Abstract
BACKGROUND—The ductus venosus connects the umbilical vein to the inferior vena cava during fetal life and subsequently closes rapidly after birth. It is known as patent ductus venosus when it remains patent in adulthood. PATIENTS—A 43 year old man with a history of panhypopituitarism presented with recurrent bouts of pedal oedema associated with fatigue, hypoalbuminaemia, and elevated prothrombin time. An ultrasound examination of his abdomen with Doppler revealed notable attenuation of the main portal vein with diminished intrahepatic branches; a computed tomography scan with angiography revealed a large collateral vein within the liver consistent with a patent ductus venosus. Sequential liver biopsies showed a considerable reduction in the calibre and number of the portal veins. His younger brother, who was diagnosed with alcohol related cirrhosis, suffered from intermittent bouts of encephalopathy and was found to have the same vascular lesion. A third brother was found to have a patent ductus venosus as well as two large hepatic masses consistent with focal nodular hyperplasia. CONCLUSION—The syndrome of familial patent ductus venosus has only previously been described in three infant brothers who presented with hepatic encephalopathy and fatty degeneration of the liver. This report documents three brothers with a patent ductus venosus presenting in adulthood with different manifestations of liver disease. The presence of the same vascular anomaly in three brothers is highly suggestive of a recessive genetic trait with an anatomical manifestation of patent ductus venosus. Keywords: patent ductus venosus; portal vein sclerosis; familial; hepatic synthetic dysfunction; hepatic encephalopathy
Full Text
The Full Text of this article is available as a PDF (113.0 KB).
Figure 1 .
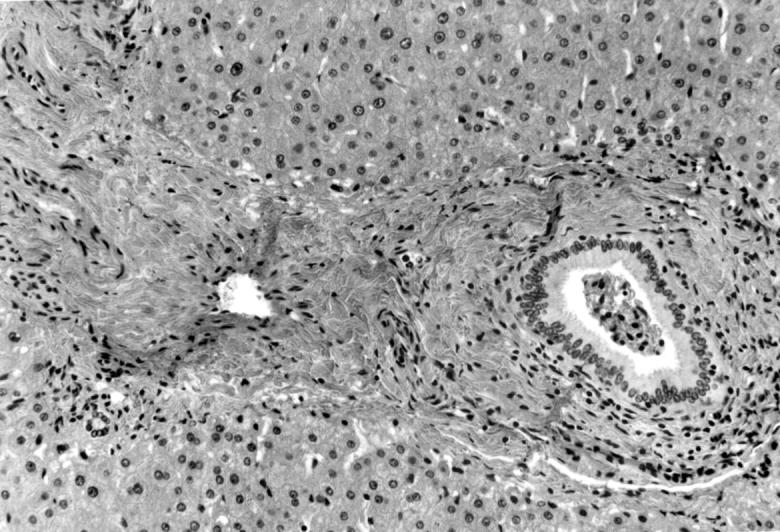
Microscopic section of the liver in patient 1, showing a sclerosed portal vein on the left of the portal triad (haematoxylin and eosin; original magnification × 100).
Figure 2 .

(A) Computed tomography of the abdomen of patient 1 during infusion of contrast into the superior mesenteric artery, showing the patent ductus venosus. The thin arrow points to the portal vein, the thick arrow to the patent ductus venosus, and the asterisk marks the inferior vena cava. (B) Selective angiogram of superior mesenteric artery of patient 1, showing the patent ductus venosus in the venous phase. The thin arrow points to the small residual right portal vein, the thick arrow to the patent ductus venosus, and the asterisk marks the right atrium.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adams P. C., Bradley C., Frei J. V. Hepatic iron and zinc concentrations after portacaval shunting for nonalcoholic cirrhosis. Hepatology. 1994 Jan;19(1):101–105. [PubMed] [Google Scholar]
- Baker A. L. Hepatotrophic factors: basic concepts and clinical implications. Acta Med Scand Suppl. 1985;703:201–208. doi: 10.1111/j.0954-6820.1985.tb08916.x. [DOI] [PubMed] [Google Scholar]
- Barsky M. F., Rankin R. N., Wall W. J., Ghent C. N., Garcia B. Patent ductus venosus: problems in assessment and management. Can J Surg. 1989 Jul;32(4):271–275. [PubMed] [Google Scholar]
- Chagnon S. F., Vallee C. A., Barge J., Chevalier L. J., Le Gal J., Blery M. V. Aneurysmal portahepatic venous fistula: report of two cases. Radiology. 1986 Jun;159(3):693–695. doi: 10.1148/radiology.159.3.3517953. [DOI] [PubMed] [Google Scholar]
- Feder J. N., Gnirke A., Thomas W., Tsuchihashi Z., Ruddy D. A., Basava A., Dormishian F., Domingo R., Jr, Ellis M. C., Fullan A. A novel MHC class I-like gene is mutated in patients with hereditary haemochromatosis. Nat Genet. 1996 Aug;13(4):399–408. doi: 10.1038/ng0896-399. [DOI] [PubMed] [Google Scholar]
- Howard E. R., Davenport M. Congenital extrahepatic portocaval shunts--the Abernethy malformation. J Pediatr Surg. 1997 Mar;32(3):494–497. doi: 10.1016/s0022-3468(97)90614-x. [DOI] [PubMed] [Google Scholar]
- Kerlan R. K., Jr, Sollenberger R. D., Palubinskas A. J., Raskin N. H., Callen P. W., Ehrenfeld W. K. Portal-systemic encephalopathy due to a congenital portocaval shunt. AJR Am J Roentgenol. 1982 Nov;139(5):1013–1015. doi: 10.2214/ajr.139.5.1013. [DOI] [PubMed] [Google Scholar]
- Mitchell I. M., Pollock J. C., Gibson A. A. Patent ductus venosus. Pediatr Cardiol. 1991 Jul;12(3):181–183. doi: 10.1007/BF02238528. [DOI] [PubMed] [Google Scholar]
- Morgan G., Superina R. Congenital absence of the portal vein: two cases and a proposed classification system for portasystemic vascular anomalies. J Pediatr Surg. 1994 Sep;29(9):1239–1241. doi: 10.1016/0022-3468(94)90812-5. [DOI] [PubMed] [Google Scholar]
- Ohnishi K., Hatano H., Nakayama T., Kohno K., Okuda K. An unusual portal-systemic shunt, most likely through a patent ductus venosus. A case report. Gastroenterology. 1983 Oct;85(4):962–965. [PubMed] [Google Scholar]
- Ohtomo K., Furui S., Saito M., Kokubo T., Itai Y., Iio M. Enormous intrahepatic communication between the portal vein and the hepatic vein. Clin Radiol. 1986 Sep;37(5):513–514. doi: 10.1016/s0009-9260(86)80085-x. [DOI] [PubMed] [Google Scholar]
- Orii T., Ohkohchi N., Kato H., Doi H., Hirano T., Sekiguchi S., Akamatsu Y., Satomi S. Liver transplantation for severe hypoxemia caused by patent ductus venosus. J Pediatr Surg. 1997 Dec;32(12):1795–1797. doi: 10.1016/s0022-3468(97)90539-x. [DOI] [PubMed] [Google Scholar]
- RASKIN N. H., PRICE J. B., FISHMAN R. A. PORTAL-SYSTEMIC ENCEPHALOPATHY DUE TO CONGENITAL INTRAHEPATIC SHUNTS. N Engl J Med. 1964 Jan 30;270:225–229. doi: 10.1056/NEJM196401302700503. [DOI] [PubMed] [Google Scholar]
- Raskin N. H., Bredesen D., Ehrenfeld W. K., Kerlan R. K. Periodic confusion caused by congenital extrahepatic portacaval shunt. Neurology. 1984 May;34(5):666–669. doi: 10.1212/wnl.34.5.666. [DOI] [PubMed] [Google Scholar]
- Rozga J., Jeppsson B., Bengmark S. Hepatotrophic factors in liver growth and atrophy. Br J Exp Pathol. 1985 Dec;66(6):669–678. [PMC free article] [PubMed] [Google Scholar]
- Starzl T. E., Francavilla A., Halgrimson C. G., Francavilla F. R., Porter K. A., Brown T. H., Putnam C. W. The origin, hormonal nature, and action of hepatotrophic substances in portal venous blood. Surg Gynecol Obstet. 1973 Aug;137(2):179–199. [PMC free article] [PubMed] [Google Scholar]
- Uchino T., Endo F., Ikeda S., Shiraki K., Sera Y., Matsuda I. Three brothers with progressive hepatic dysfunction and severe hepatic steatosis due to a patent ductus venosus. Gastroenterology. 1996 Jun;110(6):1964–1968. doi: 10.1053/gast.1996.v110.pm8964424. [DOI] [PubMed] [Google Scholar]
- Wanless I. R., Lentz J. S., Roberts E. A. Partial nodular transformation of liver in an adult with persistent ductus venosus. Review with hypothesis on pathogenesis. Arch Pathol Lab Med. 1985 May;109(5):427–432. [PubMed] [Google Scholar]
- Woodle E. S., Thistlethwaite J. R., Emond J. C., Whitington P. F., Vogelbach P., Yousefzadeh D. K., Broelsch C. E. Successful hepatic transplantation in congenital absence of recipient portal vein. Surgery. 1990 Apr;107(4):475–479. [PubMed] [Google Scholar]


