Abstract
BACKGROUND—Recent data have suggested that cardia biopsy specimens may be more reflective of gastro-oesophageal reflux disease (GORD) than squamous biopsy specimens. AIMS—To assess the distribution, severity, and types of mucosal injury in GORD. PATIENTS—Thirty patients with symptomatic GORD with no or minimal erosions. METHODS—Biopsies were performed at the squamocolumnar junction (Z-line) and 1-2 cm below the Z-line. Injury to the columnar mucosa was scored for inflammatory cells, epithelial cell abnormalities, and for the presence of intestinal metaplasia and Helicobacter pylori. A carditis score above 2 was considered positive (maximum score = 9). RESULTS—Mean carditis scores and percentages of patients with a positive carditis score were higher in Z-line biopsy specimens containing both squamous and columnar mucosa than in those with just columnar mucosa or in specimens taken 1-2 cm below the Z-line. Carditis at the Z-line was focal in 49% of the specimens and was always present adjacent to the squamous epithelium. Goblet cells were present more frequently in the specimens immediately at the Z-line than in those 1-2 cm below the Z-line. H pylori was present in only four patients. The mean carditis scores of specimens 1-2 cm below the Z-line in these patients was significantly higher than in those patients without H pylori. CONCLUSIONS—Mucosal injury at the gastric cardia is highly localised to the region adjacent to the squamocolumnar junction in patients with GORD. Morphological studies of the cardia in GORD should focus on tissue samples that contain both squamous and columnar epithelium in order to obtain an accurate picture of the spectrum of injury. Keywords: gastro-oesophageal reflux disease; Helicobacter pylori; cardia; Z-line; squamous epithelium; columnar epithelium
Full Text
The Full Text of this article is available as a PDF (92.8 KB).
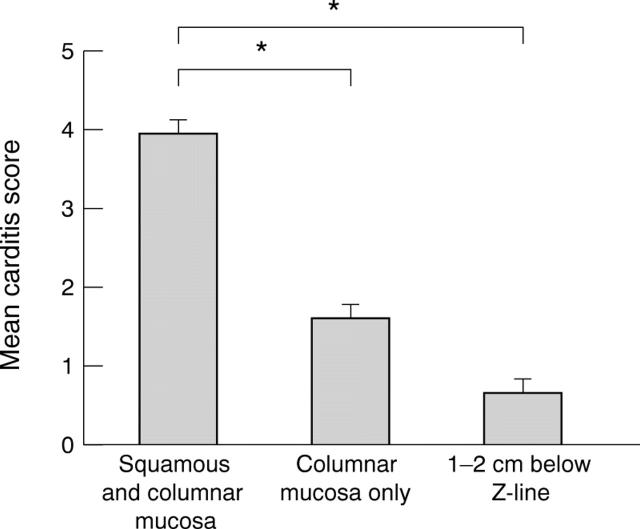
Figure 1 .
Mean carditis scores from biopsy specimens obtained in the gastric cardia.
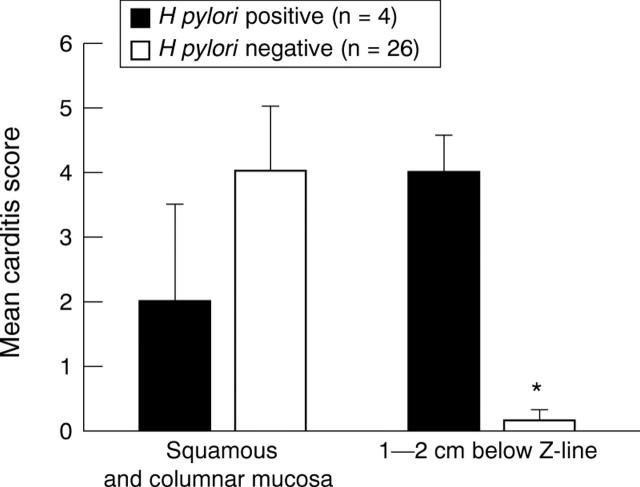
Figure 2 .
Relation of Helicobacter pylori status to mean carditis scores from biopsy specimens obtained at the Z-line, containing both squamous and columnar mucosa, and 1-2 cm below the Z-line. *p<0.05.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Antonioli D. A., Goldman H. Changes in the location and type of gastric adenocarcinoma. Cancer. 1982 Aug 15;50(4):775–781. doi: 10.1002/1097-0142(19820815)50:4<775::aid-cncr2820500425>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- Blot W. J., Devesa S. S., Fraumeni J. F., Jr Continuing climb in rates of esophageal adenocarcinoma: an update. JAMA. 1993 Sep 15;270(11):1320–1320. [PubMed] [Google Scholar]
- Blot W. J., Devesa S. S., Kneller R. W., Fraumeni J. F., Jr Rising incidence of adenocarcinoma of the esophagus and gastric cardia. JAMA. 1991 Mar 13;265(10):1287–1289. [PubMed] [Google Scholar]
- Cameron A. J., Lomboy C. T., Pera M., Carpenter H. A. Adenocarcinoma of the esophagogastric junction and Barrett's esophagus. Gastroenterology. 1995 Nov;109(5):1541–1546. doi: 10.1016/0016-5085(95)90642-8. [DOI] [PubMed] [Google Scholar]
- Genta R. M., Huberman R. M., Graham D. Y. The gastric cardia in Helicobacter pylori infection. Hum Pathol. 1994 Sep;25(9):915–919. doi: 10.1016/0046-8177(94)90011-6. [DOI] [PubMed] [Google Scholar]
- Goldblum J. R., Vicari J. J., Falk G. W., Rice T. W., Peek R. M., Easley K., Richter J. E. Inflammation and intestinal metaplasia of the gastric cardia: the role of gastroesophageal reflux and H. pylori infection. Gastroenterology. 1998 Apr;114(4):633–639. doi: 10.1016/s0016-5085(98)70576-1. [DOI] [PubMed] [Google Scholar]
- Hirota W. K., Loughney T. M., Lazas D. J., Maydonovitch C. L., Rholl V., Wong R. K. Specialized intestinal metaplasia, dysplasia, and cancer of the esophagus and esophagogastric junction: prevalence and clinical data. Gastroenterology. 1999 Feb;116(2):277–285. doi: 10.1016/s0016-5085(99)70123-x. [DOI] [PubMed] [Google Scholar]
- Johnson L. F., Demeester T. R. Twenty-four-hour pH monitoring of the distal esophagus. A quantitative measure of gastroesophageal reflux. Am J Gastroenterol. 1974 Oct;62(4):325–332. [PubMed] [Google Scholar]
- Johnston M. H., Hammond A. S., Laskin W., Jones D. M. The prevalence and clinical characteristics of short segments of specialized intestinal metaplasia in the distal esophagus on routine endoscopy. Am J Gastroenterol. 1996 Aug;91(8):1507–1511. [PubMed] [Google Scholar]
- Locke G. R., 3rd, Talley N. J., Carpenter H. A., Harmsen W. S., Zinsmeister A. R., Melton L. J., 3rd Changes in the site- and histology-specific incidence of gastric cancer during a 50-year period. Gastroenterology. 1995 Dec;109(6):1750–1756. doi: 10.1016/0016-5085(95)90740-8. [DOI] [PubMed] [Google Scholar]
- Masclee A. A., de Best A. C., de Graaf R., Cluysenaer O. J., Jansen J. B. Ambulatory 24-hour pH-metry in the diagnosis of gastroesophageal reflux disease. Determination of criteria and relation to endoscopy. Scand J Gastroenterol. 1990 Mar;25(3):225–230. [PubMed] [Google Scholar]
- Mattioli S., Pilotti V., Spangaro M., Grigioni W. F., Zannoli R., Felice V., Conci A., Gozzetti G. Reliability of 24-hour home esophageal pH monitoring in diagnosis of gastroesophageal reflux. Dig Dis Sci. 1989 Jan;34(1):71–78. doi: 10.1007/BF01536157. [DOI] [PubMed] [Google Scholar]
- Meyers W. C., Damiano R. J., Jr, Rotolo F. S., Postlethwait R. W. Adenocarcinoma of the stomach. Changing patterns over the last 4 decades. Ann Surg. 1987 Jan;205(1):1–8. doi: 10.1097/00000658-198701000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales T. G., Sampliner R. E., Bhattacharyya A. Intestinal metaplasia of the gastric cardia. Am J Gastroenterol. 1997 Mar;92(3):414–418. [PubMed] [Google Scholar]
- Nandurkar S., Talley N. J., Martin C. J., Ng T. H., Adams S. Short segment Barrett's oesophagus: prevalence, diagnosis and associations. Gut. 1997 Jun;40(6):710–715. doi: 10.1136/gut.40.6.710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oberg S., Peters J. H., DeMeester T. R., Chandrasoma P., Hagen J. A., Ireland A. P., Ritter M. P., Mason R. J., Crookes P., Bremner C. G. Inflammation and specialized intestinal metaplasia of cardiac mucosa is a manifestation of gastroesophageal reflux disease. Ann Surg. 1997 Oct;226(4):522–532. doi: 10.1097/00000658-199710000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pera M., Cameron A. J., Trastek V. F., Carpenter H. A., Zinsmeister A. R. Increasing incidence of adenocarcinoma of the esophagus and esophagogastric junction. Gastroenterology. 1993 Feb;104(2):510–513. doi: 10.1016/0016-5085(93)90420-h. [DOI] [PubMed] [Google Scholar]
- Riddell R. H. The biopsy diagnosis of gastroesophageal reflux disease, "carditis," and Barrett's esophagus, and sequelae of therapy. Am J Surg Pathol. 1996;20 (Suppl 1):S31–S50. doi: 10.1097/00000478-199600001-00005. [DOI] [PubMed] [Google Scholar]
- Schnell T. G., Sontag S. J., Chejfec G. Adenocarcinomas arising in tongues or short segments of Barrett's esophagus. Dig Dis Sci. 1992 Jan;37(1):137–143. doi: 10.1007/BF01308357. [DOI] [PubMed] [Google Scholar]
- Spechler S. J., Zeroogian J. M., Antonioli D. A., Wang H. H., Goyal R. K. Prevalence of metaplasia at the gastro-oesophageal junction. Lancet. 1994 Dec 3;344(8936):1533–1536. doi: 10.1016/s0140-6736(94)90349-2. [DOI] [PubMed] [Google Scholar]
- Vitale G. C., Cheadle W. G., Sadek S., Michel M. E., Cuschieri A. Computerized 24-hour ambulatory esophageal pH monitoring and esophagogastroduodenoscopy in the reflux patient. A comparative study. Ann Surg. 1984 Dec;200(6):724–728. doi: 10.1097/00000658-198412000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein W. M., Bogoch E. R., Bowes K. L. The normal human esophageal mucosa: a histological reappraisal. Gastroenterology. 1975 Jan;68(1):40–44. [PubMed] [Google Scholar]
- Weinstein W. M. Precursor lesions for cancer of the cardia. Gastrointest Endosc Clin N Am. 1997 Jan;7(1):19–28. [PubMed] [Google Scholar]
- Wolf B. C., Khettry U., Leonardi H. K., Neptune W. B., Bhattacharyya A. K., Legg M. A. Benign lesions mimicking malignant tumors of the esophagus. Hum Pathol. 1988 Feb;19(2):148–154. doi: 10.1016/s0046-8177(88)80342-3. [DOI] [PubMed] [Google Scholar]