Abstract
BACKGROUND AND AIMS—Little is known about the prevalence, symptoms, diagnosis, attitude, and referral to specialists of patients with irritable bowel syndrome (IBS) in general practice. This study aimed to determine these characteristics. METHODS—3111 patients attending 36 general practitioners (GPs) at six varied locations in and near Bristol, UK, were screened to identify those with a gastrointestinal problem. These patients (n=255) and their doctors were given questionnaires. Six months later the case notes were examined to reach criteria based diagnoses of functional bowel disorders. RESULTS—Of 255 patients with a gastrointestinal complaint, 30% were judged to have IBS and 14% other functional disorders. Compared with 100 patients with an "organic" diagnoses, those with IBS were more often women and more often judged by their GP to be polysymptomatic and to have unexplained symptoms. The majority of patients with IBS (58%) were diagnosed as such by the GP; 22% had other functional diagnoses. Conversely, among 54 patients diagnosed as having IBS by the GPs, the criteria based diagnosis was indeed functional in 91%; only one patient had organic disease (proctitis). More patients with IBS than those with organic disease feared cancer. In most some fear remained after the visit to the doctor. On logistic regression analysis, predictors of referral to a specialist (29% referred) were denial of a role for stress, multiple tests, and frequent bowel movements. CONCLUSIONS—Half the patients with gut complaints seen by GPs have functional disorders. These are usually recognised, and few patients are referred. In IBS, cancer fears often remain, suggesting unconfident diagnosis or inadequate explanation. Keywords: irritable bowel syndrome; general practice; primary care; gut complaints; functional bowel disease; referral; health care seeking behaviour
Full Text
The Full Text of this article is available as a PDF (96.9 KB).
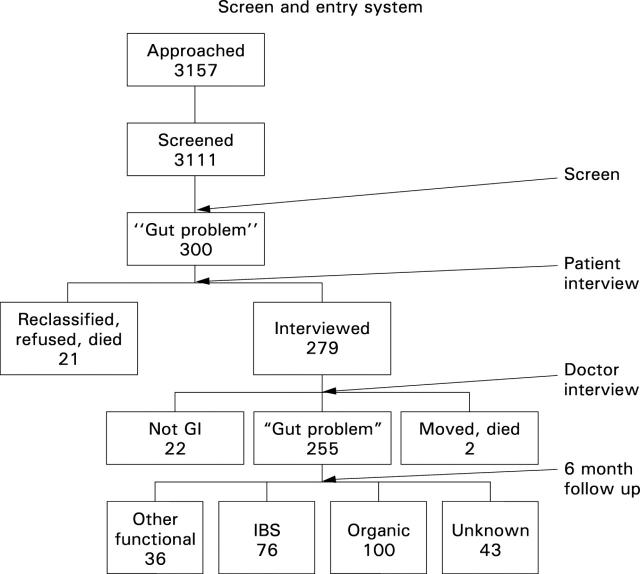
Figure 1 .
Results of approaching 3157 adults who attended their general practitioners in six English locations and further studying the 255 who had a gastrointestinal problem.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Crean G. P., Holden R. J., Knill-Jones R. P., Beattie A. D., James W. B., Marjoribanks F. M., Spiegelhalter D. J. A database on dyspepsia. Gut. 1994 Feb;35(2):191–202. doi: 10.1136/gut.35.2.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hislop I. G. Psychological significance of the irritable colon syndrome. Gut. 1971 Jun;12(6):452–457. doi: 10.1136/gut.12.6.452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kettell J., Jones R., Lydeard S. Reasons for consultation in irritable bowel syndrome: symptoms and patient characteristics. Br J Gen Pract. 1992 Nov;42(364):459–461. [PMC free article] [PubMed] [Google Scholar]
- Kruis W., Thieme C., Weinzierl M., Schüssler P., Holl J., Paulus W. A diagnostic score for the irritable bowel syndrome. Its value in the exclusion of organic disease. Gastroenterology. 1984 Jul;87(1):1–7. [PubMed] [Google Scholar]
- Lydiard R. B., Laraia M. T., Howell E. F., Ballenger J. C. Can panic disorder present as irritable bowel syndrome? J Clin Psychiatry. 1986 Sep;47(9):470–473. [PubMed] [Google Scholar]
- Manning A. P., Thompson W. G., Heaton K. W., Morris A. F. Towards positive diagnosis of the irritable bowel. Br Med J. 1978 Sep 2;2(6138):653–654. doi: 10.1136/bmj.2.6138.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald I. G., Daly J., Jelinek V. M., Panetta F., Gutman J. M. Opening Pandora's box: the unpredictability of reassurance by a normal test result. BMJ. 1996 Aug 10;313(7053):329–332. doi: 10.1136/bmj.313.7053.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker S., Knoll J. L., 3rd Partial hospitalization: an update. Am J Psychiatry. 1990 Feb;147(2):156–160. doi: 10.1176/ajp.147.2.156. [DOI] [PubMed] [Google Scholar]
- Thompson W. G., Heaton K. W., Smyth G. T., Smyth C. Irritable bowel syndrome: the view from general practice. Eur J Gastroenterol Hepatol. 1997 Jul;9(7):689–692. doi: 10.1097/00042737-199707000-00008. [DOI] [PubMed] [Google Scholar]
- Whitehead W. E., Burnett C. K., Cook E. W., 3rd, Taub E. Impact of irritable bowel syndrome on quality of life. Dig Dis Sci. 1996 Nov;41(11):2248–2253. doi: 10.1007/BF02071408. [DOI] [PubMed] [Google Scholar]
- Whorwell P. J., McCallum M., Creed F. H., Roberts C. T. Non-colonic features of irritable bowel syndrome. Gut. 1986 Jan;27(1):37–40. doi: 10.1136/gut.27.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young S. J., Alpers D. H., Norland C. C., Woodruff R. A., Jr Psychiatric illness and the irritable bowel syndrome. Practical implications for the primary physician. Gastroenterology. 1976 Feb;70(2):162–166. [PubMed] [Google Scholar]
- van der Horst H. E., van Dulmen A. M., Schellevis F. G., van Eijk J. T., Fennis J. F., Bleijenberg G. Do patients with irritable bowel syndrome in primary care really differ from outpatients with irritable bowel syndrome? Gut. 1997 Nov;41(5):669–674. doi: 10.1136/gut.41.5.669. [DOI] [PMC free article] [PubMed] [Google Scholar]