Abstract
BACKGROUND—Perception of, and adaptation of the rectum to, distension probably play an important role in the maintenance of continence, but perception studies in faecal incontinence provide controversial conclusions possibly related to methodological biases. In order to better understand perception disorders, the aim of this study was to analyse anorectal adaptation to rectal isobaric distension in subjects with incontinence. PATIENTS/METHODS—Between June 95 and December 97, 97 consecutive patients (nine men and 88 women, mean (SEM) age 55 (1) years) suffering from incontinence were evaluated and compared with 15healthy volunteers (four men and 11 women, mean age 48 (3) years). The patients were classified into three groups according to their perception status to rectal isobaric distensions (impaired, 22; normal, 61; enhanced, 14). Anal and rectal adaptations to increasing rectal pressure were analysed using a model of rectal isobaric distension. RESULTS—The four groups did not differ with respect to age, parity, or sex ratio. Magnitude of incontinence, prevalence of pelvic disorders, and sphincter defects were similar in the incontinent groups. When compared with healthy controls, anal pressure and rectal adaptation to distension were decreased in incontinent patients. When compared with incontinent patients with normal perception, patients with enhanced perception experienced similar rectal adaptation but had reduced anal pressure. In contrast, patients with impaired perception showed considerably decreased rectal adaptation but had similar anal pressure. CONCLUSION—Abnormal sensations during rectal distension are observed in one third of subjects suffering from incontinence. These abnormalities may reflect hyperreactivity or neuropathological damage of the rectal wall.
Keywords: faecal; incontinence; rectum; barostat; perception; distension
Full Text
The Full Text of this article is available as a PDF (133.2 KB).
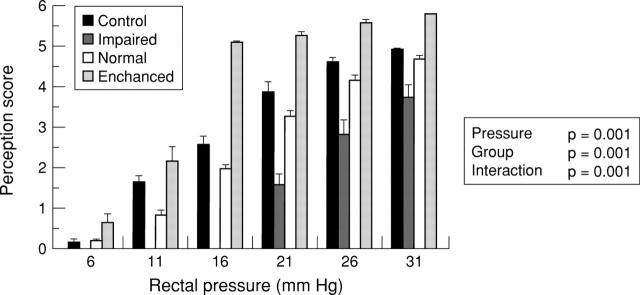
Figure 1 .
Rectal pressures and anal pressures recorded at both upper and lower parts as a function of rectal pressure during phasic isobaric distensions of the rectum in healthy controls and in incontinent patients with impaired, normal, or increased rectal perceptions.
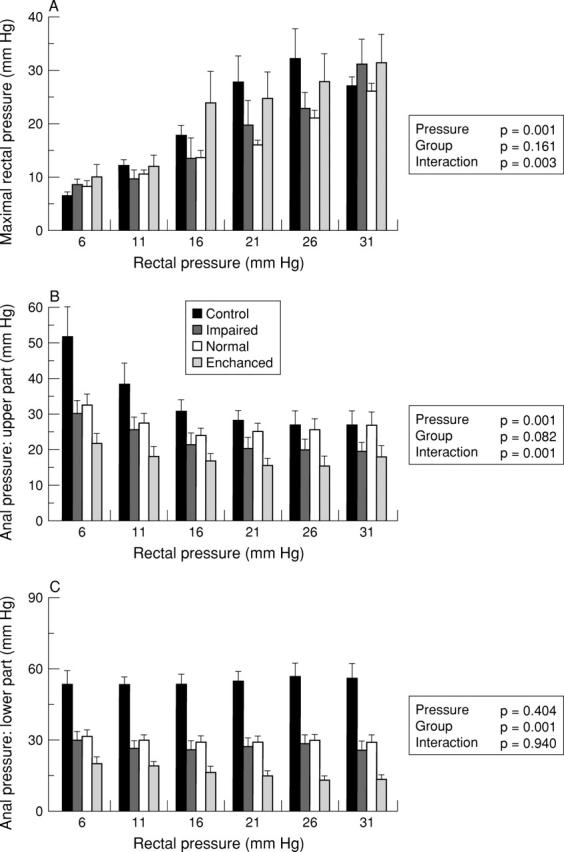
Figure 2 .
Rectal volumes as a function of rectal pressure during phasic isobaric distensions of the rectum in healthy controls and in incontinent patients with impaired, normal, or increased rectal perceptions. Rectal volumes were recorded at the end of each pressure plateau (A; maximal rectal volume), at the end of ascending pressure variation (B; volume variation during increasing pressure), and between these two points of stabilised pressure (C; volume variation at constant pressure).
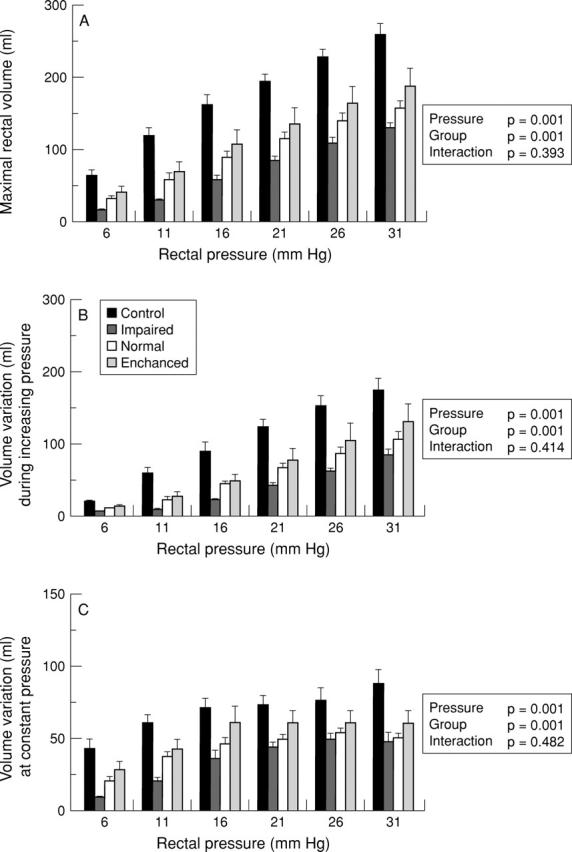
Figure 3 .
Rectal perception as a function of rectal pressure during phasic isobaric distensions of the rectum in healthy controls and in incontinent patients with impaired, normal, or increased rectal perceptions. Rectal perception was quantified by a score ranging from no sensation (0) to pain (6).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Akervall S., Fasth S., Nordgren S., Oresland T., Hultén L. Rectal reservoir and sensory function studied by graded isobaric distension in normal man. Gut. 1989 Apr;30(4):496–502. doi: 10.1136/gut.30.4.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akervall S., Nordgren S., Fasth S., Oresland T., Pettersson K., Hultén L. The effects of age, gender, and parity on rectoanal functions in adults. Scand J Gastroenterol. 1990 Dec;25(12):1247–1256. doi: 10.3109/00365529008998561. [DOI] [PubMed] [Google Scholar]
- Allen M. L., Orr W. C., Robinson M. G. Anorectal functioning in fecal incontinence. Dig Dis Sci. 1988 Jan;33(1):36–40. doi: 10.1007/BF01536628. [DOI] [PubMed] [Google Scholar]
- Bielefeldt K., Enck P., Erckenbrecht J. F. Sensory and motor function in the maintenance of anal continence. Dis Colon Rectum. 1990 Aug;33(8):674–678. doi: 10.1007/BF02150743. [DOI] [PubMed] [Google Scholar]
- Ferguson G. H., Redford J., Barrett J. A., Kiff E. S. The appreciation of rectal distention in fecal incontinence. Dis Colon Rectum. 1989 Nov;32(11):964–967. doi: 10.1007/BF02552274. [DOI] [PubMed] [Google Scholar]
- Hachet T., Caussette M. A multifunction and programmable computerized barostat. Gastroenterol Clin Biol. 1993;17(5):347–351. [PubMed] [Google Scholar]
- MacDonagh R., Sun W. M., Thomas D. G., Smallwood R., Read N. W. Anorectal function in patients with complete supraconal spinal cord lesions. Gut. 1992 Nov;33(11):1532–1538. doi: 10.1136/gut.33.11.1532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madoff R. D., Orrom W. J., Rothenberger D. A., Goldberg S. M. Rectal compliance: a critical reappraisal. Int J Colorectal Dis. 1990 Feb;5(1):37–40. doi: 10.1007/BF00496148. [DOI] [PubMed] [Google Scholar]
- Malcolm A., Phillips S. F., Camilleri M., Hanson R. B. Pharmacological modulation of rectal tone alters perception of distention in humans. Am J Gastroenterol. 1997 Nov;92(11):2073–2079. [PubMed] [Google Scholar]
- Meshkinpour H., Movahedi H., Welgan P. Clinical value of anorectal manometry index in neurogenic fecal incontinence. Dis Colon Rectum. 1997 Apr;40(4):457–461. doi: 10.1007/BF02258392. [DOI] [PubMed] [Google Scholar]
- Miner P. B., Donnelly T. C., Read N. W. Investigation of mode of action of biofeedback in treatment of fecal incontinence. Dig Dis Sci. 1990 Oct;35(10):1291–1298. doi: 10.1007/BF01536422. [DOI] [PubMed] [Google Scholar]
- Munakata J., Naliboff B., Harraf F., Kodner A., Lembo T., Chang L., Silverman D. H., Mayer E. A. Repetitive sigmoid stimulation induces rectal hyperalgesia in patients with irritable bowel syndrome. Gastroenterology. 1997 Jan;112(1):55–63. doi: 10.1016/s0016-5085(97)70219-1. [DOI] [PubMed] [Google Scholar]
- Naliboff B. D., Munakata J., Fullerton S., Gracely R. H., Kodner A., Harraf F., Mayer E. A. Evidence for two distinct perceptual alterations in irritable bowel syndrome. Gut. 1997 Oct;41(4):505–512. doi: 10.1136/gut.41.4.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Notivol R., Coffin B., Azpiroz F., Mearin F., Serra J., Malagelada J. R. Gastric tone determines the sensitivity of the stomach to distention. Gastroenterology. 1995 Feb;108(2):330–336. doi: 10.1016/0016-5085(95)90057-8. [DOI] [PubMed] [Google Scholar]
- Rao G. N., Drew P. J., Monson J. R., Duthie G. S. Physiology of rectal sensations: a mathematic approach. Dis Colon Rectum. 1997 Mar;40(3):298–306. doi: 10.1007/BF02050419. [DOI] [PubMed] [Google Scholar]
- Rao S. S., Patel R. S. How useful are manometric tests of anorectal function in the management of defecation disorders? Am J Gastroenterol. 1997 Mar;92(3):469–475. [PubMed] [Google Scholar]
- Rasmussen O. O., Sørensen M., Tetzschner T., Christiansen J. Anorectal pressure gradient in patients with anal incontinence. Dis Colon Rectum. 1992 Jan;35(1):8–11. doi: 10.1007/BF02053331. [DOI] [PubMed] [Google Scholar]
- Silverman D. H., Munakata J. A., Ennes H., Mandelkern M. A., Hoh C. K., Mayer E. A. Regional cerebral activity in normal and pathological perception of visceral pain. Gastroenterology. 1997 Jan;112(1):64–72. doi: 10.1016/s0016-5085(97)70220-8. [DOI] [PubMed] [Google Scholar]
- Siproudhis L., Bellissant E., Juguet F., Allain H., Bretagne J. F., Gosselin M. Effects of cholinergic agents on anorectal physiology. Aliment Pharmacol Ther. 1998 Aug;12(8):747–754. doi: 10.1046/j.1365-2036.1998.00361.x. [DOI] [PubMed] [Google Scholar]
- Siproudhis L., Bellissant E., Juguet F., Allain H., Bretagne J. F., Gosselin M. Octreotide acts on anorectal physiology: a dynamic study in healthy subjects. Clin Pharmacol Ther. 1998 Oct;64(4):424–432. doi: 10.1016/S0009-9236(98)90073-X. [DOI] [PubMed] [Google Scholar]
- Siproudhis L., Bellissant E., Juguet F., Mendler M. H., Allain H., Bretagne J. F., Gosselin M. Rectal adaptation to distension in patients with overt rectal prolapse. Br J Surg. 1998 Nov;85(11):1527–1532. doi: 10.1046/j.1365-2168.1998.00912.x. [DOI] [PubMed] [Google Scholar]
- Siproudhis L., Dautrème S., Ropert A., Bretagne J. F., Heresbach D., Raoul J. L., Gosselin M. Dyschezia and rectocele--a marriage of convenience? Physiologic evaluation of the rectocele in a group of 52 women complaining of difficulty in evacuation. Dis Colon Rectum. 1993 Nov;36(11):1030–1036. doi: 10.1007/BF02047295. [DOI] [PubMed] [Google Scholar]
- Speakman C. T., Hoyle C. H., Kamm M. A., Swash M., Henry M. M., Nicholls R. J., Burnstock G. Abnormal internal anal sphincter fibrosis and elasticity in fecal incontinence. Dis Colon Rectum. 1995 Apr;38(4):407–410. doi: 10.1007/BF02054231. [DOI] [PubMed] [Google Scholar]
- Speakman C. T., Kamm M. A. Abnormal visceral autonomic innervation in neurogenic faecal incontinence. Gut. 1993 Feb;34(2):215–221. doi: 10.1136/gut.34.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun W. M., Donnelly T. C., Read N. W. Utility of a combined test of anorectal manometry, electromyography, and sensation in determining the mechanism of 'idiopathic' faecal incontinence. Gut. 1992 Jun;33(6):807–813. doi: 10.1136/gut.33.6.807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun W. M., Read N. W., Miner P. B., Kerrigan D. D., Donnelly T. C. The role of transient internal sphincter relaxation in faecal incontinence? Int J Colorectal Dis. 1990 Feb;5(1):31–36. doi: 10.1007/BF00496147. [DOI] [PubMed] [Google Scholar]
- Sun W. M., Read N. W., Miner P. B. Relation between rectal sensation and anal function in normal subjects and patients with faecal incontinence. Gut. 1990 Sep;31(9):1056–1061. doi: 10.1136/gut.31.9.1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swash M., Gray A., Lubowski D. Z., Nicholls R. J. Ultrastructural changes in internal anal sphincter in neurogenic faecal incontinence. Gut. 1988 Dec;29(12):1692–1698. doi: 10.1136/gut.29.12.1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehead W. E., Delvaux M. Standardization of barostat procedures for testing smooth muscle tone and sensory thresholds in the gastrointestinal tract. The Working Team of Glaxo-Wellcome Research, UK. Dig Dis Sci. 1997 Feb;42(2):223–241. doi: 10.1023/a:1018885028501. [DOI] [PubMed] [Google Scholar]