Abstract
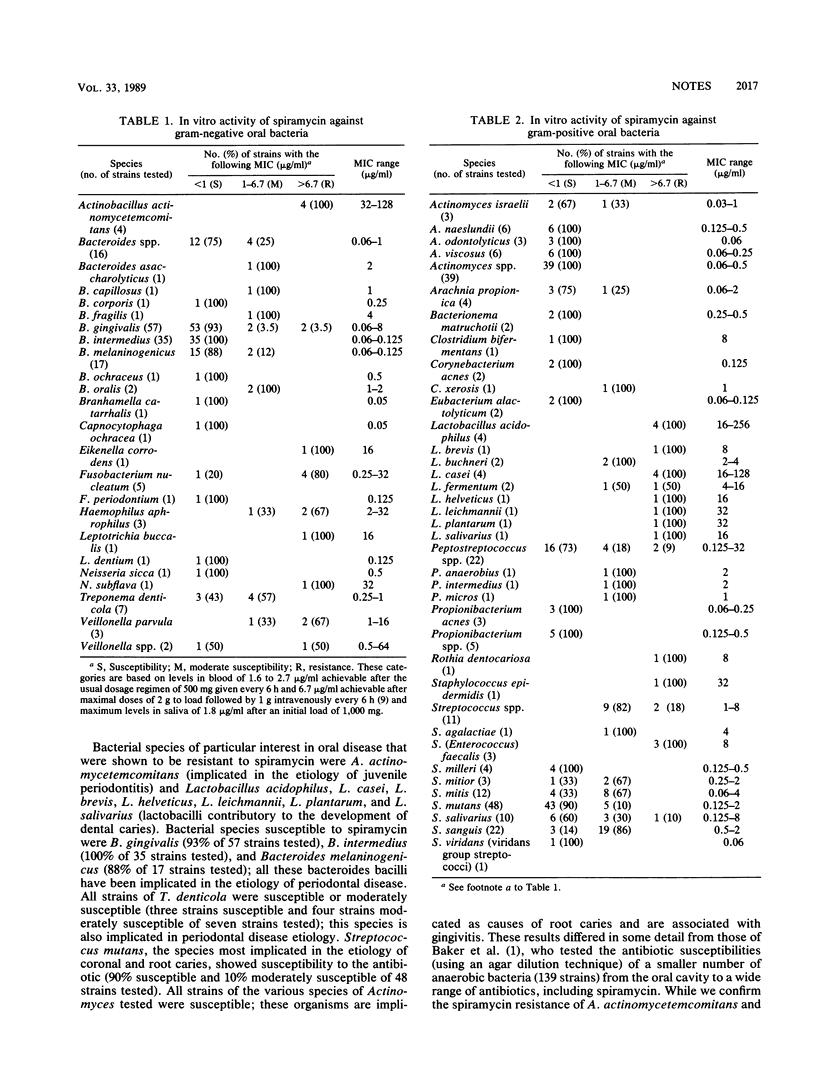
Four hundred strains of oral bacteria were tested for their susceptibility to spiramycin. Actinobacillus actinomycetemcomitans and most species of Lactobacillus were resistant to the antibiotic. All strains of cariogenic Streptococcus mutans and most strains of bacterial species implicated in adult chronic periodontitis (Bacteroides gingivalis, B. intermedius, and Treponema denticola) were susceptible to spiramycin.
Full text
PDF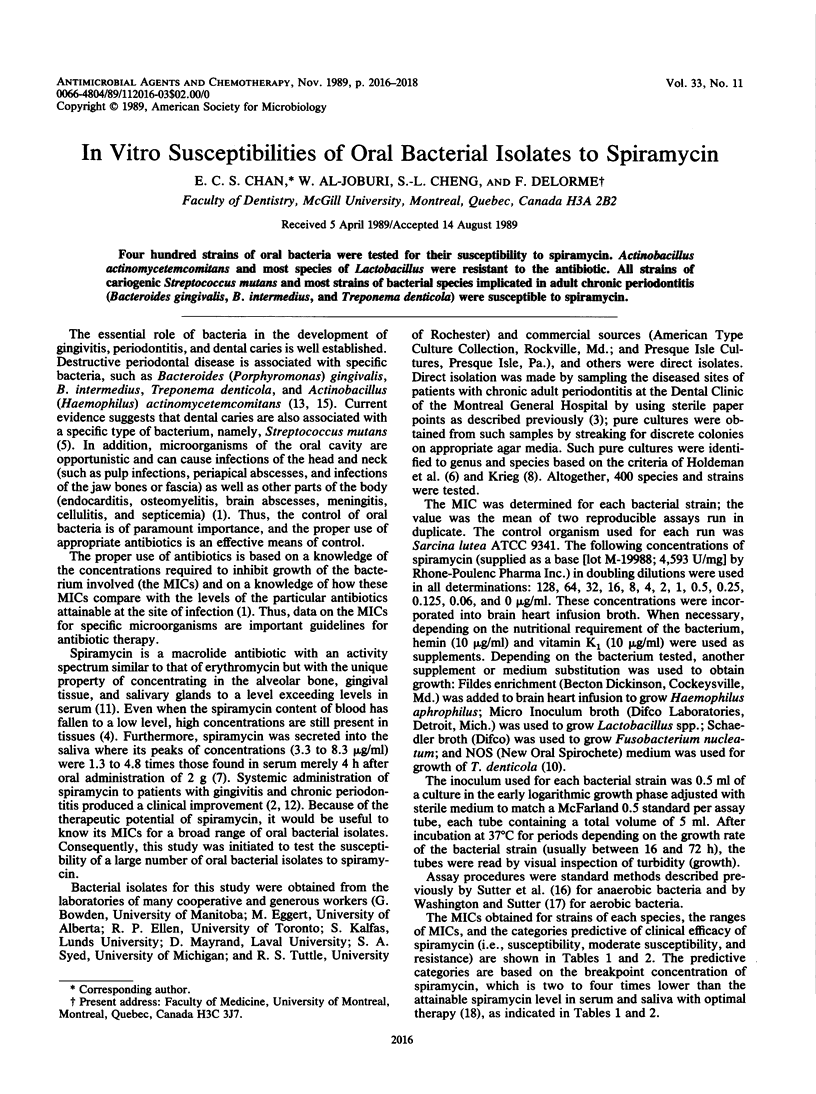

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baker P. J., Evans R. T., Slots J., Genco R. J. Antibiotic susceptibility of anaerobic bacteria from the human oral cavity. J Dent Res. 1985 Oct;64(10):1233–1244. doi: 10.1177/00220345850640101201. [DOI] [PubMed] [Google Scholar]
- Chin Quee T., Al-Joburi W., Lautar-Lemay C., Chan E. C., Iugovaz I., Bourgouin J., Delorme F. Comparison of spiramycin and tetracycline used adjunctively in the treatment of advanced chronic periodontitis. J Antimicrob Chemother. 1988 Jul;22 (Suppl B):171–177. doi: 10.1093/jac/22.supplement_b.171. [DOI] [PubMed] [Google Scholar]
- Gibbons R. J., van Houte J. Dental caries. Annu Rev Med. 1975;26:121–136. doi: 10.1146/annurev.me.26.020175.001005. [DOI] [PubMed] [Google Scholar]
- Kamme C., Kahlmeter G., Melander A. Evaluation of spiramycin as a therapeutic agent for elimination of nasopharyngeal pathogens. Possible use of spiramycin for middle ear infections and for gonococcal and meningococcal nasopharyngeal carriage. Scand J Infect Dis. 1978;10(2):135–142. doi: 10.3109/inf.1978.10.issue-2.07. [DOI] [PubMed] [Google Scholar]
- Leschine S. B., Canale-Parola E. Rifampin as a selective agent for isolation of oral spirochetes. J Clin Microbiol. 1980 Dec;12(6):792–795. doi: 10.1128/jcm.12.6.792-795.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung F. C., Gardner J. M., Paor W. S., Yankell S. L. Spiramycin excretion in animals. II. Repeated oral doses in rats. J Dent Res. 1972 May-Jun;51(3):712–715. doi: 10.1177/00220345720510030401. [DOI] [PubMed] [Google Scholar]
- Mills W. H., Thompson G. W., Beagrie G. S. Clinical evaluation of spiramycin and erythromycin in control of periodontal disease. J Clin Periodontol. 1979 Oct;6(5):308–316. doi: 10.1111/j.1600-051x.1979.tb01932.x. [DOI] [PubMed] [Google Scholar]
- Moore W. E. Microbiology of periodontal disease. J Periodontal Res. 1987 Sep;22(5):335–341. doi: 10.1111/j.1600-0765.1987.tb01595.x. [DOI] [PubMed] [Google Scholar]
- Mouton C., Dextraze L., Mayrand D. Sensibilité au métronidazole, à la spiramycine et à leur association de bactéries à potentiel parodontopathique. J Biol Buccale. 1984 Mar;12(1):17–26. [PubMed] [Google Scholar]
- Quee T. C., Chan E. C., Clark C., Lautar-Lemay C., Bergeron M. J., Bourgouin J., Stamm J. The role of adjunctive Rodogyl therapy in the treatment of advanced periodontal disease. A longitudinal clinical and microbiologic study. J Periodontol. 1987 Sep;58(9):594–601. doi: 10.1902/jop.1987.58.9.594. [DOI] [PubMed] [Google Scholar]
- Slots J. Bacterial specificity in adult periodontitis. A summary of recent work. J Clin Periodontol. 1986 Nov;13(10):912–917. doi: 10.1111/j.1600-051x.1986.tb01426.x. [DOI] [PubMed] [Google Scholar]
- Witebsky F. G., Maclowry J. D., French S. S. Broth dilution minimum inhibitory concentrations: rationale for use of selected antimicrobial concentrations. J Clin Microbiol. 1979 May;9(5):589–595. doi: 10.1128/jcm.9.5.589-595.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]



