Abstract
BACKGROUND AND AIMS—Intestinal failure defined by the minimal energy and wet weight absorption required to avoid home parenteral nutrition (HPN) is not well described. Thus the aim of this study was to identify the minimal level of gut function necessary to avoid parenteral support using objective measurements of intestinal function. METHODS—Energy (bomb calorimetry) and wet weight absorption were measured during 48 hour balance studies in 45 HPN patients with intestinal failure and in 44 non-HPN borderline patients with a short bowel or malabsorption exceeding 2 MJ/day. RESULTS—In the non-HPN patients, the lower 5% confidence interval of the absorption of energy was 84% of the basal metabolic rate (BMR, the Harris-Benedict equations), equivalent to 4.9 MJ/day. Wet weight absorption was 1.4 kg/day. The HPN patients absorbed less of either or both. The non-HPN patients absorbed 24-86% (range) of the energy and 23-95% of the wet weight. Absorption in the HPN patients ranged from below 0% (net secretion) in patients with very short bowels to 100% absorption of an insufficient oral intake in patients with pseudo-obstruction. Non-HPN patients who absorbed less than half of their intake avoided HPN by hyperphagia (200-400% of BMR equivalent to 10-24 MJ/day, and 3-7 kg/day of wet weight). CONCLUSION—Intestinal failure was accurately measured as absorption below 1.4 kg/day of wet weight and 84% of the calculated BMR (depending on weight, sex and age), which is equal to 4.9 MJ/day. Intestinal absorption, expressed as a percentage of intake, did not discriminate between patients with and without intestinal failure, except for patients who absorbed less than 25% of their intake. Keywords: absorption; intestinal failure; energy; wet weight; short bowel syndrome
Full Text
The Full Text of this article is available as a PDF (156.3 KB).
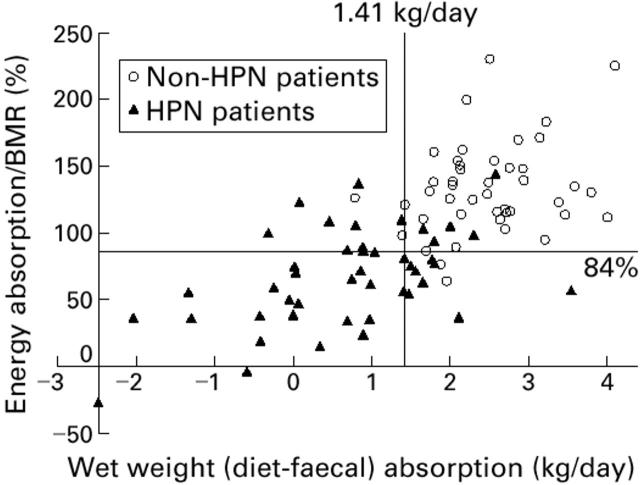
Figure 1 .
Absorption of wet weight and energy in relation to basal metabolic rate (BMR) calculated by the Harris-Benedict equations in 44 non-HPN patients and in 45 HPN patients. The 5% confidence limits of the non-HPN patients, defining intestinal failure, are given by the lines. Energy absorption/BMR was 84% and wet weight absorption 1.41 kg/day.
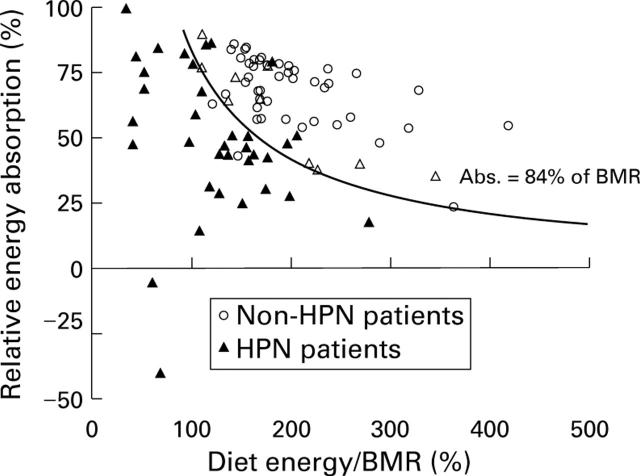
Figure 2 .
Relative energy absorption in relation to dietary energy intake/basal metabolic rate (BMR) in 44 non-HPN patients and 45 HPN patients. The open triangles indicate HPN patients who received HPN due to a wet weight absorption of less than the 5% limit (1.41 kg/day).
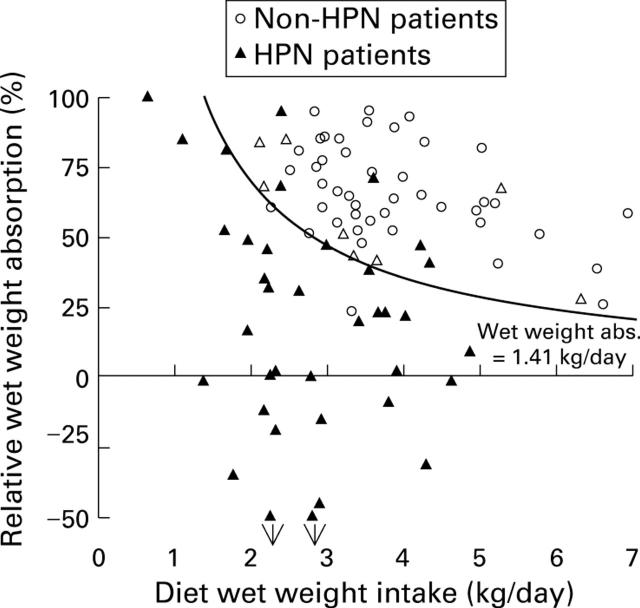
Figure 3 .
Relative wet weight absorption in relation to the dietary wet weight intake in 44 non-HPN patients and 45 HPN patients. The open triangles indicate HPN patients who received HPN because of energy absorption less than the 5% limit for basal metabolic rate (BMR) (84%).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Carbonnel F., Cosnes J., Chevret S., Beaugerie L., Ngô Y., Malafosse M., Parc R., Le Quintrec Y., Gendre J. P. The role of anatomic factors in nutritional autonomy after extensive small bowel resection. JPEN J Parenter Enteral Nutr. 1996 Jul-Aug;20(4):275–280. doi: 10.1177/0148607196020004275. [DOI] [PubMed] [Google Scholar]
- Cosnes J., Lamy P., Beaugerie L., Le Quintrec M., Gendre J. P., Le Quintrec Y. Adaptive hyperphagia in patients with postsurgical malabsorption. Gastroenterology. 1990 Dec;99(6):1814–1819. doi: 10.1016/0016-5085(90)90492-j. [DOI] [PubMed] [Google Scholar]
- Cummings J. H., James W. P., Wiggins H. S. Role of the colon in ileal-resection diarrhoea. Lancet. 1973 Feb 17;1(7799):344–347. doi: 10.1016/s0140-6736(73)90131-1. [DOI] [PubMed] [Google Scholar]
- DiCecco S., Nelson J., Burnes J., Fleming C. R. Nutritional intake of gut failure patients on home parenteral nutrition. JPEN J Parenter Enteral Nutr. 1987 Nov-Dec;11(6):529–532. doi: 10.1177/0148607187011006529. [DOI] [PubMed] [Google Scholar]
- Gouttebel M. C., Saint-Aubert B., Astre C., Joyeux H. Total parenteral nutrition needs in different types of short bowel syndrome. Dig Dis Sci. 1986 Jul;31(7):718–723. doi: 10.1007/BF01296449. [DOI] [PubMed] [Google Scholar]
- Jeppesen P. B., Staun M., Mortensen P. B. Adult patients receiving home parenteral nutrition in Denmark from 1991 to 1996: who will benefit from intestinal transplantation? Scand J Gastroenterol. 1998 Aug;33(8):839–846. doi: 10.1080/00365529850171503. [DOI] [PubMed] [Google Scholar]
- Krahn D. D., Rock C., Dechert R. E., Nairn K. K., Hasse S. A. Changes in resting energy expenditure and body composition in anorexia nervosa patients during refeeding. J Am Diet Assoc. 1993 Apr;93(4):434–438. doi: 10.1016/0002-8223(93)92291-5. [DOI] [PubMed] [Google Scholar]
- Messing B., Pigot F., Rongier M., Morin M. C., Ndeïndoum U., Rambaud J. C. Intestinal absorption of free oral hyperalimentation in the very short bowel syndrome. Gastroenterology. 1991 Jun;100(6):1502–1508. doi: 10.1016/0016-5085(91)90645-2. [DOI] [PubMed] [Google Scholar]
- Nightingale J. M., Lennard-Jones J. E., Gertner D. J., Wood S. R., Bartram C. I. Colonic preservation reduces need for parenteral therapy, increases incidence of renal stones, but does not change high prevalence of gall stones in patients with a short bowel. Gut. 1992 Nov;33(11):1493–1497. doi: 10.1136/gut.33.11.1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nightingale J. M., Lennard-Jones J. E., Walker E. R., Farthing M. J. Jejunal efflux in short bowel syndrome. Lancet. 1990 Sep 29;336(8718):765–768. doi: 10.1016/0140-6736(90)93238-k. [DOI] [PubMed] [Google Scholar]
- Rodrigues C. A., Lennard-Jones J. E., Thompson D. G., Farthing M. J. Energy absorption as a measure of intestinal failure in the short bowel syndrome. Gut. 1989 Feb;30(2):176–183. doi: 10.1136/gut.30.2.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schebendach J. E., Golden N. H., Jacobson M. S., Hertz S., Shenker I. R. The metabolic responses to starvation and refeeding in adolescents with anorexia nervosa. Ann N Y Acad Sci. 1997 May 28;817:110–119. doi: 10.1111/j.1749-6632.1997.tb48200.x. [DOI] [PubMed] [Google Scholar]
- Schofield W. N. Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr. 1985;39 (Suppl 1):5–41. [PubMed] [Google Scholar]
- Vaisman N., Rossi M. F., Goldberg E., Dibden L. J., Wykes L. J., Pencharz P. B. Energy expenditure and body composition in patients with anorexia nervosa. J Pediatr. 1988 Nov;113(5):919–924. doi: 10.1016/s0022-3476(88)80032-5. [DOI] [PubMed] [Google Scholar]