Abstract
BACKGROUND/AIMS—Intestinal metaplasia (IM) is a common finding at the oesophagogastric junction, but the aetiopathogenesis of the different IM subtypes—that is, incomplete IM (specialised columnar epithelium, SCE) and complete IM— and their associations with gastro-oesophageal reflux disease and Helicobacter pylori gastritis are unclear. METHODS—1058 consecutive dyspeptic patients undergoing gastroscopy were enrolled. The gastric, oesophagogastric junctional, and oesophageal biopsy specimens obtained were stained with haematoxylin and eosin, alcian blue (pH 2.5)-periodic acid Schiff, and modified Giemsa. RESULTS—Complete junctional IM was detected in 196 (19%) of the 1058 subjects, and in 134 (13%) was the sole IM subtype. Incomplete junctional IM (SCE) was detected in 101 (10%) subjects, of whom 62 (61%) also had the complete IM subtype. Of patients with normal gastric histology (n = 426), 6% had complete IM and 7% junctional SCE. The prevalence of both types of IM increased with age in patients with either normal gastric histology or chronic gastritis (n = 611). Epithelial dysplasia was not detected in any patients with junctional IM. In multivariate analysis, independent risk factors for incomplete junctional IM were age (odds ratio (OR) 1.3 per decade, 95% confidence interval (CI) 1.2 to 1.6), endoscopic erosive oesophagitis (OR 1.9, 95% CI 1.1 to 3.2), and chronic cardia inflammation (OR 2.9, 95% CI 1.3 to 6.2), but not gastric H pylori infection (OR 1.0, 95% CI 0.6 to 1.7). In univariate analysis, junctional incomplete IM was not associated with cardia H pylori infection. Independent risk factors for "pure" complete junctional IM (n = 134) were age (OR 1.2 per decade, 95% CI 1.0 to 1.4), antral predominant non-atrophic gastritis (OR 2.6, 95% CI 1.3 to 5.2), antral predominant atrophic gastritis (OR 2.1, 95% CI 1.1 to 5.2), and multifocal atrophic gastritis (OR 7.1, 95% CI 2.5 to 19.8). In univariate analysis, junctional complete IM was strongly associated with chronic cardia inflammation and cardia H pylori infection (p<0.001). CONCLUSIONS—Both complete and incomplete junctional IM are independent acquired lesions that increase in prevalence with age. Although IM subtypes often occur simultaneously, they show remarkable differences in their associations with gastritis and erosive oesophagitis: junctional complete IM is a manifestation of multifocal atrophic gastritis, while the incomplete form (SCE) may result from carditis and gastro-oesophageal reflux disease. The frequency of dysplasia in intestinal metaplasia at the oesophagogastric junction appears to be low. Keywords: intestinal metaplasia; oesophagogastric junction; oesophagitis; gastritis; gastro-oesophageal reflux disease; Helicobacter pylori
Full Text
The Full Text of this article is available as a PDF (112.2 KB).
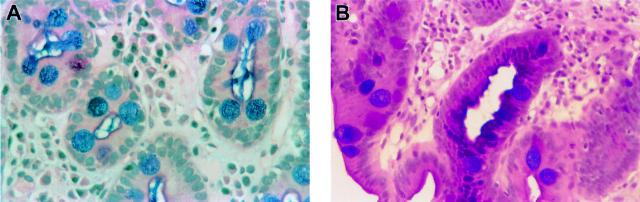
Figure 1 .
Complete intestinal metaplasia (IM) is characterised by goblet cells stained red or blue by alcian blue (pH 2.5)-periodic acid Schiff stain and by the presence of absorptive non-goblet cells (A). Incomplete IM or specialised columnar epithelium is differentiated from the complete IM subtype by the presence of goblet cells intermixed with mucin-secreting columnar-appearing non-goblet cells staining red and blue by the alcian blue (pH 2.5)-periodic acid Schiff stain (B).
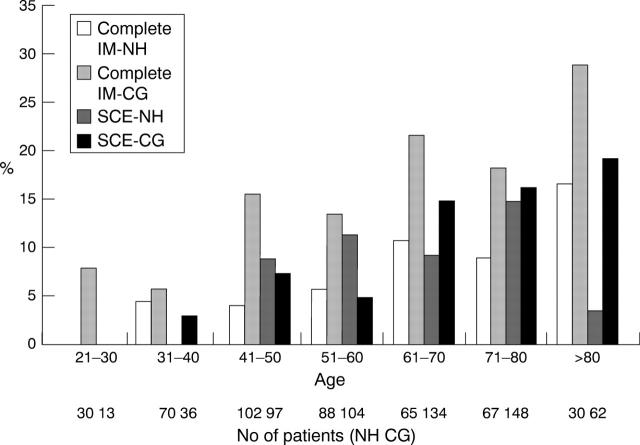
Figure 2 .
Prevalences of junctional complete and incomplete (specialised columnar epithelium, SCE) intestinal metaplasia (IM) in different age groups. NH, normal gastric histology (n = 426); CG, chronic gastritis (n = 632). The correlation of age with both IM types was significant in the CG (p<0.001 for complete IM and incomplete IM) and NH (p = 0.001 for complete IM and p = 0.002 for incomplete IM) group.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Blot W. J., Devesa S. S., Kneller R. W., Fraumeni J. F., Jr Rising incidence of adenocarcinoma of the esophagus and gastric cardia. JAMA. 1991 Mar 13;265(10):1287–1289. [PubMed] [Google Scholar]
- Cameron A. J., Lomboy C. T., Pera M., Carpenter H. A. Adenocarcinoma of the esophagogastric junction and Barrett's esophagus. Gastroenterology. 1995 Nov;109(5):1541–1546. doi: 10.1016/0016-5085(95)90642-8. [DOI] [PubMed] [Google Scholar]
- Correa P. A human model of gastric carcinogenesis. Cancer Res. 1988 Jul 1;48(13):3554–3560. [PubMed] [Google Scholar]
- Filipe M. I., Potet F., Bogomoletz W. V., Dawson P. A., Fabiani B., Chauveinc P., Fenzy A., Gazzard B., Goldfain D., Zeegen R. Incomplete sulphomucin-secreting intestinal metaplasia for gastric cancer. Preliminary data from a prospective study from three centres. Gut. 1985 Dec;26(12):1319–1326. doi: 10.1136/gut.26.12.1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuchs C. S., Mayer R. J. Gastric carcinoma. N Engl J Med. 1995 Jul 6;333(1):32–41. doi: 10.1056/NEJM199507063330107. [DOI] [PubMed] [Google Scholar]
- Genta R. M., Huberman R. M., Graham D. Y. The gastric cardia in Helicobacter pylori infection. Hum Pathol. 1994 Sep;25(9):915–919. doi: 10.1016/0046-8177(94)90011-6. [DOI] [PubMed] [Google Scholar]
- Gottfried M. R., McClave S. A., Boyce H. W. Incomplete intestinal metaplasia in the diagnosis of columnar lined esophagus (Barrett's esophagus). Am J Clin Pathol. 1989 Dec;92(6):741–746. doi: 10.1093/ajcp/92.6.741. [DOI] [PubMed] [Google Scholar]
- Haggitt R. C. Barrett's esophagus, dysplasia, and adenocarcinoma. Hum Pathol. 1994 Oct;25(10):982–993. doi: 10.1016/0046-8177(94)90057-4. [DOI] [PubMed] [Google Scholar]
- Hansson L. E., Sparén P., Nyrén O. Increasing incidence of carcinoma of the gastric cardia in Sweden from 1970 to 1985. Br J Surg. 1993 Mar;80(3):374–377. doi: 10.1002/bjs.1800800338. [DOI] [PubMed] [Google Scholar]
- Jass J. R. Role of intestinal metaplasia in the histogenesis of gastric carcinoma. J Clin Pathol. 1980 Sep;33(9):801–810. doi: 10.1136/jcp.33.9.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jauregui H. O., Davessar K., Hale J. H., Kessimian N., Cenoz C. Mucin histochemistry of intestinal metaplasia in Barrett's esophagus. Mod Pathol. 1988 May;1(3):188–192. [PubMed] [Google Scholar]
- Johnston M. H., Hammond A. S., Laskin W., Jones D. M. The prevalence and clinical characteristics of short segments of specialized intestinal metaplasia in the distal esophagus on routine endoscopy. Am J Gastroenterol. 1996 Aug;91(8):1507–1511. [PubMed] [Google Scholar]
- McClave S. A., Boyce H. W., Jr, Gottfried M. R. Early diagnosis of columnar-lined esophagus: a new endoscopic diagnostic criterion. Gastrointest Endosc. 1987 Dec;33(6):413–416. doi: 10.1016/s0016-5107(87)71676-9. [DOI] [PubMed] [Google Scholar]
- Morales T. G., Sampliner R. E., Bhattacharyya A. Intestinal metaplasia of the gastric cardia. Am J Gastroenterol. 1997 Mar;92(3):414–418. [PubMed] [Google Scholar]
- Nandurkar S., Talley N. J., Martin C. J., Ng T. H., Adams S. Short segment Barrett's oesophagus: prevalence, diagnosis and associations. Gut. 1997 Jun;40(6):710–715. doi: 10.1136/gut.40.6.710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oberg S., Peters J. H., DeMeester T. R., Chandrasoma P., Hagen J. A., Ireland A. P., Ritter M. P., Mason R. J., Crookes P., Bremner C. G. Inflammation and specialized intestinal metaplasia of cardiac mucosa is a manifestation of gastroesophageal reflux disease. Ann Surg. 1997 Oct;226(4):522–532. doi: 10.1097/00000658-199710000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owen D. A. Normal histology of the stomach. Am J Surg Pathol. 1986 Jan;10(1):48–61. doi: 10.1097/00000478-198601000-00006. [DOI] [PubMed] [Google Scholar]
- Pera M., Cameron A. J., Trastek V. F., Carpenter H. A., Zinsmeister A. R. Increasing incidence of adenocarcinoma of the esophagus and esophagogastric junction. Gastroenterology. 1993 Feb;104(2):510–513. doi: 10.1016/0016-5085(93)90420-h. [DOI] [PubMed] [Google Scholar]
- Price A. B. The Sydney System: histological division. J Gastroenterol Hepatol. 1991 May-Jun;6(3):209–222. doi: 10.1111/j.1440-1746.1991.tb01468.x. [DOI] [PubMed] [Google Scholar]
- Riddell R. H. The biopsy diagnosis of gastroesophageal reflux disease, "carditis," and Barrett's esophagus, and sequelae of therapy. Am J Surg Pathol. 1996;20 (Suppl 1):S31–S50. doi: 10.1097/00000478-199600001-00005. [DOI] [PubMed] [Google Scholar]
- Shah K. A., Deacon A. J., Dunscombe P., Price A. B. Intestinal metaplasia subtyping: evaluation of Gomori's aldehyde fuchsin for routine diagnostic use. Histopathology. 1997 Sep;31(3):277–283. doi: 10.1046/j.1365-2559.1997.2110847.x. [DOI] [PubMed] [Google Scholar]
- Spechler S. J., Zeroogian J. M., Antonioli D. A., Wang H. H., Goyal R. K. Prevalence of metaplasia at the gastro-oesophageal junction. Lancet. 1994 Dec 3;344(8936):1533–1536. doi: 10.1016/s0140-6736(94)90349-2. [DOI] [PubMed] [Google Scholar]
- Trudgill N. J., Suvarna S. K., Kapur K. C., Riley S. A. Intestinal metaplasia at the squamocolumnar junction in patients attending for diagnostic gastroscopy. Gut. 1997 Nov;41(5):585–589. doi: 10.1136/gut.41.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tytgat G. N., Hameeteman W., Onstenk R., Schotborg R. The spectrum of columnar-lined esophagus--Barrett's esophagus. Endoscopy. 1989 Jul;21(4):177–185. doi: 10.1055/s-2007-1012937. [DOI] [PubMed] [Google Scholar]
- Weinstein W. M., Ippoliti A. F. The diagnosis of Barrett's esophagus: goblets, goblets, goblets. Gastrointest Endosc. 1996 Jul;44(1):91–95. doi: 10.1016/s0016-5107(96)70239-0. [DOI] [PubMed] [Google Scholar]
- Weston A. P., Krmpotich P., Makdisi W. F., Cherian R., Dixon A., McGregor D. H., Banerjee S. K. Short segment Barrett's esophagus: clinical and histological features, associated endoscopic findings, and association with gastric intestinal metaplasia. Am J Gastroenterol. 1996 May;91(5):981–986. [PubMed] [Google Scholar]