Abstract
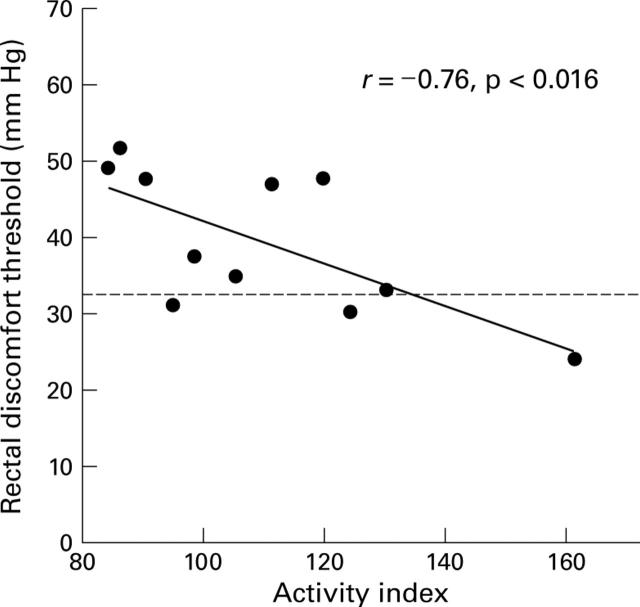
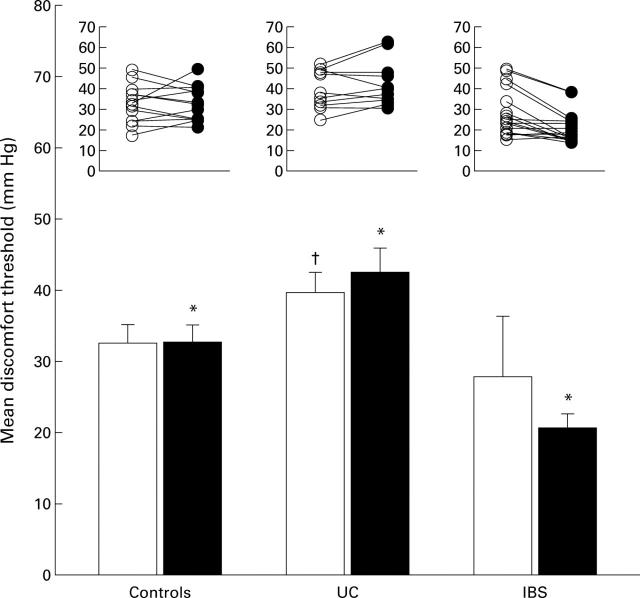
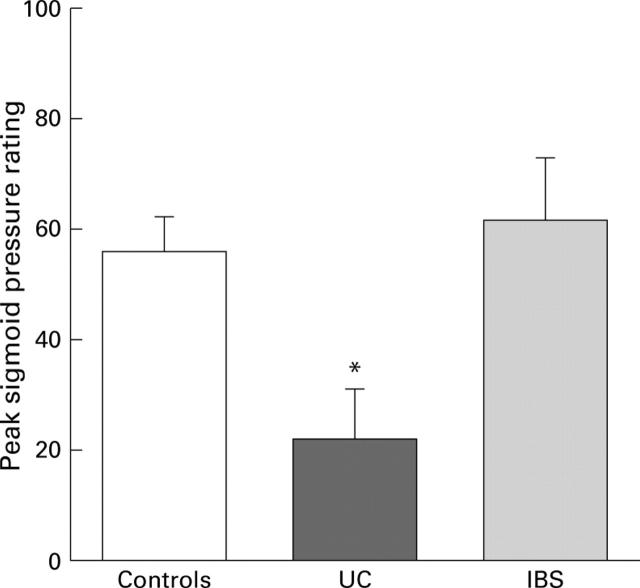
BACKGROUND AND AIMS—Enhanced visceral sensitivity following a transient inflammatory process in the gut has been postulated as an aetiological mechanism of irritable bowel syndrome (IBS). In this study we compared perceptual responses to rectosigmoid distension in patients with mild chronic inflammation of the rectum (ulcerative colitis (UC)) and patients without mucosal inflammation (IBS) to determine if chronic low grade mucosal inflammation may be a plausible explanation for rectosigmoid hypersensitivity reported in both IBS and UC patients. METHODS—UC disease activity was quantified using activity index scores. Perception thresholds for discomfort during rectosigmoid distension were compared between 11 UC patients with quiescent or mild disease activity, 18 IBS patients, and 13 healthy controls. RESULTS—Although UC activity index scores negatively correlated with perceptual thresholds for discomfort (r=−0.76, p=0.016), UC patients had higher discomfort thresholds compared with IBS patients and controls before (p=0.02) and after (p<0.001) a noxious sigmoid conditioning stimulus. CONCLUSIONS—Rectal perception was attenuated in UC but enhanced in IBS. In chronic mild inflammation, activation of antinociceptive mechanisms may prevent the development of visceral hyperalgesia. Low grade mucosal inflammation alone is unlikely to be responsible for symptoms in functional gastrointestinal disorders. Keywords: ulcerative colitis; irritable bowel syndrome; abdominal pain
Full Text
The Full Text of this article is available as a PDF (171.3 KB).
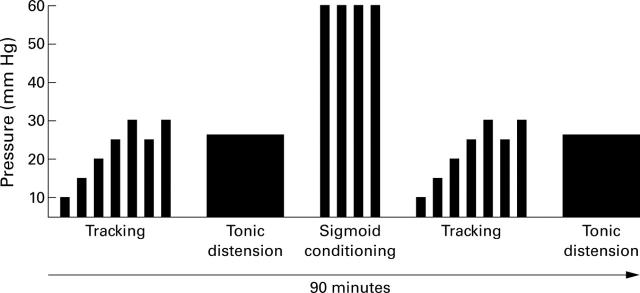
Figure 1 .
Sequence of rectal and sigmoid distension paradigms. Rectal threshold tracking and tonic distension paradigms were performed before and after the sigmoid conditioning stimulus. This illustration does not represent the actual number of distensions given.
Figure 2 .
Correlation of ulcerative colitis activity index and rectal discomfort thresholds. Broken line indicates mean rectal discomfort threshold in normal controls.
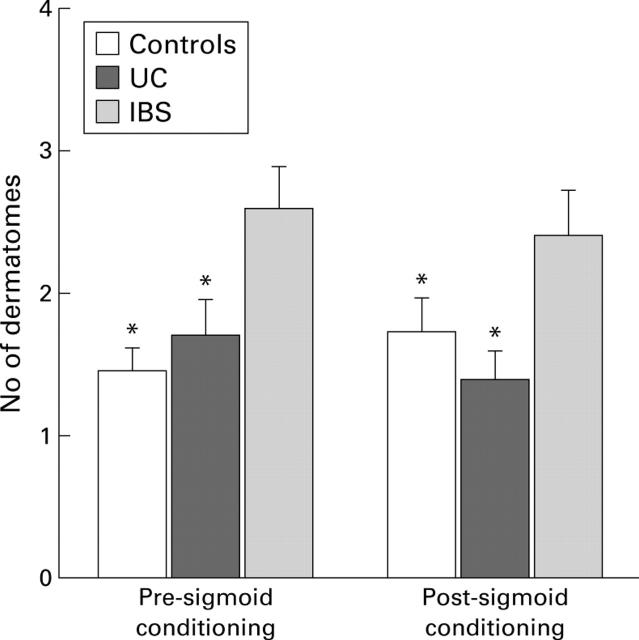
Figure 3 .
Rectal discomfort thresholds in normal controls, and in patients with ulcerative colitis (UC) and inflammatory bowel disease (IBS) before (open columns) and after (filled columns) noxious sigmoid stimulus. (Bottom) Mean rectal discomfort thresholds are shown; *significant differences compared with the two other groups (p<0.05); †significant difference compared with IBS group. (Top) Individual rectal discomfort thresholds. In this and subsequent figures, values are mean (SEM).
Figure 4 .
Mean peak sensory ratings for perception of pressure during the initial pressure pulse of the noxious sigmoid stimulus in normal subjects, and in patients with ulcerative colitis (UC) and inflammatory bowel disease (IBS). *Significant difference compared with the two other groups (p<0.05).
Figure 5 .
Viscerosomatic referral areas to which healthy subjects and patients with ulcerative colitis (UC) and inflammatory bowel disease (IBS) referred their sensations in response to the tonic rectal stimulus before (left) and after (right) noxious sigmoid stimulus. *Significant difference compared with patients with IBS (p<0.05).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bernstein C. N., Niazi N., Robert M., Mertz H., Kodner A., Munakata J., Naliboff B., Mayer E. A. Rectal afferent function in patients with inflammatory and functional intestinal disorders. Pain. 1996 Aug;66(2-3):151–161. doi: 10.1016/0304-3959(96)03062-x. [DOI] [PubMed] [Google Scholar]
- Bouchier I. A., Pennington C. R. Serum bile acids in hepatobiliary disease. Gut. 1978 Jun;19(6):492–496. doi: 10.1136/gut.19.6.492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CHAUDHARY N. A., TRUELOVE S. C. The irritable colon syndrome. A study of the clinical features, predisposing causes, and prognosis in 130 cases. Q J Med. 1962 Jul;31:307–322. [PubMed] [Google Scholar]
- Cook I. J., van Eeden A., Collins S. M. Patients with irritable bowel syndrome have greater pain tolerance than normal subjects. Gastroenterology. 1987 Oct;93(4):727–733. doi: 10.1016/0016-5085(87)90434-3. [DOI] [PubMed] [Google Scholar]
- Coutinho S. V., Meller S. T., Gebhart G. F. Intracolonic zymosan produces visceral hyperalgesia in the rat that is mediated by spinal NMDA and non-NMDA receptors. Brain Res. 1996 Oct 14;736(1-2):7–15. doi: 10.1016/0006-8993(96)00661-0. [DOI] [PubMed] [Google Scholar]
- Denis P., Colin R., Galmiche J. P., Geffroy Y., Hecketsweiler P., Lefrancois R., Pasquis P. Elastic properties of the rectal wall in normal adults and in the patients with ulcerative colitis. Gastroenterology. 1979 Jul;77(1):45–48. [PubMed] [Google Scholar]
- Fass R., Naliboff B., Higa L., Johnson C., Kodner A., Munakata J., Ngo J., Mayer E. A. Differential effect of long-term esophageal acid exposure on mechanosensitivity and chemosensitivity in humans. Gastroenterology. 1998 Dec;115(6):1363–1373. doi: 10.1016/s0016-5085(98)70014-9. [DOI] [PubMed] [Google Scholar]
- Garrison D. W., Chandler M. J., Foreman R. D. Viscerosomatic convergence onto feline spinal neurons from esophagus, heart and somatic fields: effects of inflammation. Pain. 1992 Jun;49(3):373–382. doi: 10.1016/0304-3959(92)90245-7. [DOI] [PubMed] [Google Scholar]
- Goldhill J., Pichat P., Roome N., Angel I., Arbilla S. Effect of mizolastine on visceral sensory afferent sensitivity and inflammation during experimental colitis. Arzneimittelforschung. 1998 Feb;48(2):179–184. [PubMed] [Google Scholar]
- Gracely R. H., McGrath F., Dubner R. Ratio scales of sensory and affective verbal pain descriptors. Pain. 1978 Jun;5(1):5–18. doi: 10.1016/0304-3959(78)90020-9. [DOI] [PubMed] [Google Scholar]
- Gwee K. A., Graham J. C., McKendrick M. W., Collins S. M., Marshall J. S., Walters S. J., Read N. W. Psychometric scores and persistence of irritable bowel after infectious diarrhoea. Lancet. 1996 Jan 20;347(8995):150–153. doi: 10.1016/s0140-6736(96)90341-4. [DOI] [PubMed] [Google Scholar]
- Gwee K. A., Leong Y. L., Graham C., McKendrick M. W., Collins S. M., Walters S. J., Underwood J. E., Read N. W. The role of psychological and biological factors in postinfective gut dysfunction. Gut. 1999 Mar;44(3):400–406. doi: 10.1136/gut.44.3.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Julia V., Mezzasalma T., Buéno L. Influence of bradykinin in gastrointestinal disorders and visceral pain induced by acute or chronic inflammation in rats. Dig Dis Sci. 1995 Sep;40(9):1913–1921. doi: 10.1007/BF02208656. [DOI] [PubMed] [Google Scholar]
- Lembo T., Munakata J., Mertz H., Niazi N., Kodner A., Nikas V., Mayer E. A. Evidence for the hypersensitivity of lumbar splanchnic afferents in irritable bowel syndrome. Gastroenterology. 1994 Dec;107(6):1686–1696. doi: 10.1016/0016-5085(94)90809-5. [DOI] [PubMed] [Google Scholar]
- Loening-Baucke V., Metcalf A. M., Shirazi S. Anorectal manometry in active and quiescent ulcerative colitis. Am J Gastroenterol. 1989 Aug;84(8):892–897. [PubMed] [Google Scholar]
- Loening-Baucke V., Metcalf A. M., Shirazi S. Anorectal manometry in active and quiescent ulcerative colitis. Am J Gastroenterol. 1989 Aug;84(8):892–897. [PubMed] [Google Scholar]
- Manning A. P., Thompson W. G., Heaton K. W., Morris A. F. Towards positive diagnosis of the irritable bowel. Br Med J. 1978 Sep 2;2(6138):653–654. doi: 10.1136/bmj.2.6138.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayer E. A., Gebhart G. F. Basic and clinical aspects of visceral hyperalgesia. Gastroenterology. 1994 Jul;107(1):271–293. doi: 10.1016/0016-5085(94)90086-8. [DOI] [PubMed] [Google Scholar]
- Mertz H., Fullerton S., Naliboff B., Mayer E. A. Symptoms and visceral perception in severe functional and organic dyspepsia. Gut. 1998 Jun;42(6):814–822. doi: 10.1136/gut.42.6.814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mertz H., Naliboff B., Munakata J., Niazi N., Mayer E. A. Altered rectal perception is a biological marker of patients with irritable bowel syndrome. Gastroenterology. 1995 Jul;109(1):40–52. doi: 10.1016/0016-5085(95)90267-8. [DOI] [PubMed] [Google Scholar]
- Miampamba M., Chéry-Croze S., Gorry F., Berger F., Chayvialle J. A. Inflammation of the colonic wall induced by formalin as a model of acute visceral pain. Pain. 1994 Jun;57(3):327–334. doi: 10.1016/0304-3959(94)90008-6. [DOI] [PubMed] [Google Scholar]
- Morteau O., Julia V., Eeckhout C., Bueno L. Influence of 5-HT3 receptor antagonists in visceromotor and nociceptive responses to rectal distension before and during experimental colitis in rats. Fundam Clin Pharmacol. 1994;8(6):553–562. doi: 10.1111/j.1472-8206.1994.tb00837.x. [DOI] [PubMed] [Google Scholar]
- Munakata J., Naliboff B., Harraf F., Kodner A., Lembo T., Chang L., Silverman D. H., Mayer E. A. Repetitive sigmoid stimulation induces rectal hyperalgesia in patients with irritable bowel syndrome. Gastroenterology. 1997 Jan;112(1):55–63. doi: 10.1016/s0016-5085(97)70219-1. [DOI] [PubMed] [Google Scholar]
- Naliboff B. D., Munakata J., Fullerton S., Gracely R. H., Kodner A., Harraf F., Mayer E. A. Evidence for two distinct perceptual alterations in irritable bowel syndrome. Gut. 1997 Oct;41(4):505–512. doi: 10.1136/gut.41.4.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ness T. J., Gebhart G. F. Visceral pain: a review of experimental studies. Pain. 1990 May;41(2):167–234. doi: 10.1016/0304-3959(90)90021-5. [DOI] [PubMed] [Google Scholar]
- Rao S. S., Read N. W., Davison P. A., Bannister J. J., Holdsworth C. D. Anorectal sensitivity and responses to rectal distention in patients with ulcerative colitis. Gastroenterology. 1987 Dec;93(6):1270–1275. doi: 10.1016/0016-5085(87)90255-1. [DOI] [PubMed] [Google Scholar]
- Sengupta J. N., Snider A., Su X., Gebhart G. F. Effects of kappa opioids in the inflamed rat colon. Pain. 1999 Feb;79(2-3):175–185. doi: 10.1016/s0304-3959(98)00175-4. [DOI] [PubMed] [Google Scholar]
- Seo M., Okada M., Yao T., Okabe N., Maeda K., Oh K. Evaluation of disease activity in patients with moderately active ulcerative colitis: comparisons between a new activity index and Truelove and Witts' classification. Am J Gastroenterol. 1995 Oct;90(10):1759–1763. [PubMed] [Google Scholar]
- Stein C. The control of pain in peripheral tissue by opioids. N Engl J Med. 1995 Jun 22;332(25):1685–1690. doi: 10.1056/NEJM199506223322506. [DOI] [PubMed] [Google Scholar]
- Sutherland L. R., Martin F., Greer S., Robinson M., Greenberger N., Saibil F., Martin T., Sparr J., Prokipchuk E., Borgen L. 5-Aminosalicylic acid enema in the treatment of distal ulcerative colitis, proctosigmoiditis, and proctitis. Gastroenterology. 1987 Jun;92(6):1894–1898. doi: 10.1016/0016-5085(87)90621-4. [DOI] [PubMed] [Google Scholar]
- TRUELOVE S. C., WITTS L. J. Cortisone in ulcerative colitis; final report on a therapeutic trial. Br Med J. 1955 Oct 29;2(4947):1041–1048. doi: 10.1136/bmj.2.4947.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]