Abstract
BACKGROUND/AIMS—Quality of life is an important determinant of the effectiveness of health technologies, but it has rarely been assessed in patients receiving home parenteral nutrition (HPN). PATIENTS/METHODS—The non-disease specific sickness impact profile (SIP) and the disease specific inflammatory bowel disease questionnaire (IBDQ) were used on a cohort of 49 patients receiving HPN, and the results compared with those for 36 non-HPN patients with either anatomical (<200 cm) or functional (faecal energy excretion >2.0 MJ/day (~488 kcal/day)) short bowel. RESULTS—In the HPN patients the SIP scores were worse (higher) overall (17 (13)% v 8 (9)%) and with regard to physical (13 (15)% v 5 (8)%) and psychosocial (14 (12)% v 9 (11)%) dimensions and independent categories (20 (12)% v 9 (8)%) compared with the non-HPN patients (means (SD); all p<0.001). The IBDQ scores were worse (lower) in the HPN patients overall (5.0 (4.3-5.7) v 5.6 (4.8-6.2)) and with regard to systemic symptoms (3.8 (2.8-5.4) v 5.2 (3.9-5.9)) and emotional (5.3 (4.4-6.2) v 5.8 (5.4-6.4)) and social (4.3 (3.4-5.5) v 4.8 (4.5-5.8)) function (median (25-75%); all p<0.05), but only tended to be worse with regard to bowel symptoms (5.2 (4.8-6.1) v 5.7 (4.9-6.4), p = 0.08). HPN also reduced quality of life in patients with a stoma, whereas a stoma did not reduce quality of life among the non-HPN patients. Female HPN patients and HPN patients older than 45 scored worse. CONCLUSION—Quality of life is reduced in patients on HPN compared with those with anatomical or functional short bowel not receiving HPN, and compares with that reported for patients with chronic renal failure treated by dialysis. Keywords: parenteral nutrition; quality of life; sickness impact profile; inflammatory bowel disease
Full Text
The Full Text of this article is available as a PDF (166.7 KB).
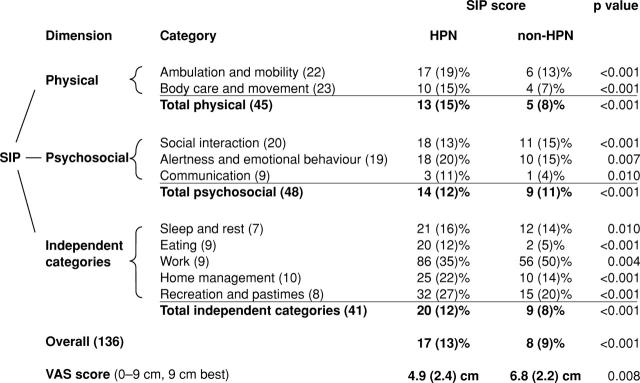
Figure 1 .
Comparison of SIP scores between patients receiving home parenteral nutrition (HPN) and those who did not. Results are expressed as mean (SD). Frequencies of confirmatory answers in the SIP questionnaire were compared between groups using the χ2 test or alternatively Fisher's exact test. The VAS scores were compared using a Mann-Whitney rank sum test. The values in parentheses in the category column give the numbers of items in each category. Zero per cent indicates the best possible function (absence of dysfunction), whereas 100% indicates presence of all possible dysfunctional behaviour.
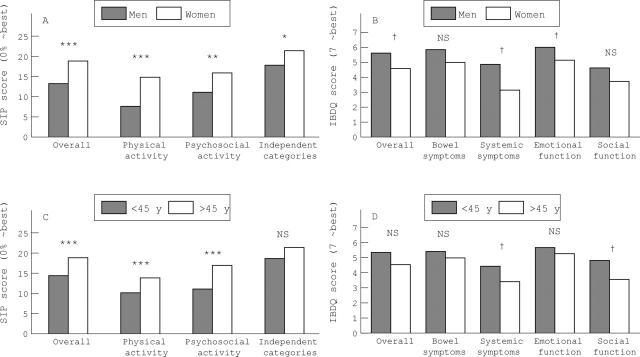
Figure 2 .
Mean sickness impact profile (SIP) scores and median inflammatory bowel disease questionnaire (IBDQ) scores according to sex (A and B) and age (C and D) in the patients on home parenteral nutrition (HPN). χ2 or Fisher exact test: *p<0.05; **p<0.01, ***p<0.001. Mann-Whitney rank sum test: †p<0.05.
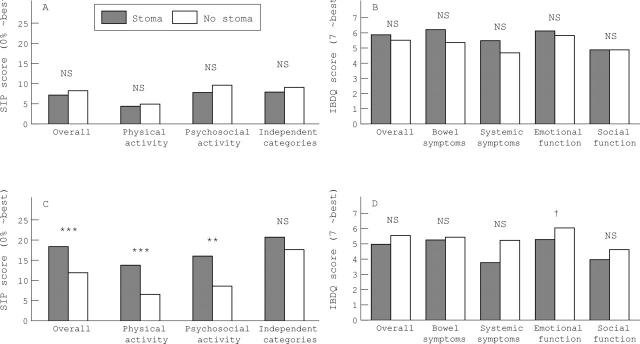
Figure 3 .
Mean sickness impact profile (SIP) scores and median inflammatory bowel disease questionnaire (IBDQ) scores according to the presence or absence of a stoma in patients not on home parenteral nutrition (HPN) (A and B) and those on HPN (C and D). χ2 or Fisher exact test: *p<0.05; **p<0.01; ***p<0.001. Mann-Whitney rank sum test: †p<0.01.
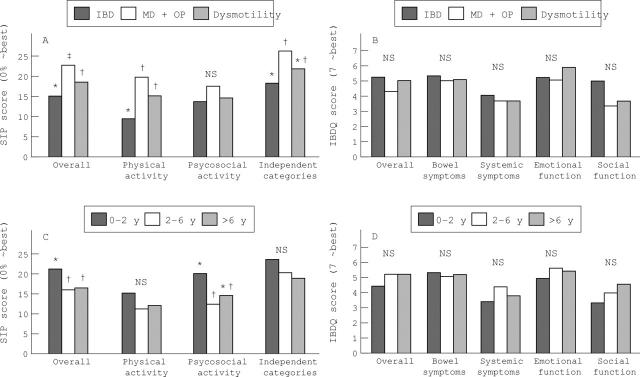
Figure 4 .
Mean sickness impact profile (SIP) scores and median inflammatory bowel disease questionnaire (IBDQ) scores according to diagnosis (A and B) and duration of home parenteral nutrition (HPN) (C and D). IBD, patients with inflammatory bowel disease; MD+OP, patients with intestinal resection because of mesenteric vascular disease or complications of intra-abdominal surgery; dysmotility, patients with intestinal dysmotility. *, † and ‡ denote significant difference (p<0.05) by the χ2 or Fisher exact test.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Abu-Elmagd K., Reyes J., Todo S., Rao A., Lee R., Irish W., Furukawa H., Bueno J., McMichael J., Fawzy A. T. Clinical intestinal transplantation: new perspectives and immunologic considerations. J Am Coll Surg. 1998 May;186(5):512–527. doi: 10.1016/s1072-7515(98)00083-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergner L., Hallstrom A. P., Bergner M., Eisenberg M. S., Cobb L. A. Health status of survivors of cardiac arrest and of myocardial infarction controls. Am J Public Health. 1985 Nov;75(11):1321–1323. doi: 10.2105/ajph.75.11.1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergner M., Bobbitt R. A., Carter W. B., Gilson B. S. The Sickness Impact Profile: development and final revision of a health status measure. Med Care. 1981 Aug;19(8):787–805. doi: 10.1097/00005650-198108000-00001. [DOI] [PubMed] [Google Scholar]
- Cummings J. H., James W. P., Wiggins H. S. Role of the colon in ileal-resection diarrhoea. Lancet. 1973 Feb 17;1(7799):344–347. doi: 10.1016/s0140-6736(73)90131-1. [DOI] [PubMed] [Google Scholar]
- Detsky A. S., McLaughlin J. R., Abrams H. B., L'Abbe K. A., Whitwell J., Bombardier C., Jeejeebhoy K. N. Quality of life of patients on long-term total parenteral nutrition at home. J Gen Intern Med. 1986 Jan-Feb;1(1):26–33. doi: 10.1007/BF02596321. [DOI] [PubMed] [Google Scholar]
- Grant D. Current results of intestinal transplantation. The International Intestinal Transplant Registry. Lancet. 1996 Jun 29;347(9018):1801–1803. doi: 10.1016/s0140-6736(96)91619-0. [DOI] [PubMed] [Google Scholar]
- Guyatt G., Mitchell A., Irvine E. J., Singer J., Williams N., Goodacre R., Tompkins C. A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterology. 1989 Mar;96(3):804–810. [PubMed] [Google Scholar]
- Jeppesen P. B., Staun M., Mortensen P. B. Adult patients receiving home parenteral nutrition in Denmark from 1991 to 1996: who will benefit from intestinal transplantation? Scand J Gastroenterol. 1998 Aug;33(8):839–846. doi: 10.1080/00365529850171503. [DOI] [PubMed] [Google Scholar]
- Ladefoged K. Quality of life in patients on permanent home parenteral nutrition. JPEN J Parenter Enteral Nutr. 1981 Mar-Apr;5(2):132–137. doi: 10.1177/0148607181005002132. [DOI] [PubMed] [Google Scholar]
- Laupacis A., Keown P., Pus N., Krueger H., Ferguson B., Wong C., Muirhead N. A study of the quality of life and cost-utility of renal transplantation. Kidney Int. 1996 Jul;50(1):235–242. doi: 10.1038/ki.1996.307. [DOI] [PubMed] [Google Scholar]
- Levy N. B., Wynbrandt G. D. The quality of life on maintenance haemodialysis. Lancet. 1975 Jun 14;1(7920):1328–1328. doi: 10.1016/s0140-6736(75)92329-6. [DOI] [PubMed] [Google Scholar]
- Messing B., Landais P., Goldfarb B., Irving M. Home parenteral nutrition in adults: a multicentre survey in Europe. Clin Nutr. 1989 Feb;8(1):3–9. doi: 10.1016/0261-5614(89)90018-6. [DOI] [PubMed] [Google Scholar]
- Nightingale J. M. The Sir David Cuthbertson Medal Lecture. Clinical problems of a short bowel and their treatment. Proc Nutr Soc. 1994 Jul;53(2):373–391. doi: 10.1079/pns19940043. [DOI] [PubMed] [Google Scholar]
- Price B. S., Levine E. L. Permanent total parenteral nutrition: psychological and social responses of the early stages. JPEN J Parenter Enteral Nutr. 1979 Mar-Apr;3(2):48–52. doi: 10.1177/014860717900300203. [DOI] [PubMed] [Google Scholar]
- Richards D. M., Irving M. H. Assessing the quality of life of patients with intestinal failure on home parenteral nutrition. Gut. 1997 Feb;40(2):218–222. doi: 10.1136/gut.40.2.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinovitch A. E. Home total parenteral nutrition: a psycho-social viewpoint. JPEN J Parenter Enteral Nutr. 1981 Nov-Dec;5(6):522–525. doi: 10.1177/0148607181005006522. [DOI] [PubMed] [Google Scholar]
- Schofield W. N. Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr. 1985;39 (Suppl 1):5–41. [PubMed] [Google Scholar]
- Temkin N., McLean A., Jr, Dikmen S., Gale J., Bergner M., Almes M. J. Development and evaluation of modifications to the Sickness Impact Profile for head injury. J Clin Epidemiol. 1988;41(1):47–57. doi: 10.1016/0895-4356(88)90008-x. [DOI] [PubMed] [Google Scholar]