Abstract
BACKGROUND AND AIMS—Assessing the presence and degree of intestinal inflammation objectively, simply, and reliably is a significant problem in gastroenterology. We assessed faecal excretion of calprotectin, a stable neutrophil specific marker, as an index of intestinal inflammation and its potential use as a screening test to discriminate between patients with Crohn's disease and those with irritable bowel syndrome. METHODS—The validity of faecal calprotectin as a marker of intestinal inflammation was assessed in 22 patients with Crohn's disease (35 studies) by comparing faecal excretions and concentrations using four day faecal excretion of 111indium white cells. A cross sectional study assessed the sensitivity of faecal calprotectin concentration for the detection of established Crohn's disease (n=116). A prospective study assessed the value of faecal calprotectin in discriminating between patients with Crohn's disease and irritable bowel syndrome in 220 patients referred to a gastroenterology clinic. RESULTS—Four day faecal excretion of 111indium (median 8.7%; 95% confidence interval (CI) 7-17%; normal <1.0%) correlated significantly (p<0.0001) with daily (median ranged from 39 to 47 mg; normal <3 mg; r=0.76-0.82) and four day faecal calprotectin excretion (median 101 mg; 95% CI 45-168 mg; normal <11 mg; r=0.80) and single stool calprotectin concentrations (median 118 mg/l; 95% CI 36-175 mg/l; normal <10 mg/l; r=0.70) in patients with Crohn's disease. The cross sectional study showed a sensitivity of 96% for calprotectin in discriminating between normal subjects (2 mg/l; 95% CI 2-3 mg/l) and those with Crohn's disease (91 mg/l; 95% CI 59-105 mg/l). With a cut off point of 30 mg/l faecal calprotectin has 100% sensitivity and 97% specificity in discriminating between active Crohn's disease and irritable bowel syndrome. CONCLUSION—The calprotectin method may be a useful adjuvant for discriminating between patients with Crohn's disease and irritable bowel syndrome. Keywords: inflammatory bowel disease; Crohn's disease; intestinal inflammation; irritable bowel syndrome
Full Text
The Full Text of this article is available as a PDF (195.0 KB).
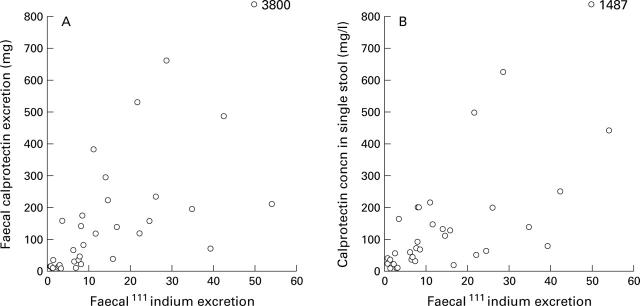
Figure 1 .
(A) Four day faecal excretion of 111indium labelled white cells (% dose) plotted against four day faecal excretion (mg) of calprotectin (r=0.80, p<0.001). (B) Four day faecal excretion of 111indium white cells plotted against single stool calprotectin concentrations (mg/l) (r=0.70, p<0.001) in patients with Crohn's disease.
Figure 2 .
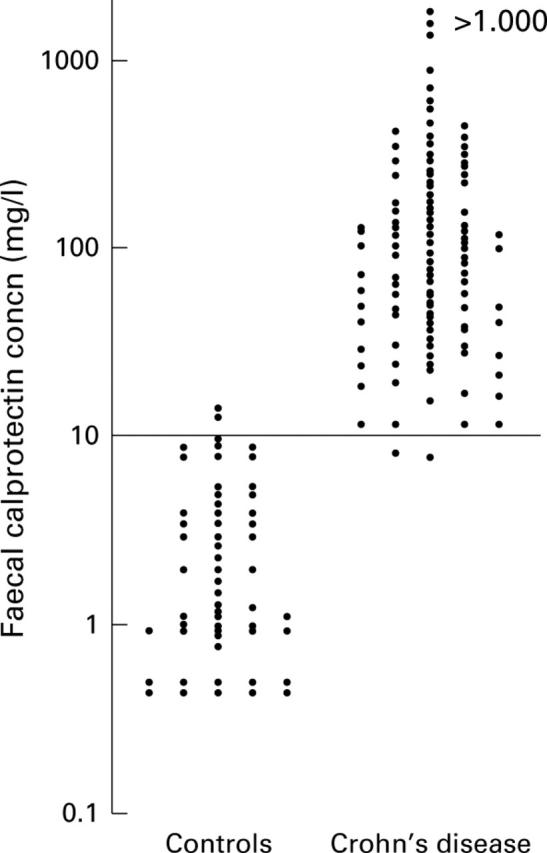
Concentrations of calprotectin (on a logarithmic scale) in faeces in 116 patients with Crohn's disease compared with controls. The horizontal line indicates the upper normal limit (+2SD) for calprotectin concentrations.
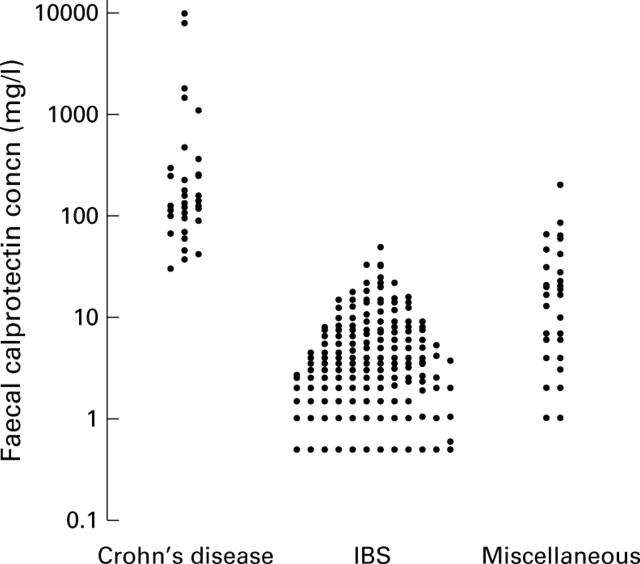
Figure 3 .
Concentrations of calprotectin (on a logarithmic scale) in faeces in patients subsequently diagnosed as having Crohn's disease, irritable bowel syndrome (IBS), and miscellaneous diseases. The upper normal limit (+2SD) for calprotectin concentrations is 10 mg/l.
Figure 4 .
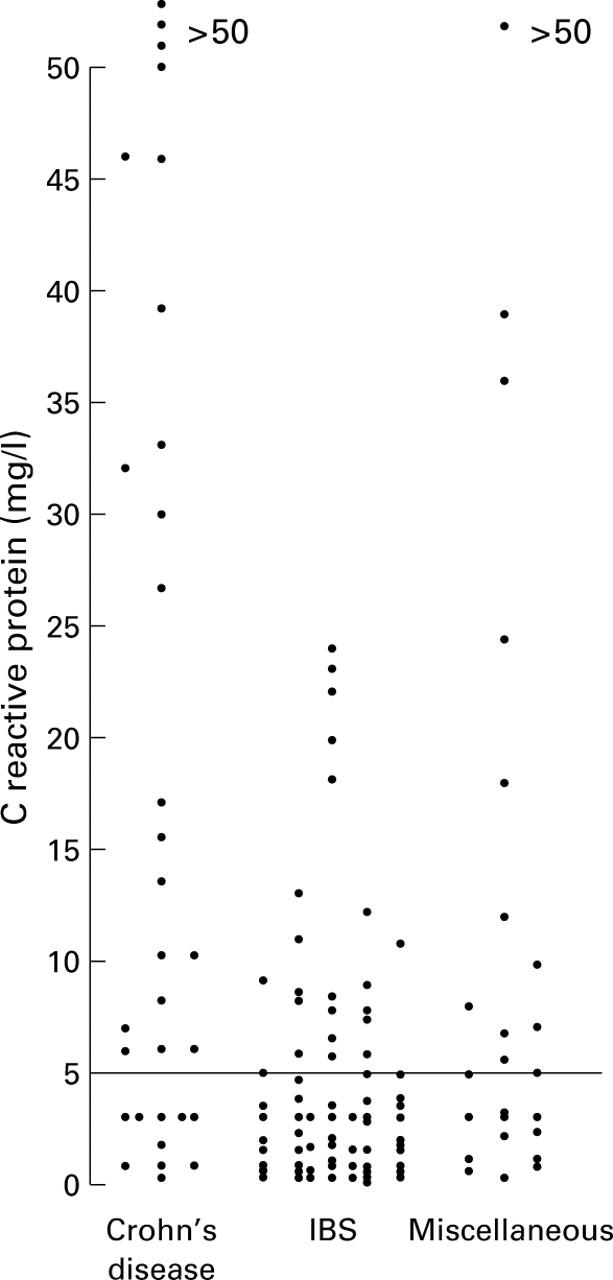
Serum C reactive protein levels in patients subsequently diagnosed as having Crohn's disease, irritable bowel syndrome (IBS), and miscellaneous disease. The upper limit of normal, which had previously been established at the Department of Immunology, King's College Hospital, for C reactive protein is 5 mg/l.
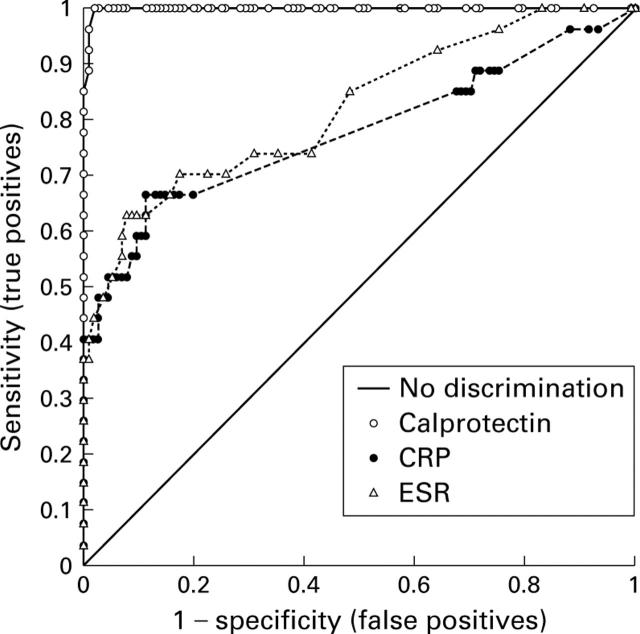
Figure 5 .
Receiver operating characteristic analysis of the ability of calprotectin, C reactive protein (CRP), and erythrocyte sedimentation rate (ESR) to discriminate between patients with Crohn's disease and the irritable bowel syndrome. The unbroken line ("no discrimination") indicates values that have no discriminatory value. Note that on the vertical axis, the scale is from no (0) to complete (1 or 100%) sensitivity. The horizontal axis is a reciprocal scale (1−specificity). The optimum performance of a test is determined either as the highest sum of the specificity and sensitivity or at an acceptable level of sensitivity for the given disease. A cut off value of 30 mg/l for faecal calprotectin gives 100% sensitivity and 97% specificity for discriminating between patients with Crohn's disease and the irritable bowel syndrome.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adeyemi E. O., Hodgson H. J. Faecal elastase reflects disease activity in active ulcerative colitis. Scand J Gastroenterol. 1992;27(2):139–142. doi: 10.3109/00365529209165434. [DOI] [PubMed] [Google Scholar]
- Best W. R., Becktel J. M., Singleton J. W., Kern F., Jr Development of a Crohn's disease activity index. National Cooperative Crohn's Disease Study. Gastroenterology. 1976 Mar;70(3):439–444. [PubMed] [Google Scholar]
- Best W. R., Becktel J. M., Singleton J. W. Rederived values of the eight coefficients of the Crohn's Disease Activity Index (CDAI). Gastroenterology. 1979 Oct;77(4 Pt 2):843–846. [PubMed] [Google Scholar]
- Bjarnason I., Hayllar J., MacPherson A. J., Russell A. S. Side effects of nonsteroidal anti-inflammatory drugs on the small and large intestine in humans. Gastroenterology. 1993 Jun;104(6):1832–1847. doi: 10.1016/0016-5085(93)90667-2. [DOI] [PubMed] [Google Scholar]
- Bjarnason I., MacPherson A., Hollander D. Intestinal permeability: an overview. Gastroenterology. 1995 May;108(5):1566–1581. doi: 10.1016/0016-5085(95)90708-4. [DOI] [PubMed] [Google Scholar]
- Bjarnason I., Sharpstone D. R., Francis N., Marker A., Taylor C., Barrett M., Macpherson A., Baldwin C., Menzies I. S., Crane R. C. Intestinal inflammation, ileal structure and function in HIV. AIDS. 1996 Oct;10(12):1385–1391. doi: 10.1097/00002030-199610000-00011. [DOI] [PubMed] [Google Scholar]
- Braegger C. P., Nicholls S., Murch S. H., Stephens S., MacDonald T. T. Tumour necrosis factor alpha in stool as a marker of intestinal inflammation. Lancet. 1992 Jan 11;339(8785):89–91. doi: 10.1016/0140-6736(92)90999-j. [DOI] [PubMed] [Google Scholar]
- Brooke B. N. Index of Crohn's disease activity. Lancet. 1980 Mar 29;1(8170):711–711. [PubMed] [Google Scholar]
- Choudari C. P., O'Mahony S., Brydon G., Mwantembe O., Ferguson A. Gut lavage fluid protein concentrations: objective measures of disease activity in inflammatory bowel disease. Gastroenterology. 1993 Apr;104(4):1064–1071. doi: 10.1016/0016-5085(93)90275-h. [DOI] [PubMed] [Google Scholar]
- Crama-Bohbouth G., Pena A. S., Biemond I., Verspaget H. W., Blok D., Arndt J. W., Weterman I. T., Pauwels E. K., Lamers C. B. Are activity indices helpful in assessing active intestinal inflammation in Crohn's disease? Gut. 1989 Sep;30(9):1236–1240. doi: 10.1136/gut.30.9.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drossman D. A., Whitehead W. E., Camilleri M. Irritable bowel syndrome: a technical review for practice guideline development. Gastroenterology. 1997 Jun;112(6):2120–2137. doi: 10.1053/gast.1997.v112.agast972120. [DOI] [PubMed] [Google Scholar]
- Fagan E. A., Dyck R. F., Maton P. N., Hodgson H. J., Chadwick V. S., Petrie A., Pepys M. B. Serum levels of C-reactive protein in Crohn's disease and ulcerative colitis. Eur J Clin Invest. 1982 Aug;12(4):351–359. doi: 10.1111/j.1365-2362.1982.tb02244.x. [DOI] [PubMed] [Google Scholar]
- Grohmann G. S., Glass R. I., Pereira H. G., Monroe S. S., Hightower A. W., Weber R., Bryan R. T. Enteric viruses and diarrhea in HIV-infected patients. Enteric Opportunistic Infections Working Group. N Engl J Med. 1993 Jul 1;329(1):14–20. doi: 10.1056/NEJM199307013290103. [DOI] [PubMed] [Google Scholar]
- Guerrant R. L., Araujo V., Soares E., Kotloff K., Lima A. A., Cooper W. H., Lee A. G. Measurement of fecal lactoferrin as a marker of fecal leukocytes. J Clin Microbiol. 1992 May;30(5):1238–1242. doi: 10.1128/jcm.30.5.1238-1242.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris M. S. Irritable bowel syndrome. A cost-effective approach for primary care physicians. Postgrad Med. 1997 Mar;101(3):215-6, 219-20, 223-6. doi: 10.3810/pgm.1997.03.184. [DOI] [PubMed] [Google Scholar]
- Harvey R. F., Bradshaw J. M. A simple index of Crohn's-disease activity. Lancet. 1980 Mar 8;1(8167):514–514. doi: 10.1016/s0140-6736(80)92767-1. [DOI] [PubMed] [Google Scholar]
- Henderson A. R. Assessing test accuracy and its clinical consequences: a primer for receiver operating characteristic curve analysis. Ann Clin Biochem. 1993 Nov;30(Pt 6):521–539. doi: 10.1177/000456329303000601. [DOI] [PubMed] [Google Scholar]
- Kordossis T., Joseph A. E., Gane J. N., Bridges C. E., Griffin G. E. Fecal leukocytosis, indium-111-labelled autologous polymorphonuclear leukocyte abdominal scanning, and quantitative fecal indium-111 excretion in acute gastroenteritis and enteropathogen carriage. Dig Dis Sci. 1988 Nov;33(11):1383–1390. doi: 10.1007/BF01536992. [DOI] [PubMed] [Google Scholar]
- Lynn R. B., Friedman L. S. Irritable bowel syndrome. N Engl J Med. 1993 Dec 23;329(26):1940–1945. doi: 10.1056/NEJM199312233292608. [DOI] [PubMed] [Google Scholar]
- Löser C., Möllgaard A., Fölsch U. R. Faecal elastase 1: a novel, highly sensitive, and specific tubeless pancreatic function test. Gut. 1996 Oct;39(4):580–586. doi: 10.1136/gut.39.4.580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malchow H., Ewe K., Brandes J. W., Goebell H., Ehms H., Sommer H., Jesdinsky H. European Cooperative Crohn's Disease Study (ECCDS): results of drug treatment. Gastroenterology. 1984 Feb;86(2):249–266. [PubMed] [Google Scholar]
- Mazlam M. Z., Hodgson H. J. Why measure C reactive protein? Gut. 1994 Jan;35(1):5–7. doi: 10.1136/gut.35.1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meling T. R., Aabakken L., Røseth A., Osnes M. Faecal calprotectin shedding after short-term treatment with non-steroidal anti-inflammatory drugs. Scand J Gastroenterol. 1996 Apr;31(4):339–344. doi: 10.3109/00365529609006407. [DOI] [PubMed] [Google Scholar]
- Røseth A. G., Aadland E., Jahnsen J., Raknerud N. Assessment of disease activity in ulcerative colitis by faecal calprotectin, a novel granulocyte marker protein. Digestion. 1997;58(2):176–180. doi: 10.1159/000201441. [DOI] [PubMed] [Google Scholar]
- Røseth A. G., Fagerhol M. K., Aadland E., Schjønsby H. Assessment of the neutrophil dominating protein calprotectin in feces. A methodologic study. Scand J Gastroenterol. 1992 Sep;27(9):793–798. doi: 10.3109/00365529209011186. [DOI] [PubMed] [Google Scholar]
- Røseth A. G., Kristinsson J., Fagerhol M. K., Schjønsby H., Aadland E., Nygaard K., Roald B. Faecal calprotectin: a novel test for the diagnosis of colorectal cancer? Scand J Gastroenterol. 1993 Dec;28(12):1073–1076. doi: 10.3109/00365529309098312. [DOI] [PubMed] [Google Scholar]
- Sachar D. B., Luppescu N. E., Bodian C., Shlien R. D., Fabry T. L., Gumaste V. V. Erythrocyte sedimentation as a measure of Crohn's disease activity: opposite trends in ileitis versus colitis. J Clin Gastroenterol. 1990 Dec;12(6):643–646. doi: 10.1097/00004836-199012000-00009. [DOI] [PubMed] [Google Scholar]
- Saverymuttu S. H., Camilleri M., Rees H., Lavender J. P., Hodgson H. J., Chadwick V. S. Indium 111-granulocyte scanning in the assessment of disease extent and disease activity in inflammatory bowel disease. A comparison with colonoscopy, histology, and fecal indium 111-granulocyte excretion. Gastroenterology. 1986 May;90(5 Pt 1):1121–1128. doi: 10.1016/0016-5085(86)90376-8. [DOI] [PubMed] [Google Scholar]
- Saverymuttu S. H. Clinical remission in Crohn's disease--assessment using faecal 111In granulocyte excretion. Digestion. 1986;33(2):74–79. doi: 10.1159/000199277. [DOI] [PubMed] [Google Scholar]
- Saverymuttu S. H., Maltby P., Batman P., Joseph A. E., Maxwell D. False positive localisation of indium-111 granulocytes in colonic carcinoma. Br J Radiol. 1986 Aug;59(704):773–777. doi: 10.1259/0007-1285-59-704-773. [DOI] [PubMed] [Google Scholar]
- Saverymuttu S. H., Peters A. M., Lavender J. P., Hodgson H. J., Chadwick V. S. 111Indium autologous leucocytes in inflammatory bowel disease. Gut. 1983 Apr;24(4):293–299. doi: 10.1136/gut.24.4.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saverymuttu S. H., Peters A. M., Lavender J. P., Pepys M. B., Hodgson H. J., Chadwick V. S. Quantitative fecal indium 111-labeled leukocyte excretion in the assessment of disease in Crohn's disease. Gastroenterology. 1983 Dec;85(6):1333–1339. [PubMed] [Google Scholar]
- Teahon K., Pearson M., Smith T., Bjarnason I. Alterations in nutritional status and disease activity during treatment of Crohn's disease with elemental diet. Scand J Gastroenterol. 1995 Jan;30(1):54–60. doi: 10.3109/00365529509093236. [DOI] [PubMed] [Google Scholar]
- Teahon K., Smethurst P., Pearson M., Levi A. J., Bjarnason I. The effect of elemental diet on intestinal permeability and inflammation in Crohn's disease. Gastroenterology. 1991 Jul;101(1):84–89. doi: 10.1016/0016-5085(91)90463-u. [DOI] [PubMed] [Google Scholar]
- Teahon K., Webster A. D., Price A. B., Weston J., Bjarnason I. Studies on the enteropathy associated with primary hypogammaglobulinaemia. Gut. 1994 Sep;35(9):1244–1249. doi: 10.1136/gut.35.9.1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tromm A., Tromm C. D., Hüppe D., Schwegler U., Krieg M., May B. Evaluation of different laboratory tests and activity indices reflecting the inflammatory activity of Crohn's disease. Scand J Gastroenterol. 1992 Sep;27(9):774–778. doi: 10.3109/00365529209011182. [DOI] [PubMed] [Google Scholar]
- Uchida K., Matsuse R., Tomita S., Sugi K., Saitoh O., Ohshiba S. Immunochemical detection of human lactoferrin in feces as a new marker for inflammatory gastrointestinal disorders and colon cancer. Clin Biochem. 1994 Aug;27(4):259–264. doi: 10.1016/0009-9120(94)90027-2. [DOI] [PubMed] [Google Scholar]
- van der Sluys Veer A., Brouwer J., Biemond I., Bohbouth G. E., Verspaget H. W., Lamers C. B. Fecal lysozyme in assessment of disease activity in inflammatory bowel disease. Dig Dis Sci. 1998 Mar;43(3):590–595. doi: 10.1023/a:1018823426917. [DOI] [PubMed] [Google Scholar]