BF01318197. [DOI] [PubMed] [Google Scholar]
- Peghini P. L., Castell D. O. Does sensitization of esophageal mucosal receptors occur during provocative testing? Am J Gastroenterol. 1997 Jun;92(6):919–920. [PubMed] [Google Scholar]
- Rao S. S., Gregersen H., Hayek B., Summers R. W., Christensen J. Unexplained chest pain: the hypersensitive, hyperreactive, and poorly compliant esophagus. Ann Intern Med. 1996 Jun 1;124(11):950–958. doi: 10.7326/0003-4819-124-11-199606010-00002. [DOI] [PubMed] [Google Scholar]
- Richter J. E., Barish C. F., Castell D. O. Abnormal sensory perception in patients with esophageal chest pain. Gastroenterology. 1986 Oct;91(4):845–852. doi: 10.1016/0016-5085(86)90685-2. [DOI] [PubMed] [Google Scholar]
- Ritchie J. Pain from distension of the pelvic colon by inflating a balloon in the irritable colon syndrome. Gut. 1973 Feb;14(2):125–132. doi: 10.1136/gut.14.2.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato T. L., Madakasira S. Monitoring tricyclic antidepressant plasma levels. Am Fam Physician. 1984 May;29(5):199–202. [PubMed] [Google Scholar]
- Silverman D. H., Munakata J. A., Ennes H., Mandelkern M. A., Hoh C. K., Mayer E. A. Regional cerebral activity in normal and pathological perception of visceral pain. Gastroenterology. 1997 Jan;112(1):64–72. doi: 10.1016/s0016-5085(97)70220-8. [DOI] [PubMed] [Google Scholar]
- Trimble K. C., Farouk R., Pryde A., Douglas S., Heading R. C. Heightened visceral sensation in functional gastrointestinal disease is not site-specific. Evidence for a generalized disorder of gut sensitivity. Dig Dis Sci. 1995 Aug;40(8):1607–1613. doi: 10.1007/BF02212678. [DOI] [PubMed] [Google Scholar]
- Wang J. K. Antinociceptive effect of intrathecally administered serotonin. Anesthesiology. 1977 Sep;47(3):269–271. doi: 10.1097/00000542-197709000-00007. [DOI] [PubMed] [Google Scholar]
- Whitehead W. E., Holtkotter B., Enck P., Hoelzl R., Holmes K. D., Anthony J., Shabsin H. S., Schuster M. M. Tolerance for rectosigmoid distention in irritable bowel syndrome. Gastroenterology. 1990 May;98(5 Pt 1):1187–1192. doi: 10.1016/0016-5085(90)90332-u. [DOI] [PubMed] [Google Scholar]
- de Caestecker J. S., Pryde A., Heading R. C. Site and mechanism of pain perception with oesophageal balloon distension and intravenous edrophonium in patients with oesophageal chest pain. Gut. 1992 May;33(5):580–586. doi: 10.1136/gut.33.5.580. [DOI] [PMC free article] [PubMed] [Google Scholar]